Targeting a protein that is essential for supporting the MYC oncogene could offer a new therapeutic approach to preventing prostate cancer (PC) metastasis, according to early research results in laboratory-grown cells and mouse models. MYC is a powerful oncogene that drives cell growth and proliferation in many different types of cancer, but cannot be targeted by conventional anticancer drug therapies.
Studies in laboratory-grown cells by researchers at Cold Spring Harbor Laboratory and Weill Cornell Medicine have now shown that blocking a protein known as PHLPP2 in human prostate cancer cells led to reduced levels of MYC, halting cell proliferation and leading to cancer cell death.
“Now, we have a new way of getting at this old foe in cancer research,” said Cold Spring Harbor Laboratory researcher Lloyd Trotman, PhD. “And that’s with an enzyme called PHLPP2, which presents a back-door route to target the gene … Our results suggest that targeted efforts to design pharmacologically relevant PHLPP2 inhibitors could result in very efficient new drugs that suppress MYC-driven cancer.” Trotman and Dawid G. Nowak, PhD, an assistant professor at Weill Cornell Medicine, are co-senior authors on the team’s paper, released today in the Journal of Cell Biology, which is titled, “The PHLPP2 phosphatase is a druggable driver of prostate cancer progression.”
Prostate cancer is one of the most common cancers in men, and causes up to 30,000 deaths every year in the U.S. alone, the authors wrote. Prostate cancer can be controlled if diagnosed and treated early, and the 5-year survival rate for prostate-confined disease is almost 99%. However, the prognosis is much worse when the prostate cancer has spread, and the 5-year survival rate for metastatic disease is only about 28%.
Understanding how genetic changes are linked to cancer progression can help to build a picture of the mechanisms that allow cancers to escape from their primary sites and spread to other organs. Unfortunately, the authors continued, there aren’t many samples of metastatic prostate cancer available for study, because taking biopsies at metastatic sites is invasive and can be dangerous, and also offers “uncertain” clinical benefit to patients.
Researchers are instead using genetically engineered mice (GEMs) to functionally test how individual gene alterations contribute to disease. Such studies have demonstrated a pivotal role for Pten as a key signaling suppressor that is involved in the onset, progression, and outcome of prostate cancer. The team’s prior studies have also shown that loss of a gene known as phlpp2 triggers prostate cancer on its own, and in combination with loss of Pten results in far more aggressive prostate cancer.
Trotman and colleagues recently developed a GEM model called RapidCaP, for studying metastatic prostate cancer. The model exhibits prostatic loss of the Pten and Trp53 genes, both of which are hallmarks of genetic changes in human metastatic prostate cancer. The newly reported studies in RapidCaP mouse-derived cultured cells showed that combined Pten and Trp53 deletion resulted in increased levels of total Myc and Phlpp2.
Surprisingly, knocking out Phlpp2 in addition to Pten and Trp53 deletion caused a sharp reduction in total levels of the Myc gene, whereas overexpressing Phlpp2 in the Pten/Trp53 knockouts led to increased Myc protein, “confirming the notion that PHLPP2 regulates Myc levels,” the team wrote. Interestingly, knocking out Phlpp2 in two different human metastatic prostate cancer cell lines resulted in up to 75% reductions in MYC protein. “Collectively, our results suggested that PHLPP2 both controls and is required to maintain MYC levels and proliferation of cells, possibly more efficiently in metastatic cell lines.”
Upregulation of MYC in different human cancers can occur via different mechanisms, and stability of the oncogene is regulated by a system of phosphorylation at two sites on the protein. The researchers’ studies found that PHLPP2 directly impacts on MYC phosphorylation, and stabilizes MYC by removing a phosphate group at the threonine-58 site (T58) that would otherwise trigger a process leading to degradation of the protein. “We show that PHLPP2 protects MYC from degradation. PHLPP2 dephosphorylates the T58 site of MYC, thus directly increasing its stability.”
Given their results the team hypothesized that using a drug compound to directly inhibit PHLPP2 might have an anticancer effect by suppressing the MYC protein. Tests with a PHLPP2 inhibitor termed NCI45586 led to dose-dependent reductions in total Myc protein in two GEM mouse-derived cell lines that were known to drive prostate cancer through Myc. Pharmacologic inhibition of phlpp2 also led to increased cell death in another mouse prostate cancer cell line, and in cells derived from the RapidCaP GEM model.
Treatment using the PHLPP2 inhibitor reduced cell viability and proliferation, and increased cell death in a human metastatic prostate cancer cell line. Similar results were obtained in bone metastasis-derived prostate cancer cells. “Our results with the NCI45586 tool compound closely mirrored those from genetic ablation of the PHLPP2 gene, a proof of concept that could lead to the development of pharmacologically relevant drugs,” the team stated “ … our results showed that the PHLPP2 function of protecting MYC can be targeted to kill PTEN mutant cells.”
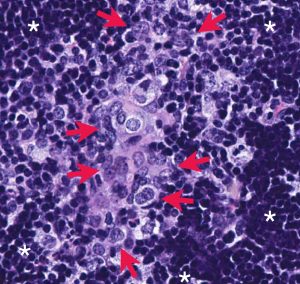
Encouragingly, RapidCaP GEM mice in which the Phlpp2 gene was knocked out (i.e., mice lacking Pten, Tp53, and Phlpp2) exhibited significantly lower overall disease burden compared with the original RapidCaP animals after 10 months. The triple knockouts also didn’t develop metastases, whereas the Pten/Tp53 knockouts developed metastases at multiple sites.
Knocking out Phlpp2 didn’t appear to have any adverse effects on normal cells. “Taken together, our in vivo genetic validation data demonstrated that Phlpp2 is required for the tumor and metastasis formation seen in the Pten/Trp53-mutant RapidCaP model,” the investigators commented. “The PHLPP2 phosphatase is an attractive drug target for several reasons. First, we show that Pten-deficient metastatic PC cells fully depend on it. In contrast, normal cells do not, as demonstrated by the normal viability of the phlpp2 knockout mice. Next, general advances in structural understanding of phosphatases have led to a “renaissance” of inhibitor design. By looking beyond the active site, novel allosteric inhibitors can now shut down phosphatases that used to be considered “undruggable.”
The team’s results are particularly promising given that scientists have to date been unable to find a way to target the MYC protein directly. Each year an estimated 450,000 people in the U.S. are diagnosed with a cancer that is driven by MYC. “Thus, our work introduces the PHLPP2 phosphatase as an unexpected, yet druggable, driver of MYC-driven PC and its progression,” the team concluded.

