Pathophysiology
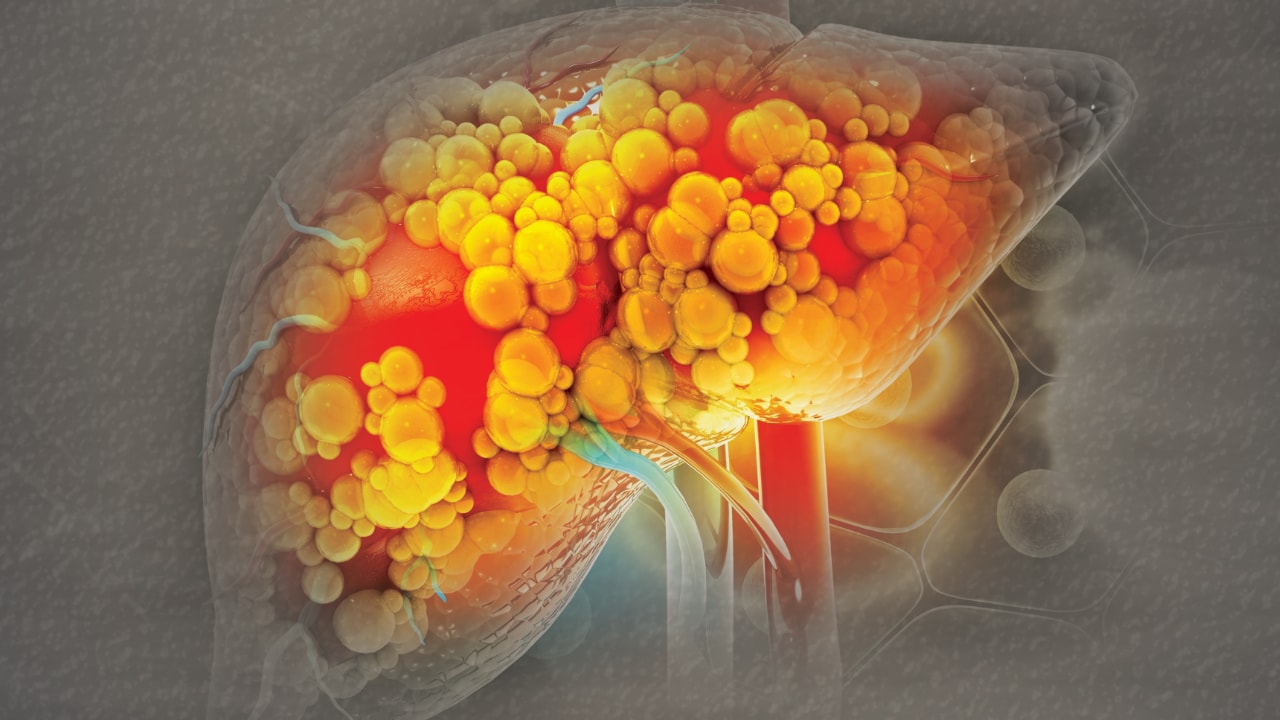
Two histological presentations of NAFLD occur: fatty liver and NASH. With fatty liver, infiltration of fat changes hepatocyte shape, resulting in swelling and nuclei displaced to the edge of the cell.[4] This "ballooning" indicates cellular injury and degeneration. NASH is the progressive form of NAFLD, which is characterized by inflammation and heptocyte necrosis, and it can progress to cirrhosis.
Although the exact mechanism of NAFLD pathology is unknown, several hypotheses suggest that the liver damage is multifactorial. The multi-hit hypothesis describes proposed NAFLD pathology.[6] The first insult, or hit, to the liver occurs from insulin resistance. This causes increased levels of fatty acids that result in fatty infiltration of the liver, or steatosis. These hits continue and the increasing fatty acids eventually cause apoptosis, or cell death, of hepatocytes.
Other hypotheses suggest that, after the first hit with insulin resistance and fatty infiltration, a second hit from a gut and adipose tissue-derived endotoxin may cause progression to NASH.[10] The multiple-parallel hits hypothesis proposes that many insults to the liver happen concurrently, ultimately causing fatty infiltration and hepatic inflammation. Regardless of the hypothesis, progressive liver damage at the cellular level seems to stem from a combination of insulin resistance and fat deposit in the liver that ultimately result from obesity.
It is not entirely clear what causes progression from NAFLD to NASH, although insulin resistance appears to be a marker for both initiation of fatty liver disease and its progression to NASH. Other possible risk factors for progression include increasing weight, age progression, and an aspartate aminotransferase/alanine transaminase (AST/ALT) ratio > 1 (normal is < 1).[11]
Hepatic iron deposits, or hemochromatosis, may also be a causative factor for disease progression. The role of iron accumulation has been established for other chronic hepatic diseases, but its role in NAFLD and NASH remains unclear.[12] Promising research links the more severe forms of NAFLD to iron deposits that occur exclusively in the reticuloendothelial system, while mild disease states show iron accumulation exclusively in hepatocytes.
Finally, there may be a genetic predisposition to NAFLD related to the risk factors of acquiring metabolic syndrome.[13] Factors that tend to cluster in families include obesity, insulin resistance, type 2 diabetes, high triglyceride levels, and low HDL cholesterol levels. The familial clustering of NAFLD related to these comorbidities is also mediated by lifestyle and environmental factors, particularly diet and exercise. Therefore, it is not yet known whether NAFLD is related to genetic factors, learned behaviors, or a combination of both.
Journal for Nurse Practitioners. 2012;8(1):45-50. © 2012 Elsevier Science, Inc.







Comments