Diagnosis
The diagnosis of ectopic pregnancy requires differentiating it from a viable intrauterine pregnancy. This is done with the use of ß-human chorionic gonadotropin levels (ß-hCG), transvaginal ultrasound and, in some cases, uterine curettage. Although progesterone levels are typically higher in intrauterine gestations compared with ectopic gestations and a progesterone level of less than 5 ng/ml can rule out a viable pregnancy, there is not a definitive value that demarcates the two.[12] Therefore, progesterone levels often do not aid in the diagnosis of ectopic pregnancy.
A transvaginal ultrasound can confirm the presence of an intrauterine gestation by 5.5 weeks in almost all cases. However, a gestational sac can be identified on transvaginal ultrasound as early as 4.5-5 weeks gestation and a yolk sac is visible on ultrasound by as early as 5 weeks. A fetal pole with heart motion can be seen by 6 weeks' gestation.[13] However, because patients are not always certain of their last menstrual period, ß-HCG levels are often used to determine when an intrauterine gestation should be seen on transvaginal ultrasound. This cutoff level of ß-hCG varies by institution but ranges from 1500 to 2500 mIU/ml. Setting a low ß-HCG cutoff value increases the sensitivity of ultrasound and ß-hCG at diagnosing an ectopic pregnancy but increases the risk of missing a viable intrauterine pregnancy. A higher ß-hCG cutoff value is used to maximize specificity, or to ensure a viable intrauterine pregnancy is not missed. If the ß-hCG level is below this value at presentation, serial ß-hCG levels must be obtained to assess viability.
With the use of radioimmunoassay and specific antiserum to ß-hCG, levels can be detected in serum at 1 mIU/ml and in the urine at 20 mIU/ml. This allows for very precise quantification of ß-hCG and allows clinicians to accurately follow trends in ß-hCG levels. Traditionally, an increase of at least 66% over 2 days would confirm the presence of a normally developing pregnancy.[14] However, more contemporary ß-hCG curves have determined that some viable pregnancies have a slightly slower increase in ß-hCG levels, with a 99 percentile demonstrated to be a 53% rise in 2 days. This is the expected rate of rise in ß-hCG values less than 10,000 mIU/ml. Rare cases of intrauterine gestations have been noted with ß-hCG levels increasing 35% in 2 days.[15,16] However, ß-hCG levels rise similarly to a normally developing pregnancy in 21% of ectopic pregnancies, so ultrasound remains an important part of the diagnostic work-up when ß-hCG levels reach the discriminatory cutoff.[17]
In 85% of abnormal pregnancies, there is an abnormal rise in ß-hCG levels or a plateau in ß-hCG levels. A rapid decline in ß-hCG levels, which is defined as a decrease of 21-35% (depending on initial levels) over 2 days, is most indicative of a miscarriage. However, declining ß-hCG levels may also be seen in resolving ectopic gestations.[17] It is important to follow weekly ß-hCG levels in these patients until they are undetectable. In patients with abnormally rising ß-hCG levels, an abnormal intrauterine gestation needs to be differentiated from an ectopic pregnancy.
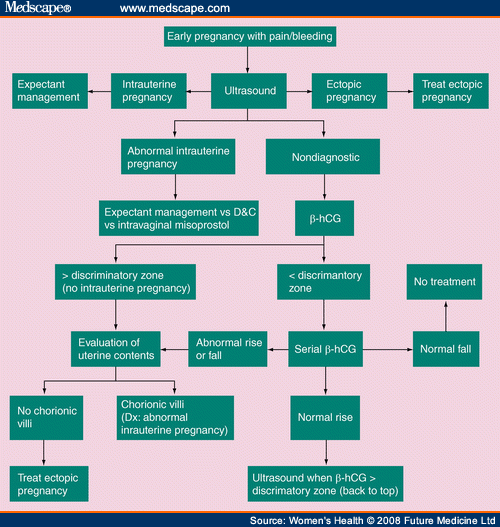
If ß-hCG levels are above the discriminatory cutoff value, an ultrasound should be performed. See the algorithm in Figure 2. Using transvaginal ultrasound, an intrauterine pregnancy should be seen when ß-hCG levels are greater than 2000 mIU/ml. It is important to evaluate the adnexa even when an intrauterine pregnancy is seen to evaluate for a heterotopic gestation. When an intrauterine pregnancy is not visualized and an extraovarian, noncystic adnexal mass is seen on ultrasound, this finding has a sensitivity ranging from 84 to 90% and a specificity of 94-99% for ectopic gestation.[18,19,20] Most (57.9%) ectopic gestations seen on ultrasound will present as a homogeneous mass with the rest presenting as a mass, with a hyperechoic ring around a gestational sac (20.4%) or a gestational sac with a fetal pole and with or without cardiac activity (13.2%).[18]
Figure 2.
Diagnostic algorithm for ectopic pregnancy. Adapted from reference 54. ß-hCG: ß-human chorionic gonadotropin levels.
Ectopic pregnancies can cause the formation of a pseudogestational sac in the endometrium, which is a collection of fluid in the endometrial cavity caused by bleeding from the decidualized endometrium. A pseudogestational sac is centrally located whereas a true gestational sac is often eccentric in location, but the two can be confused on ultrasound. Other ultrasound findings seen with ectopic gestations include a corpus luteum, which is seen on the same side as the ectopic gestation in 70-85% of cases.[18,21,22] In addition, the presence of blood in the pelvis is seen in approximately 30% of ectopic gestations and may be the result of tubal rupture or leakage of blood from the fallopian tube.[18]
When a nonviable gestation has been confirmed, but its location has not been determined by ultrasound, a dilation and curettage (D&C) should be performed. Two such situations are when the hCG is above the discriminatory zone and no intrauterine pregnancy (or extrauterine) gestation has been visualized or in the case of abnormally rising ß-hCG levels as part of the workup for ectopic pregnancy. In both cases, a histological examination should be performed on the evacuated uterine contents to look for the presence of chorionic villi. If chorionic villi are identified, the diagnosis is an abnormal intrauterine gestation, which is treated by the D&C. If chorionic villi are not present on histological examination, the diagnosis of ectopic pregnancy has been made and treatment should ensue. However, there are cases in which histological examination of the specimen is not readily available or may be unreliable. In these cases, before treatment for an ectopic pregnancy is begun, a quantitative ß-hCG should be performed prior to the D&C and a second level should be drawn 12-24 h later. The ß-hCG level should decrease by at least 15% in this time if an intrauterine pregnancy was evacuated. In most cases of a nonviable intrauterine pregnancy, the decline is more dramatic. If the ß-hCG does not decline after the contents of the uterus have been removed, the diagnosis of an ectopic pregnancy can be made and treated accordingly. Again, it is important to follow weekly ß-hCG levels until they are undetectable to confirm resolution of the pregnancy.
Women's Health. 2008;4(1):79-87. © 2008 Future Medicine Ltd.
Cite this: Ectopic Pregnancy: Diagnosis and Management - Medscape - Jan 01, 2008.






Comments