Abstract and Introduction
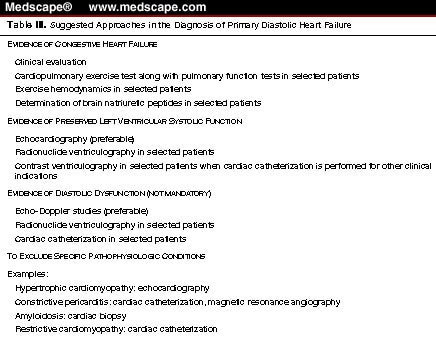
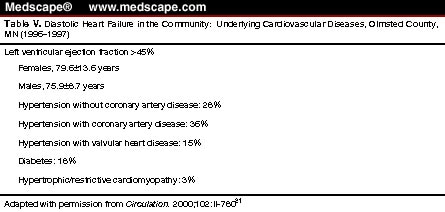
Diastolic heart failure is defined clinically when signs and symptoms of heart failure are present in the presence of preserved left ventricular systolic function (ejection fraction >45%). The incidence and prevalence of primary diastolic heart failure increases with age and it may be as high as 50% in the elderly. Age, female gender, hypertension, coronary artery disease, diabetes and increased body mass index are risk factors for diastolic heart failure. Hemodynamic consequences such as increased pulmonary venous pressure, post-capillary pulmonary hypertension, and secondary right heart failure as well as decreased cardiac output are similar to those of systolic left ventricular failure, although the nature of primary left ventricular dysfunction is different. Diagnosis of primary diastolic heart failure depends on the presence of preserved left ventricular ejection fraction. Assessment of diastolic dysfunction is preferable but not mandatory. It is to be noted that increased levels of B-type natriuretic peptide does not distinguish between diastolic and systolic heart failure. Echocardiographic studies are recommended to exclude hypertrophic cardiomyopathy, infiltrative heart disease, primary valvular heart disease, and constrictive pericarditis. Myocardial stress imaging is frequently required to exclude ischemic heart disease. The prognosis of diastolic heart failure is variable; it is related to age, severity of heart failure, and associated comorbid diseases such as coronary artery disease. The prognosis of severe diastolic heart failure is similar to that of systolic heart failure. However, cautious use of diuretics and/or nitrates may cause hypotension and low output state. Heart rate control is essential to improving ventricular filling. Pharmacologic agents such as angiotensin receptor blockers, angiotensin-converting enzyme inhibitors, and calcium channel blockers are used in selected patients to decrease left ventricular hypertrophy. To decrease myocardial fibrosis, aldosterone antagonists have a potential therapeutic role. However, prospective controlled studies will be required to establish their efficacy in primary diastolic heart failure.
It is well established that the syndrome of heart failure can occur in the presence of both preserved and depressed ventricular systolic function.[1,2] Primary diastolic heart failure is diagnosed when left ventricular (LV) ejection fraction is normal or near normal and primary systolic heart failure is diagnosed when there is a decrease in LV ejection fraction. It should be appreciated, however, that abnormalities of diastolic or systolic function do not always cause clinical heart failure. Furthermore, in both primary systolic and diastolic heart failure, some indices of systolic and diastolic function may be abnormal. For example, in dilated cardiomyopathy with a marked increase in ventricular diastolic pressure, a restrictive transmitral flow pattern (diastolic dysfunction) is frequently present. Similarly, in primary diastolic heart failure, although the ejection fraction is normal, myocardial contractile function may be depressed. It is also recognized that the phase of systole following completion of ejection until the closure of the semilunar valves (hang-out time) is related to myocardial relaxation. The isovolumic relaxation and rapid filling phases are also markedly influenced by systolic function.[3] Thus, systolic and diastolic phases and function are interdependent.
The clinical manifestations and hemodynamic consequences of diastolic and systolic heart failure may be similar, although the primary pathophysiologic mechanisms are different. Decreased ventricular compliance (increased stiffness) and abnormal diastolic filling are the principal functional abnormalities in patients with diastolic heart failure.[4,5] Decreased LV compliance is associated with a disproportionate elevation of its diastolic pressure, which causes a passive increase in left atrial and pulmonary venous pressures, which produces symptoms of pulmonary venous congestion. Passive increase in pulmonary artery pressure (post-capillary pulmonary hypertension), when severe, is the mechanism of secondary right ventricular failure associated with increased right ventricular diastolic and right atrial pressure and signs and symptoms of systemic venous hypertension. With a marked restriction in ventricular filling stroke volume may decline due to decreased preload associated with signs and symptoms of low cardiac output.
In primary systolic failure, a reduced LV ejection fraction is the initial functional derangement, which is associated with a disproportionate increase in end-systolic and end-diastolic volumes and pressures and a passive increase in left atrial and pulmonary venous pressures -- the hemodynamic mechanism of signs and symptoms of pulmonary venous congestion. Post-capillary pulmonary hypertension and right heart failure is associated with signs and symptoms of systemic venous hypertension. A decrease in forward stroke volume and cardiac output may also occur due to reduced ejection fraction. The mechanism of hemodynamic consequences in primary diastolic heart failure is summarized in Table 1 . It is apparent that it is difficult to distinguish between diastolic and systolic heart failure by clinical and hemodynamic profiles.
Am J Geriatr Cardiol. 2002;11(3) © 2002 Le Jacq Communications, Inc.
Cite this: Primary Diastolic Heart Failure - Medscape - Feb 01, 2002.