If you have a deep-vein thrombosis, your doctor should usually prescribe either heparin or the related drug fondaparinux (Arixtra and generic). That is often followed by warfarin (Coumadin, Jantoven, and generic). Although those medications are often referred to as blood thinners, they don't actually thin the blood. Instead, they impair the clotting process and can prevent existing clots from growing larger. But they can also cause life-threatening internal bleeding (see box below).
You probably won't receive intravenous medication for more than a few days. After that, you should usually be switched to self-injections of heparin and warfarin pills. Warfarin takes up to several days to work but once it becomes effective, you can usually stop taking heparin, though you may continue taking warfarin for several months or longer.
Warfarin is very effective but poses a risk of serious internal bleeding while you are taking it, so blood tests are required at least once a month to make sure it's continuing to work properly and that you're not at risk of bleeding. Uncontrolled bleeding caused by the drug leads to an estimated 43,000 visits to emergency rooms each year.
Some foods and beverages can reduce warfarin's effectiveness. Specifically, you should avoid eating unusually large amounts of food high in vitamin K, such as broccoli, brussel sprouts, collard greens, kale, and spinach. Also be sure to tell your doctor about any medications or dietary supplements you take, because many drugs and supplements can interact with warfarin.
Medical compression stockings are commonly used to prevent further blood clots after suffering a DVT, and after any surgery that might require bed rest. The stockings, which stretch from the foot to the knee, can help relieve pain and swelling. They're tight at the ankle and looser near the knee, to keep blood from pooling and forming a clot in the lower leg. Some people wear them for two years or longer after first having a clot.
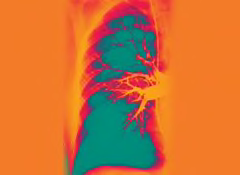
A pulmonary embolism is a medical emergency. If the clot is life-threatening, doctors in the hospital usually give the patient medications called thrombolytics, such as alteplase (Activase), to try to dissolve it. Those medications carry a risk of serious sudden internal bleeding, so they're used only in life-threatening situations. In some cases, doctors might need to thread a flexible tube, or catheter, through a vein in your groin or arm to the clot. The doctor can then try suction to remove the clot or deliver thrombolytic medication through the catheter to dissolve it. In rarer cases, doctors might have to perform surgery to remove the clot.
After treatment for pulmonary embolism, you'll probably have to take the same drugs that people take after a deep-vein thrombosis.