Focused Physical Examination of the Infant With Suspected BPI
Brachial plexus injuries are apparent at birth or soon thereafter. A systematic examination should take place as soon as possible; the goal is to do the following:
Establish a working diagnosis
Document a baseline functional assessment
Track the evolution of symptoms and follow for the natural history of recovery
Carefully review the labor and delivery history for any of the following: maternal diabetes; fetal macrosomia; abnormal labor patterns; malpresentation, nonreassuring fetal heart pattern; mode of delivery; and difficult extraction and/or use of instrumentation. Any family history of BPI should also be noted.[19]
Any examination dependent on neurological or motor function must be interpreted in the context of the infant's gestational age, underlying clinical condition, the presence or absence of sedatives or narcotics, and the infant's state at the time of the examination. A BPI may not be readily apparent in the hypotonic infant who presents with severe perinatal depression. At-risk infants require ongoing serial evaluations.
If BPI is suspected by the nurse on admission, gentle handling is necessary to minimize the potential of further injury to the affected extremity.[20] Position the infant supine and observe his or her activity both at rest and with spontaneous movement and handling. Keep the head midline to avoid differences in upper arm movements due to head position. A quiet, full-term infant normally lies with arms adducted, elbows flexed, and moves the limbs alternately and equally. Observe all spontaneous movements for symmetry, quantity, and quality.
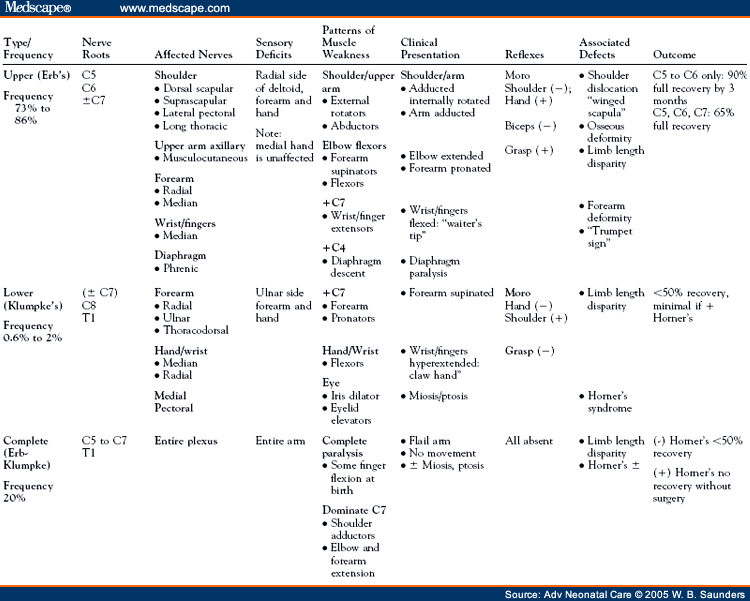
A limited examination of primitive reflexes is necessary to evaluate motor function. Assess movement in response to the Moro reflex and palmar grasp; evaluate for equality in strength and symmetry. In newborns, the tonic neck reflex should be present; it causes the extension of the arm on the same side that the head is turned to and flexion of the opposite sidethe classic fencing position.[21] Compare movements bilaterally. Although BPI is usually unilateral, bilateral injuries have been reported.[20] Asymmetric, incomplete, weak, or absent palmar, grasp, and Moro reflexes may indicate motor nerve injury.[12,13]
Evaluate gross sensory function by assessing the infant's response to touch and painful stimuli. A grimace and cry without withdrawal of the affected limb can indicate muscle paralysis.[21]
Arm weakness or paralysis is usually readily apparent. A weak or limp arm or hand, asymmetric movements, or incomplete reflexes indicate a possible brachial plexus nerve injury. If a completely limp arm with hand weakness is noted, inspect the eye on the affected side for eyelid drooping and unequal pupils. These are signs that may be indicative of Horner's syndrome.[19] Pale cool dry skin may also indicate impaired sympathetic tone.[22]
Brachial plexus injury may be associated with facial and phrenic nerve palsies.[23] Inspect the face and scalp for visible forceps marks or lacerations. Inspect the chest, neck, and upper extremities for localized bruising or edema. Unequal facial movements, which may indicate a facial palsy, are most obvious when the infant is crying. Also evaluate the infant's suck and cry. A weak suck, stridor, or a hoarse cry may indicate vocal cord paralysis and tongue weakness due to transient injury to the recurrent laryngeal and hypoglossal nerves.[24] Infants with facial palsies may also have difficulty latching and feeding.
Monitor for respiratory distress; this may present with tachypnea or asynchronous abdominal breathing often associated with diaphragmatic paralysis.[19] Palpate the neck, clavicles, shoulders, and both extremities, noting any crepitus or swelling that may indicate fractures of the humerus or clavicle, or sternocleidomastoid injury, and/or contraction. These injuries can compress the brachial plexus nerves and cause upper arm weakness.[10] Note differences in the size or length of the affected extremity. Muscle atrophy and shortened limb length at birth indicate a long-standing prenatal insult.[25] Carefully document all abnormal findings and report them immediately to the primary care provider.
After hospital discharge, ongoing serial assessments during the first weeks of life, often performed by the infant's primary care providers, is required to document the natural history of the injury.[26] Complete documentation of the findings of the initial examination are essential for comparison. Detection of individual muscle strength in infants is difficult and Results should be evaluated with caution. Examinations should focus on the following joint functions:[10]
Shoulder flexion, extension, abduction, internal and external rotation
Elbow flexion, extension, supination, pronation
Wrist, finger and thumb flexion, extension, adduction, abduction, and apposition
A key indicator of recovery is the return of biceps function. This is detected by palpable contraction and observation of extremity movement against gravity. Observe the infant in multiple positions (supine, propped seated, and prone) to detect the impact of gravity on motor strength.[26,27] Antigravity movements are induced by use of the Moro and asymmetric tonic neck reflexes to assess shoulder abduction and forward elevation, elbow flexion, and wrist and finger extension.[28]
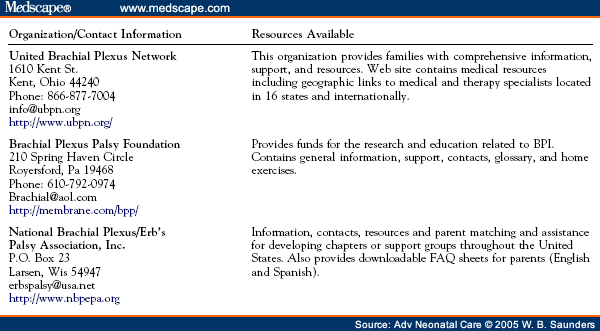
If there is not complete recovery of tone and function by the end of the first month of life, a pediatric neurologist should be consulted for further evaluation. At this stage, the diagnostic evaluation includes a more extensive assessment of motor and sensory function, determination of the level of spinal nerve injury level with a neonatal sensory dermatone map, and a motor function evaluation with a muscle-grading scale.[19] These tests require specialized education, experience, and training and are outside the scope of an initial nursery or primary care provider evaluation. Referral to a BPI specialty center is made based on the findings of these specialized examinations and is discussed later in the article.
Adv Neonatal Care. 2005;5(5):240-251. © 2005 W.B. Saunders
Although Dr. Nath does not agree with all of the concepts brought forth in these articles, he has graciously allowed the use of these excellent teaching tools to further educate the medical community on BPI.
Cite this: Part 2. Distinguishing Physical Characteristics and Management of Brachial Plexus Injuries - Medscape - Oct 01, 2005.




Comments