Abstract and Introduction
Abstract
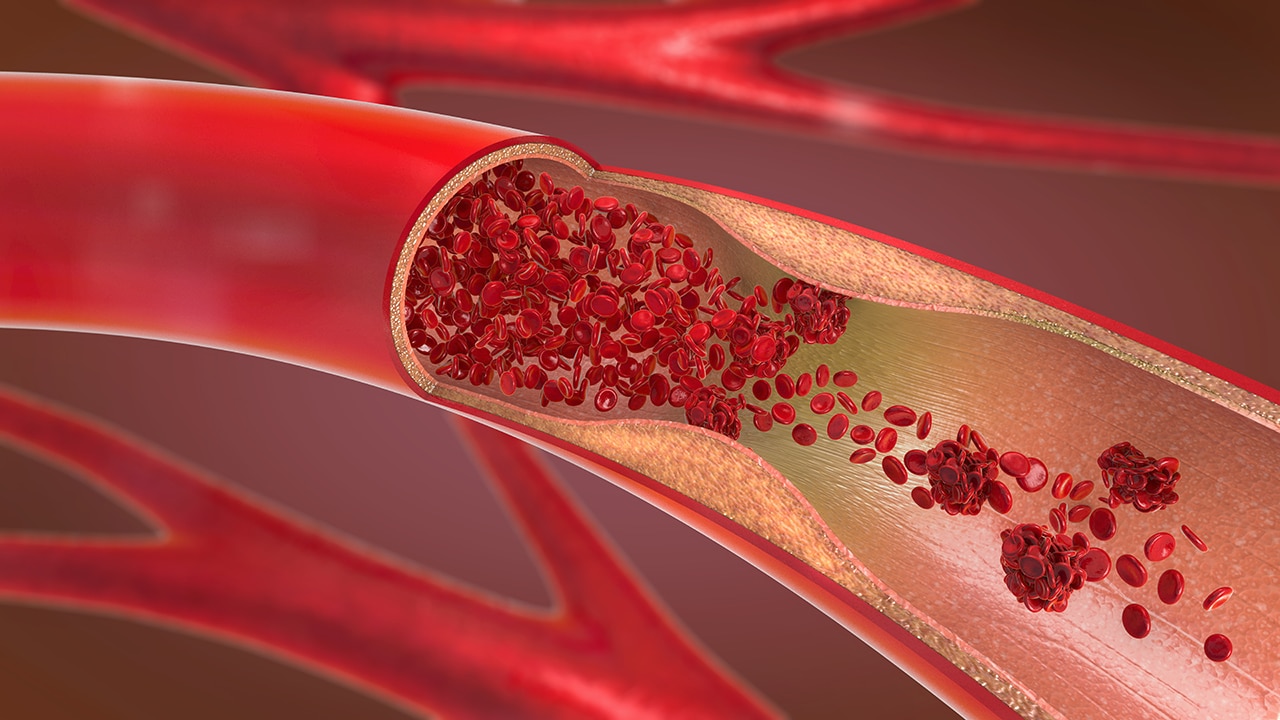
Deep vein thrombosis (DVT) is a significant health problem, leading to the hospital admission of over 250,000 Americans each year. Its most serious acute complication, namely pulmonary embolus, kills approximately 100,000 each year, and is the third most common cardiovascular related mortality after myocardial infarction and stroke. Chronic leg problems following DVT include leg heaviness, tiredness, cramping and ulceration. These are termed the post-thrombotic syndrome. The current standard therapy of anticoagulation has changed little over 50 years. It does not remove or destroy thrombus, relying instead on the bodies own fibrinolytic mechanisms to do so. DVT needs to be more accurately categorized on an anatomical basis, and for a variety of reasons, the area of most importance is the iliofemoral region. The rationale for active, rather than passive, thrombus removal relies on multiple observations that, by doing so improves luminal patency, restores valvular function and has the potential to reduce the severity of post-thrombotic syndrome. Techniques for thrombus removal include catheter-directed thrombolysis, mechanical thrombectomy and various combinations of both (pharmacomechanical catheter-directed thrombolysis). There are no direct trials comparing these different forms of treatment. Each has shown reasonable efficacy as detailed in the literature below.
Introduction
Acute deep vein thrombosis (DVT) is a major health issue causing approximately 300,000–600,000 new cases per annum in the USA.[101] Venous thromboembolism accounts for more deaths than the total combined mortality of breast cancer, road traffic accidents and AIDS combined.[101] It is the third most common cause of cardiovascular mortality after myocardial infarction and cerebral vascular accidents. Apart from the initial symptoms, which may be severe and progress to phlegmasia cerulea dolens, there is the risk of pulmonary embolic disease that can be life threatening. The chronic subsequent leg problems of leg swelling, pain, ulceration and so on are termed the 'post-thrombotic syndrome' (PTS).
Conventional management of acute DVT is based upon one trial from 1960 and several subsequent observational trials.[1–3] It has changed little over that time. This consists of immediate anticoagulation (AC) with heparin or, more recently, low-molecular-weight heparin (LMWH) followed by 3 months of oral AC. However, neither of these treatments offers significant fibrinolytic activity, relying instead on the body's own urokinase.
Acute DVT refers to symptoms less than 14 days.
Interv Cardiol. 2011;3(5):589-596. © 2011 Future Medicine Ltd.








Comments