Poor Kids With Cancer Relapse Earlier Than Rich Children
Nearly one in three families aren’t able to meet their own basic needs while a child is in chemotherapy.
Poverty is bad for children’s health. The evidence is everywhere. Babies from poor families are often born at lower weights, then suffer higher rates of respiratory infections, gastrointestinal sickness, anemia, nutritional deficiencies, ear disease, and wheezing illnesses. They fail to thrive at higher rates than their wealthier peers.
Poor children are more likely to be obese, and they’re more likely to have higher levels of lead in their blood. They get more cavities and they experience higher rates of vision loss.
“Virtually all aspects of health are worse among children living in poverty than among children from affluent families,” wrote the pediatrician Richard Reading in the medical journal, Archives of Disease in Childhood.
Even in settings where children from different economic backgrounds receive the same medical care, like treatment for leukemia, the poorer children often have worse outcomes.
At the same time, survival rates for most pediatric cancer patients have improved significantly. Though childhood cancer is rare overall, acute lymphoblastic leukemia is among the most common cancer diagnoses for young patients. In the 1960s, the vast majority of children with acute lymphoblastic leukemia didn’t survive; but the five-year survival rate went from less than 10 percent half-a-century ago to higher than 80 percent today.
“We’re often held up as the success story in modern medicine,” said Kira Bona, a pediatric oncologist at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. “But the flip side is that 20 percent of kids will die, and that is far too many.”
Bona is part of a team of researchers who assessed a decade’s worth of data showing how children with leukemia from different income areas fared after they went into remission. What they found was troubling. While the overall rates of relapse were roughly the same for all the patients, the children from high-poverty areas were much more likely to relapse early—less than 36 months into remission—and earlier relapses are linked with worse outcomes overall. “If you relapse early, it’s significantly harder to cure you,” Bona told me. “The difference is pretty dramatic.”
She and her colleagues found early relapses occurred among 92 percent of poor kids compared with 48 percent of wealthier children. Their work was published in the journal Pediatric Blood & Cancer in February. Now, doctors are working to figure out why this disparity exists, and what they can do about it.
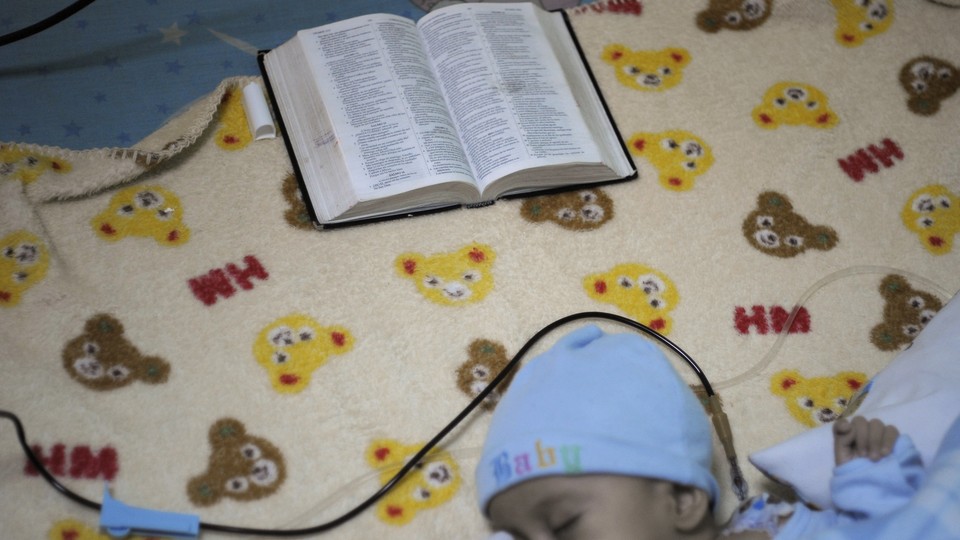
One hypothesis looks at the extent to which underlying health problems—which are already more likely among poor people—play a role. “Perhaps poor children, at the time they’re diagnosed, have worse underlying health so they’re more vulnerable to the toxicities of chemotherapy,” she said. Another possibility is that low-income families have difficulty adhering to the schedule for administering oral chemotherapy at home, perhaps in some cases because they don’t have enough money to pay electricity bills—and therefore can’t keep their children’s medicines cold.
“When your financial situation is causing you to have your heat shut off—and your child has cancer, and they’re immune compromised—it’s a very dangerous situation,” said Carla Tardif, the CEO of the Family Reach Foundation, a grant-providing nonprofit that helps families cope with the financial burden of a cancer diagnosis. “Some of these medicines have to be taken with food. Healthy food for a sick child is critical. Many families cars have been repossessed. We have families taking a couple buses and trains just to get treatment.”
“It is a reality of cancer that people don’t talk about,” she added. “There are folks that enter cancer already in financial dire straits, but in a lot of cases we see it’s the cancer diagnosis that’s causing the financial devastation.”
Even for families with health insurance, out-of-pocket costs associated with cancer treatment can be anywhere between $10,000 to $35,000 or more, depending on the illness, according to several studies. Yet the median annual income for families in the United States is $52,000 annually. “That’s the math,” Tardif said. “That’s why you’re in financial trouble, not because you did anything wrong.”
That’s also why many cancer patients—more than one in five, Tardif told me—end up cutting their medication in half to make it last longer. “Nobody prepares for cancer,” Tardif said. “These families are in crisis. Their life has changed in an instant when they hear their child has cancer. They are very, very afraid ... And they are afraid to tell their doctor [about money problems] because they’re afraid they won’t treat them the same.”
Meanwhile, doctors are often so focused on treating a serious illness that they don’t ask families about whether they’re having trouble financially, and families may not know that many hospitals have social workers who might be able to help. There are already suggested screening questions that could make a difference. In 2011, a study published in the International Journal of Family Medicine found that asking one screening question could predict poverty the vast majority of the time. The question: “Do you ever have difficulty making ends meet at the end of the month?”
Bona says that, in addition to encouraging clinicians to ask screening questions, it’s important to give doctors and nurses the tools so that they can provide tangible help to families who need it. “There’s a huge hesitancy to discuss this topic in the exam room,” Bona said. “It’s really challenging to have a family tell you something awful and you don’t know how to fix it for them.”
In a study last year, Bona and her colleagues found that nearly one in three families aren’t able to meet their own basic needs while a child is in chemotherapy. Bona says seemingly small steps could make an enormous difference—like having health-care providers ask screening questions over time, and giving doctors and nurses resources like pre-paid grocery cards to give to families in need. More broadly, she says, doctors need to think about poverty as an issue to be integrated into their care models.
“This has value whether or not it’s linked to disease outcome,” Bona said. “It’s simply not acceptable for families to be struggling with food insecurity while their children are being treated for cancer.”


