The first time I tried to have sex I was 16. I knew it might hurt and that perhaps I would bleed. I was OK with that: it was part of the mythology. I imagined that, afterwards, I would stare at myself in the bathroom mirror, like the heroine in my own coming-of-age drama.
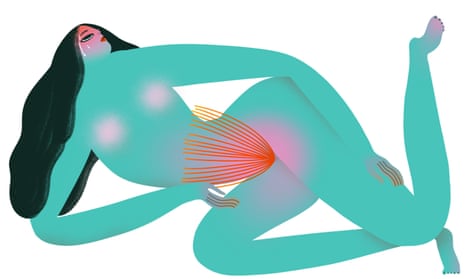
As it turned out, I had to stop the sex before it properly began. An excruciating pain at the opening of my vagina shocked me into total stillness – it felt like burning and ripping at once. I was so consumed with shame that I couldn’t have looked at my reflection if I had tried.
This was the first time I experienced what I now know as vulvodynia, an umbrella term for a condition characterised by chronic pain of the vulva. I was diagnosed at the age of 24, after years of being sent away from sexual health clinics with vague advice to “change positions”.
According to the US’s National Vulvodynia Association, as many as 16% of women experience the condition at some point. Some have pain only during penetrative sex or when using tampons; for others, it is far more severe – their discomfort is such that they can barely sit down. The pain itself is sharp and searing, and can range from giving the same sensation as severe thrush to feeling as if something inside you has been torn.
Amy*, 32, first noticed a problem when she was 14 and tried to insert a tampon. “The pain was so intense that I thought I was going to pass out.” She continued to use sanitary towels and the problem didn’t occur again until she lost her virginity at 17. “The problem stayed and never went away,” she says. She went to several doctors, none of whom had any answers. Last year, she went for a smear test. “I lay there in tears during what should have been a routine procedure.” She describes the pain as “like a red hot poker; the worst pain I’ve experienced.” She was referred to a gynaecologist and was finally diagnosed with vulvodynia.
There is no commonly agreed cause of the condition, because it isn’t defined by any physical abnormality. As a result, those living with it are often misdiagnosed with recurrent thrush, referred for psychosexual counselling (which is sometimes, but not always, necessary), repeatedly tested for sexually transmitted infections, or dismissed. “Because this is a condition you can’t see objectively, it’s harder to understand,” says Dr Attam Singh, a consultant in pain medicine at the London Pain Clinic.” It’s a very small and specific specialist problem within the speciality of gynaecology.”
Sue*, 51, began to experience vulval pain 12 years ago, but it was eight years before it was diagnosed properly. It started with a feeling of irritation in her genital area, especially when her legs were closed. “I was finding myself standing with my legs apart. It got so bad that I couldn’t even put on a pair of pants. I couldn’t sit down at all,” she says. “My GP, no matter how fantastic he was, had no idea, because everything looked absolutely fine.”
Sue first came across the term vulvodynia on the website for Channel 4’s Embarrassing Bodies. “It was everything I had. My husband asked the doctor to look it up and he said: ‘I think that’s it, yes.’”
Part of the problem is a lack of research. Dr David Nunns, a consultant gynaecologist at Nottingham City hospital, is one of the few experts in vulvodynia. Although the term has been around since the 1800s, it was only in the 1980s that it began to be taken seriously by the medical community. The research at that time was very much medically led, says Nunns, because there was little in the way of funding for research, but, he says: “In the last 10 years, there’s been more of a focus on a chronic-pain-management approach to the condition, which helps women to manage it.”
Dr Deborah Boyle is a consultant gynaecologist at the UK’s largest vulval service, based at the Royal Free hospital in London. She says the dearth of research into vulval pain can be partly explained by the reality of “a public health system that is so strapped for cash”, but also, because vulval pain is not an urgent public health issue, research into it is hard to do.
“If somebody has a pain problem, it has a massive impact on their life and their sense of self – but those consequences aren’t necessarily felt in the GP surgery or in the gynaecology service,” she says. “And when there isn’t a drug development issue, it’s harder to get anybody particularly interested, which I find quite depressing: it’s women’s quality of life.”
Dr Virginia Beckett, a spokeswoman for the Royal College of Obstetricians and Gynaecologists, agrees that NHS cuts are a major factor in the lack of awareness among healthcare professionals and long diagnosis times. “The NHS is in dire straits and sexual health services are now under the control of local councils rather than NHS trusts,” she says. “The services for women’s health have been fragmented; contraceptive services are now done mainly over the phone or on the internet.” In these conditions, it is no wonder that vulval pain – a frequently mystifying problem – flies under the radar.
A 2003 study in the US found that 60% of women who sought treatment for vulvodynia had seen three or more doctors, many of whom did not provide a diagnosis. “It takes an enormous amount of courage to visit a doctor and talk about such a personal issue, so to be dismissed is incredibly damaging,” says Amy. “The physical pain is one thing, but I think the emotional scars caused by years of suffering with no help, and feeling so isolated by it, have actually done the most damage.”
In her 2018 memoir Ask Me About My Uterus: A Quest to Make Doctors Believe in Women’s Pain, Abby Norman examined gender politics and medicine. Why is it that vaginal pain is still so misunderstood? “When the definition of so-called ‘textbook cases’ have primarily been written by men, the language used becomes precedent,” she says. “We see echoes of this when the health concerns of anyone who doesn’t identify as male are dismissed or disbelieved. Women seem especially prone to being outright accused of manipulation or hysteria.”
There are, however, places women like me can turn to. The Vulval Pain Society (for which Nunns is a medical adviser) is a charity that provides crucial information about many aspects of vulval pain, largely via the internet. Indeed, for many women, especially those in locations where care is difficult to access, the internet has been a godsend. The fact that I recently asked to be referred for physiotherapy was entirely down to recommendations on a Facebook group.
Becki, 21, has also experienced the positive effects of online resources. She heard about “the only treatment that has helped” – the neuropathic pain medication amitriptyline, which is among the most common treatments for vulvodynia – through social media. Becki runs the Instagram account @vulvodyniasupport to stop people like us “feeling so isolated”. As with any chronic pain, vulvodynia can be alienating, with many women reporting the loss of careers or relationships.
Rebecca, 33, was forced to resign from her job in HR because she was in too much pain. “I had just gone to university and was doing my postgraduate diploma, but I was just not able to stay in work,” she says. “It was pretty sad, really.” She says that discovering Facebook support groups such as Vulvodynia UK when she was feeling most alone was “a turning point … Having that community is really helpful.”
And there is a growing understanding about the condition in the medical community. Beckett is optimistic about “vulva clinics that are run with a multidisciplinary approach – dermatologists and gynaecologists working together.”
Boyle, whose patients travel to her clinic from all over the UK, views vulval pain as “not that difficult to treat, as long as you’ve got the right diagnosis and the specialised team of physiotherapy colleagues”. She says her work has “a cure rate in the order of 85%”.
In my case, the pain persists, but I am now being treated and am receiving excellent care – although this is bittersweet, considering the years I spent suffering quietly, terrified by my body. Now, however, as vulvodynia’s profile grows, so, too, do women’s chances of receiving the treatment they need and deserve.
*Names have been changed
Comments (…)
Sign in or create your Guardian account to join the discussion