Nineteen years ago, I was hospitalized for severe anorexia. I was in dire shape: My skin was yellow from liver failure. I was unable to stand up, walk, or bathe myself. At 5'6" tall, I weighed 58 pounds.
Had I been hospitalized today, physicians might have debated whether I met the criteria for a new, controversial condition—terminal anorexia. Not yet an official diagnosis, the term appeared in the Journal of Eating Disorders, in an article describing the deaths of three patients with "severe and enduring anorexia."
According to the authors, their prognosis was grim, but treatment was "medically futile." Instead of forcing hospitalization, the consulting physician felt the most compassionate response was to allow them to die.
They were offered palliative care, and two patients received prescriptions for Medical Aid and Dying (MAiD). One patient died after ingesting a lethal dose, the other of malnutrition before she could take the medication.
The article sparked an outcry, igniting a debate about whether right-to-die laws allow patients with anorexia to end their own lives. MAiD is now legal in eleven states, but its use for a psychiatric disorder is a legal gray area.
In most states, physicians must confirm a person has a terminal illness and less than six months to live to prescribe the lethal drugs. If adopted, terminal anorexia would open a legal pathway for people with anorexia to end their own life.

Nearly all aid-in-dying laws contain an important proviso. Physicians must confirm patients have the mental capacity to make an informed decision. Assessing capacity in a mentally ill person—an illness that, by definition, impairs mental functioning—requires careful evaluation.
But it is especially complex in anorexia, a disorder in which patients appear rational in all ways except their ability to do the one thing that could save their lives—eat.
Even at the height of my illness, I was a convincing narrator of my mental capacity. I was remarkably lucid, yet could not comprehend the risk that starvation posed to my life.
One of the most striking neurological effects of starvation is how it distorts your emotional perception of risk and reward.
I felt comfort when I was hungry, but apathetic about my failing organs. If I had not been forcibly hospitalized, I would have continued starving.
Many doctors had little hope for my recovery. My care team tried everything—psychological therapies, psychiatric drugs, and residential treatment. I was called obstinate, stubborn, intractable, and treatment-resistant. I felt hopeless and despondent, a burden to my family.
If the option for assisted dying had been available, I would have taken it.
After 16 months of state-mandated treatment, I did recover. Today, I run a nonprofit that helps people with eating disorders. I have not weighed myself or counted calories in almost twenty years.
For years, I believed I had a chronic and likely terminal disease. I was told by well-meaning medical professionals that relapse was inevitable. I met people who had cycled in and out of treatment for decades—they said anorexia never goes away.
These ideas are unscientific and misleading, eroding the sense of agency and self-efficacy you need to recover.
The notion that anorexia is a terminal disorder has no place in medicine. Anorexia is difficult to recover from, but it is a treatable condition. Even with a paucity of evidence-based treatments, most people will recover.
Anorexia has the highest mortality rate of any psychiatric disorder—but with effective treatment, up to 72 percent of patients make at least a partial recovery and nearly half recover completely.
Assisted dying laws require physicians to deem with "reasonable medical certainty" that the patient will die within six months.
But in mental illness, there are no standardized tests to determine disease progression like there are in physical illnesses like cancer. Physicians' assessments of who is terminal are almost entirely subjective, carrying life-or-death consequences.
A diagnostic term is powerful, and especially for those with psychiatric disorders, a terminal one can become a self-fulfilling prophecy. Calling treatment "futile" and death "inevitable" can itself diminish a person's capacity to make sound judgments about whether to continue living.
The creation of "terminal anorexia" will inevitably sow feelings of cynicism and hopelessness in people with a real shot at recovery.
Further, a diagnosis of terminal anorexia may gloss over widespread failures in healthcare. Many patients desperately want to recover but never receive adequate treatment.
Those with the most severe conditions are at a life-threatening disadvantage. Many facilities lack the expertise to manage their complex medical needs, and private centers rarely accept Medicaid.
When people do take the brave step of seeking help, they often receive ineffective and unproven treatments. There are no binding standards for eating disorder care. Many centers peddle treatments that look cutting edge, but even at up to $2,000 a day, are only marginally effective.
When patients fail to get better they may languish for years in relapse.
This makes the slide toward palliative care all the more chilling—the most expensive, hard-to-treat patients can be pushed toward assisted dying, while the system continues to churn out subpar care.
Instead of a new diagnosis of terminal anorexia, we need enforceable standards of treatment and more funding for eating disorder research. Most importantly, we must not abandon or lose hope in those who have been struggling to get better in a flawed system the longest.
We can respect a person's autonomy without colluding with their most despairing thoughts—the feeling their life is not valuable. I am alive today thanks to those who never gave up on me, and for that, I will always be grateful.
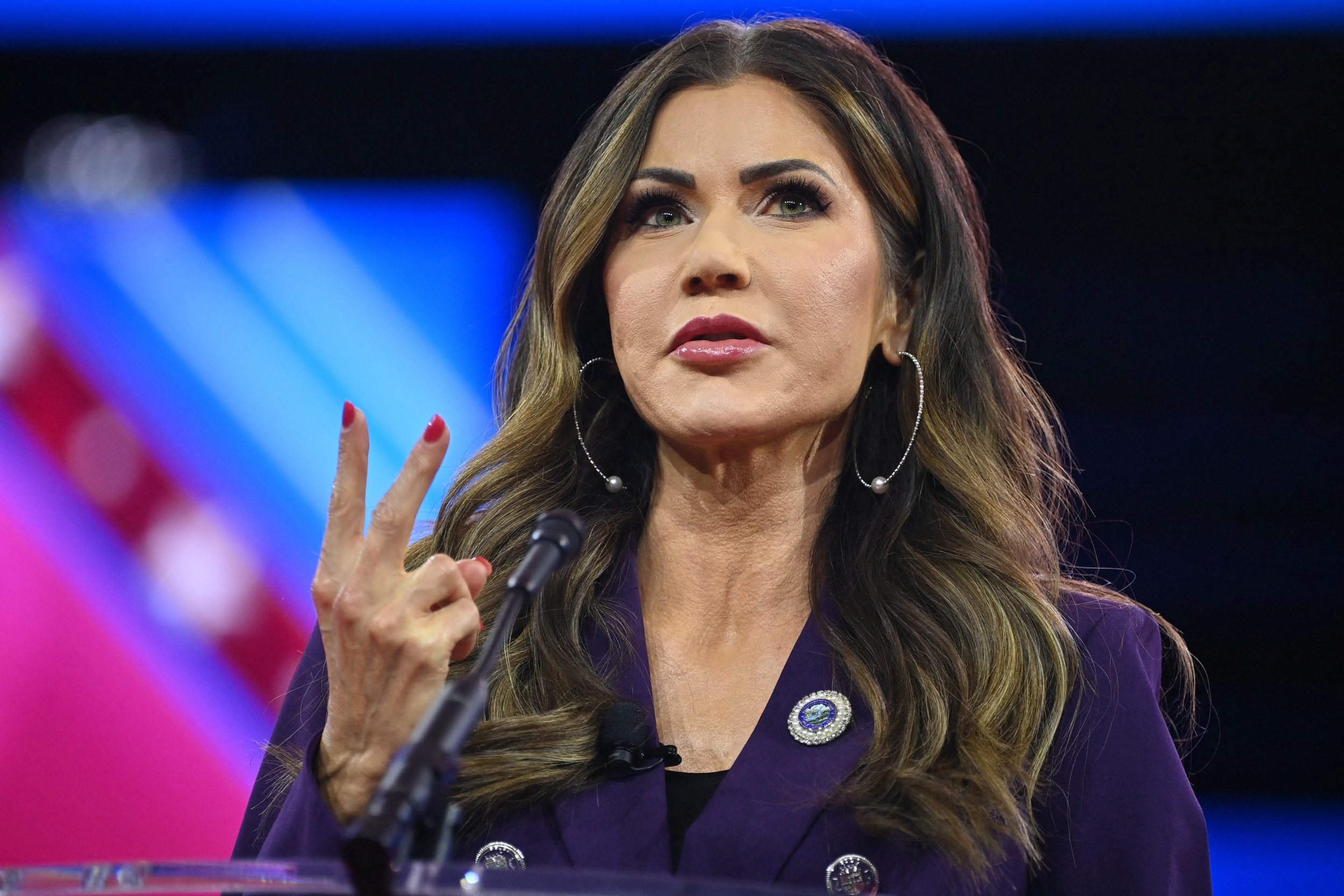
Chelsea Roff is the executive director of Eat Breathe Thrive, a nonprofit that helps people recover from eating disorders. A yoga therapist, educator, and researcher, she has spent over a decade working to develop, deliver, and conduct scientific studies on yoga programs for people with eating disorders.
All views expressed in this article are the author's own.
Do you have a unique experience or personal story to share? Email the My Turn team at myturn@newsweek.com.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Chelsea Roff is the Executive Director of Eat Breathe Thrive, a nonprofit that helps people recover from eating disorders. A ... Read more
To read how Newsweek uses AI as a newsroom tool, Click here.