Coronavirus Today: Aiming for vaccine equity
Good evening. I’m Amina Khan, and it’s Wednesday, Dec. 30. This newsletter is taking the rest of this week off for the holiday, so here’s what’s happening with the coronavirus, plus a few good reads to tide you over through the long New Year’s weekend.
It’s no secret that communities of color have suffered outsized numbers of infections, hospitalizations and deaths. Now that two COVID-19 vaccines have been rolled out to healthcare workers and nursing home residents, health officials are teetering their way across a precarious high wire: how to diplomatically nudge communities of color to the front of the line for the scarce shots without triggering a political or legal backlash.
This balancing act is tricky because America has long been deeply divided over racial quotas and affirmative action, my colleague Melissa Healy writes — and assigning vaccine priority based on race or ethnic heritage could open the door to recrimination and courtroom challenges at a crucial point in the pandemic fight.
The numbers clearly show that this pandemic is deeply discriminatory. Black and Latinx Americans are hospitalized with COVID-19 at rates roughly four times that of white Americans, and their risk of dying of COVID-19 is almost three times as high. American Indians and Alaska Natives are also nearly twice as likely to die from the disease as white Americans, according to the Centers for Disease Control and Prevention.
This is because people of color are treated differently — and unequally — in this society in many different and interwoven ways. Public health experts and medical ethicists have said with near-unanimity that the burdens of poverty, discrimination and social disadvantage have led to outsized rates of infection, hospitalization and death in these communities. And that excess vulnerability demands that they get some priority access to vaccines.
But saying plainly that race and ethnicity should be taken into account will not sit well with everyone. So experts and authorities have focused instead on equity as a key factor in determining how vaccines should be allocated.
In cases where conditions of work, housing, transportation and education conspire to make a group of people more vulnerable to COVID-19, the government’s key panel of vaccine advisors cited equity as the reason for giving that group early access to a vaccine. Skin color and ethnicity are treated as incidental — they just happen to be strongly correlated with those conditions.
That’s a big reason why the panel put essential workers in line right behind healthcare workers and nursing home residents.
“If we’re serious about valuing equity, we need to have this,” said Dr. Beth P. Bell, a panel member and expert on pandemic preparedness at the University of Washington.
Racial preferences for COVID-19 vaccines are “an ethical imperative,” said Lawrence Gostin, a Georgetown University expert in public health law — and there are many ways for state and local public health agencies to aim for vaccine equity without running afoul of the law.
For example, “a vaccine distribution formula ... could lawfully prioritize populations based on factors like geography, socioeconomic status, and housing density that would favor racial minorities de facto, but not explicitly include race,” Gostin and two colleagues wrote in the Journal of the American Medical Assn.
Public health agencies “should not exacerbate racial divisions” with their vaccine decisions, the trio wrote. But they have an opportunity to become “agents of change toward improving social and racial justice,” they said.
Harald Schmidt, a medical ethics and health policy expert at the University of Pennsylvania, was one of Gostin’s coauthors. Schmidt said he was surprised by the “embrace of equity” in so many states’ vaccination plans. But perhaps, in the middle of a pandemic, he said, “it’s smarter to not talk about race and just do it.”
By the numbers
California cases, deaths and vaccinations as of 5:42 p.m. PST Wednesday:

Track the latest numbers and how they break down in California with our graphics.
Across California and beyond
Just one day after officials in Colorado reported that a new, potentially more contagious variant of the coronavirus had arrived in the U.S., that strain was identified in California, Gov. Gavin Newsom said Wednesday. The carrier is a 30-year-old resident of San Diego County, officials there said.
Although there is some evidence that the variant identified in Britain spreads more easily, many scientists are skeptical that the genetic changes in this strain (known as B.1.1.7) really do make it more contagious. There are other possible explanations for its rapid spread in England, such as being in the right place at the right time to fuel transmission through dense communities.
In any case, “there’s no indication at all that it increases the virulence … the ability to make you sick or kill you. It doesn’t seem to make it more strong in that regard,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases. Another bit of good news: The COVID-19 vaccines developed to date appear to be effective against the variant, Fauci added.
The initial patient in Colorado was identified Wednesday as a member of the state’s National Guard who had been sent to help out at a nursing home struggling with a coronavirus outbreak. A second guardsman may have the variant too, officials said.
The tsunami of coronavirus cases continues to wreak new kinds of havoc on Southern California’s healthcare system. Paramedics and emergency medical technicians are now declining to transport some less severely ill patients whom, in non-surge times, they might otherwise take to the hospital. After being assessed, these patients are being asked to remain at home because “if they did come to the hospital, they may not get the type of attention that they might expect,” said Dr. Mark Ghaly, the state health secretary.
It’s one of the steps health workers are being forced to take as Los Angeles County struggles to deal with the hospital-crippling surge. Many hospitals are now performing contingency care, in which staffers work longer hours and wards are reconfigured to take in more patients. The next step may be “crisis care,” in which more medical rationing would take place.
“State officials have yet to hear reports of the direst circumstances, such as a hospital having to choose who gets the last ventilator,” my colleagues Rong-Gong Lin II and Melissa Gomez write. “But there are fears that day could come.”
Elsewhere in the U.S., the man who would have been Louisiana’s newest Republican member of Congress died Tuesday night from complications related to COVID-19. Luke Letlow was only 41, and he was just days away from being sworn in to serve in the House of Representatives.
Letlow won his runoff election on Dec. 5 and was admitted to a Monroe hospital two weeks later. He was later transferred to Ochsner LSU Health Shreveport, where he was treated in the hospital’s intensive care unit.
Republican Sen. Bill Cassidy of Louisiana, a doctor who had COVID-19 earlier this year and has since recovered, posted in a Twitter video: “It just, just, just, just brings home COVID can kill. For most folks it doesn’t, but it truly can. So, as you remember Luke, his widow, his children in your prayers, remember as well to be careful with COVID.”
U.S. researchers have kicked off a big study of another vaccine candidate that could bolster the country’s scarce supply if it is authorized for emergency use. The experimental vaccine made by Novavax Inc. is the fifth to reach final-stage testing in the U.S. About 30,000 volunteers are needed to evaluate the vaccine, which is a different type from those made by Pfizer and Moderna.
This vaccine uses harmless, lab-grown copies of the coronavirus’s spike protein to train the immune system to recognize the real deal. The Pfizer and Moderna vaccines, in contrast, use a newer technology that injects the genetic code for that protein and then relies on a recipient’s cells to make it. Johnson & Johnson and AstraZeneca also have vaccine candidates in late-stage testing.
Britain on Wednesday became the first country to authorize AstraZeneca’s cheap and easy-to-handle COVID-19 vaccine. The move adds another weapon to health officials’ arsenal amid a surge so severe that the government has extended lockdowns to three quarters of England’s population.
The vaccine, developed in partnership with Oxford University, could be very appealing in the developing world thanks to its low cost and because it can be kept in regular refrigerators rather than at the ultra-cold temperatures that some other vaccines require.
Partial results from studies in nearly 24,000 people suggest the shots are safe and about 70% effective at preventing COVID-19. (Moderna and Pfizer’s offerings were 94% and 95% effective in their respective clinical trials.) But there are some questions about how well the AstraZeneca doses protect older people. Here’s an explainer covering how the AstraZeneca vaccine compares.
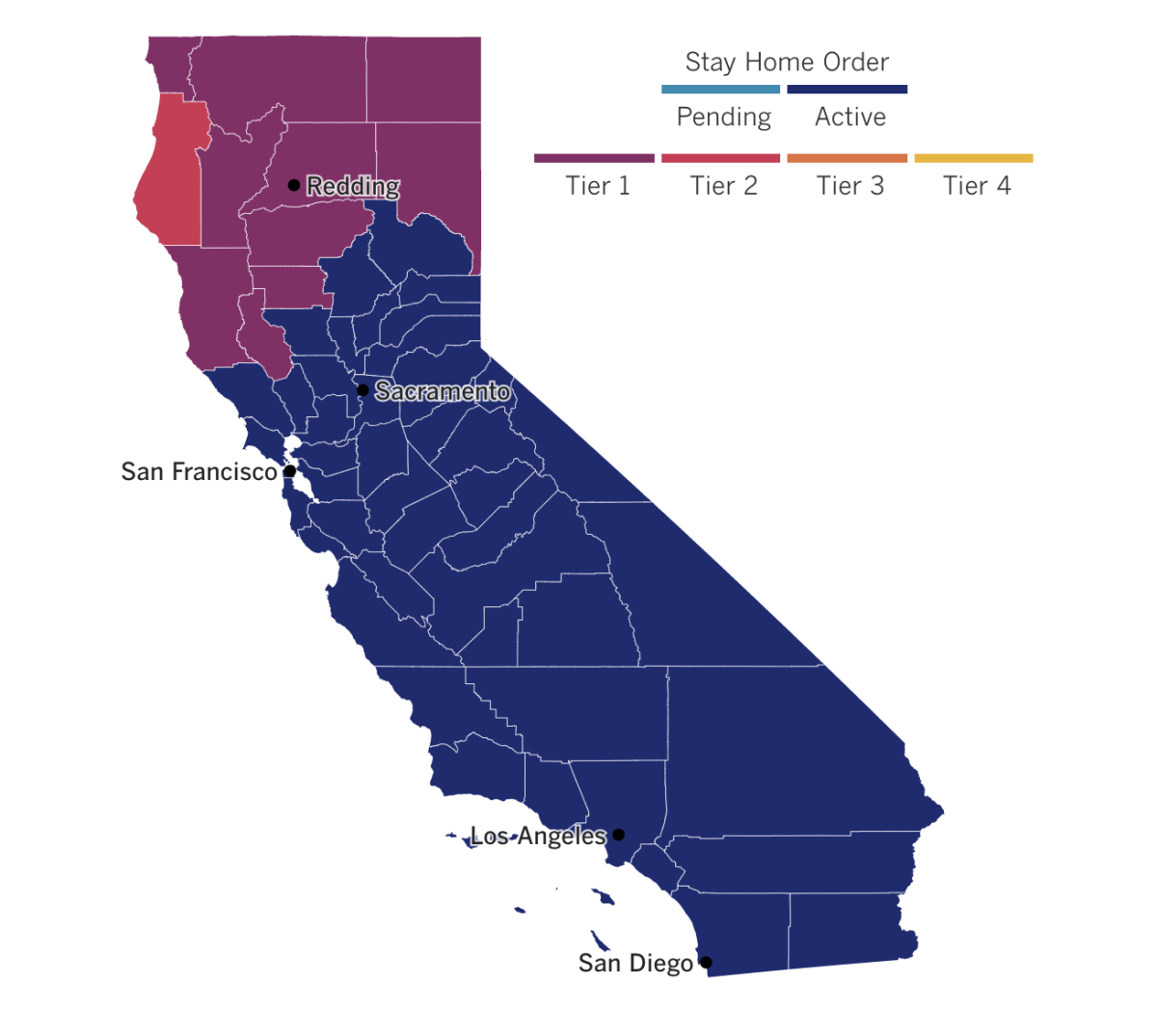
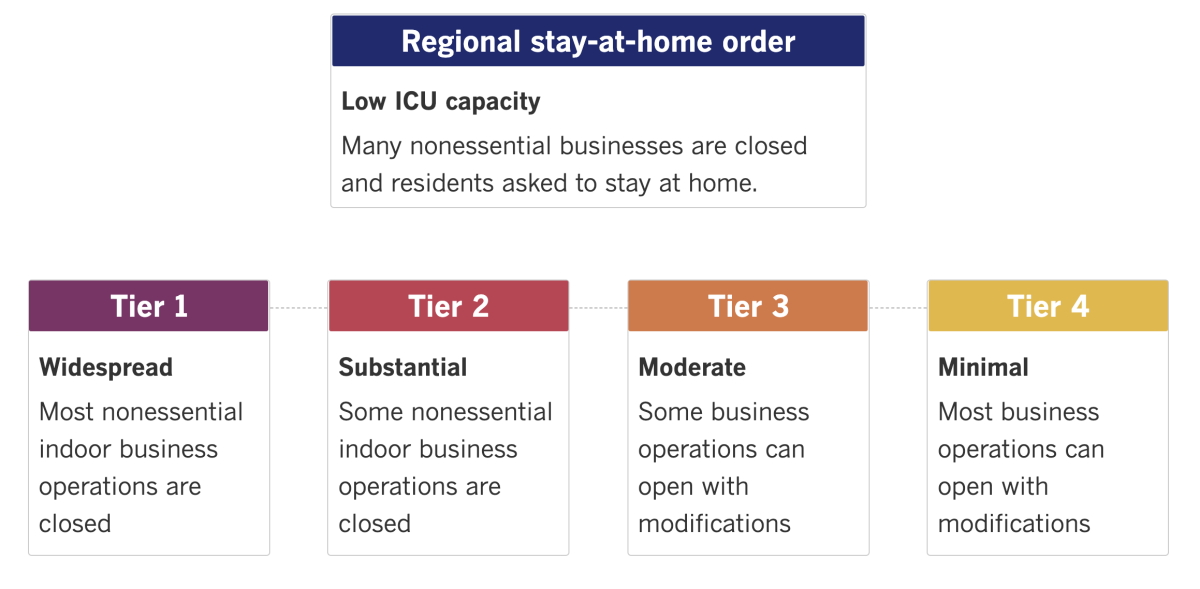
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Long (weekend) reads
‘Like practicing Civil War medicine’
All hospitals in Los Angeles County are being slammed by waves of COVID-19 patients. But those that serve the poor and communities of color have been hit the hardest — and they face the biggest hurdles when it comes to providing their patients with quality care, a Times analysis shows.
Take Kaiser Permanente Downey Medical Center, where more than 80% of patients either have or are suspected to have been infected with the coronavirus. Patients were “piled in administrative hallways, stuffed in the corners, hanging over chairs,” one healthcare worker said. When the emergency room ran out of crevices, staffers began treating people right in the waiting room. “It was like practicing Civil War medicine. It was the worst shift of my life,” the worker said.
Martin Luther King Jr. Community Hospital in Willowbrook has 131 beds and 128 COVID-19 patients. By Monday afternoon, when the patient census reached 215, administrators were ready to declare an internal disaster, meaning it did not have the staff or space to admit any more patients.
Soon, hospitals will have to start rationing care, said Dr. Elaine Batchlor, the hospital’s chief executive. “It’s horrible, it’s something that no health professional wants to contemplate,” she said. Her hospital is so full because many patients are essential workers who put themselves at risk every day, and who had preexisting chronic diseases that they’d struggled to get treatment for. “This has made our community here a setup for having a very difficult time with COVID, and it’s all playing out in real time as one might expect,” Batchlor said.
East L.A., reshaped by the pandemic
The coronavirus has left its mark on nearly every street corner in this predominantly Latino neighborhood, from the “We cash all stimulus checks” banner hanging outside a payday-loan spot to the way that three women outside a clinic quietly reposition their bodies when someone nearby coughs. In these seven square miles, more than 1 in every 10 people has tested positive for the virus — the second-highest recorded tally of any region in the country.
In this dispatch from East L.A., my colleagues weave together stories of people living and working just minutes from one another: an overwhelmed funeral home director with four employees who each lost loved ones to COVID-19 in less than a week; a novice florist struggling to keep up the family business after her husband was deported; high school students waiting on life-changing news from top-tier universities; and a family struggling in myriad ways to survive this new, shared reality. Give it a read — it’s well worth your time.

Reaching out to failing students
For teachers, winter break has traditionally served as a much-needed respite from the rigors of schooling. But this year, English teacher Keara Williams has been working the phone nonstop as she tries to make contact with 28 students (including 11 seniors) who received an “incomplete” grade at the end of the fall semester. If they don’t complete makeup work to raise their grade to at least a D by the end of January, they will fail her class. But she tells them not to give up — and that she’ll work with them over her vacation if that’s what it takes to avoid an F.
Williams isn’t the only one. Many teachers in the Los Angeles Unified School District are finding themselves in the same position in the midst of a pandemic that has closed campuses for nine months and burdened so many students with unforeseen hardships. Teachers are struggling to balance compassion and empathy with the low grades in their record books, and trying to find ways to engage their lost students before it’s too late, my colleague Melissa Gomez writes.
“For me, it’s personal. I want to know what’s going on, but they’re not answering,” Williams said. Even when she’s not sitting behind her computer, she’s still working the problem in her head: “How do I be the most effective teacher?”
Curbside. Covidiot. Doomscrolling
The pandemic has changed how we work, how we socialize, how we dress — and it has also changed the way we speak. “As 2020 comes to a close, many of us find ourselves fluent in a new language that would have been nearly indecipherable just one year ago,” my colleague Deborah Netburn writes. For example, it’s safe to assume a “socially distanced” picnic likely means that all the guests stayed at least six feet apart and did not share food or drinks. And public health officials aren’t the only ones who know what it means to “flatten the curve.”
While the English language is always in flux, linguists and lexicographers say this has been a banner year for the sheer volume of words that have entered our daily lives. “It’s the global aspect of this that’s so mind-blowing,” said Fiona McPherson, a senior editor of the Oxford English Dictionary. “All of us have been affected by the pandemic, at least indirectly. So we’re all having these conversations and using the same type of language.” Take a peek at this surprisingly delightful pandemic story and appreciate the tiny, spoken ways in which — through a difficult year — we’ve still managed to achieve a little growth and change.
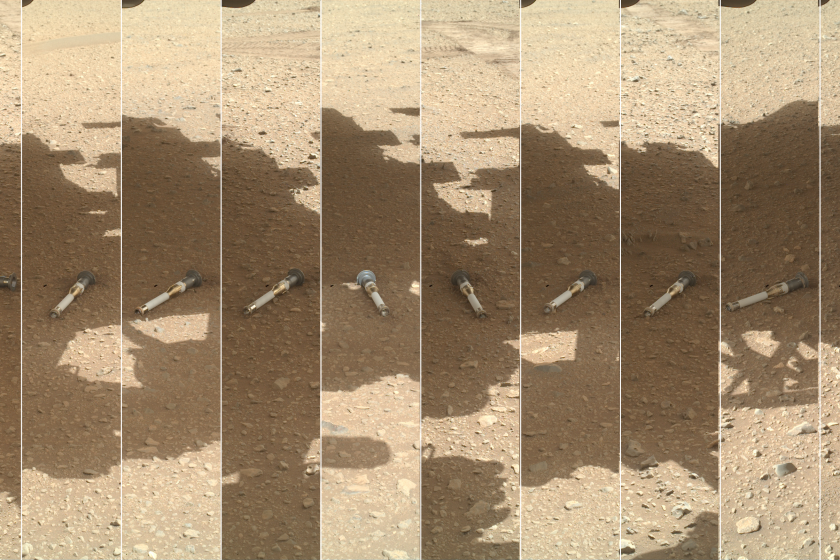
The pandemic in pictures

The pandemic has reshaped daily public life for people around the world, and this story about COVID-19 design solutions looks at the myriad ways that is quite literally true. “As COVID-19 barraged us with new challenges, it also forced adaptation that in the design world translated to faster, lighter, cheaper and more flexible buildings and landscapes,” architecture journalist Sam Lubell writes.
Lubell offers a sampling of 14 clever COVID hacks from around the world — including this park in Elblag, Poland, where grass mowed into a checkerboard pattern delineates safe social distances for those seeking an outdoor escape from isolation at home.
Folks, it’s been a rough 2020. The challenges and hardship will continue as we move into 2021, but so will the fight to get this pandemic under control. Hope is on the horizon as the vaccine rollout continues. As we bid good riddance to the old year and turn to face what comes, I want to wish you all a Happy New Year, and the best it has to offer. Stay safe, be well, and see you Monday.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.