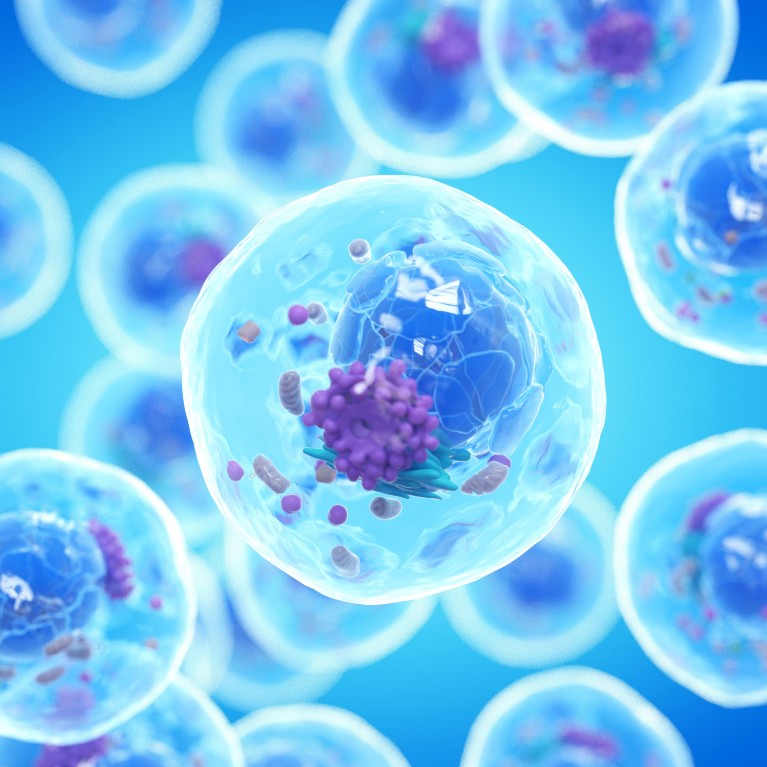
Each cell has its own DNA with epigenetic markers, and unique RNA transcripts and protein output. Examining tumours at the single-cell level provides a big picture perspective of how the cancer might react to treatment.Credit: Science Photo Library/Shutterstock
The more you look at cancer, the more variation there is. “A pea-sized tumour can have dozens, hundreds, thousands of clones and daughter cells that each have slightly different genetic mutations and gene expression,” says Kelly Paulson, an oncologist at the Swedish Cancer Institute in Seattle, Washington.
Cancer cells, both within and between tumours, can have distinct cellular morphologies, gene expression patterns, proliferation rates, metastatic potential and sensitivity to treatment. This heterogeneity is a major obstacle to understanding and treating cancer. “The high chance of having one or a few resistant clones at the start of treatment explains why current therapies often cause tumours to shrink but are rarely, and only for certain cancers, a cure,” Paulson adds.
Traditional molecular profiling techniques, often described as bulk sequencing, are useful for identifying common mutations and gene expression patterns associated with cancer, but can’t often identify rare, clonal subpopulations. Single cell technologies, however, analyse the DNA mutation and gene expression patterns of many individual cells, so can potentially identify resistant cells before or during treatment. Bulk sequencing and single cell sequencing have been likened to smoothies and fruit salads, respectively. Determining the types and features of the fruit (cells) is much easier before they go into the blender.
Technological advances that allow researchers to gather and interpret genome-wide information from thousands of individual cells are opening new avenues for cancer research. High-throughput technologies that sequence a cell’s DNA (genome), the epigenetic markers that regulate gene expression (epigenome), RNA readouts of gene expression (transcriptome) and protein expression (proteome) are providing new insights into cancer metastases and recurrence. Moreover, being able to examine such data over time and space will allow researchers to test new hypotheses on the role of the tumour microenvironment and cell-cell interactions in cancer progression and potentially discover new treatment targets.
Acquiring new layers of information
“Single-cell sequencing offers a level of data resolution that was not available before,” says Ignaty Leshchiner, a computational biologist investigating post-treatment tumour heterogeneity, who is a senior group leader in the Cancer Genome Computational Analysis group at the Broad Institute in Cambridge, Massachusetts. Leshchiner is developing methods to integrate single-cell and bulk-sequencing data. By merging both types of information from tumour samples, he aims to more accurately identify disease-associated genes and pathways than by using either method alone.
“One of the benefits of high-throughput single cell sequencing is that it provides multiple measurements of a recurrent cell type or state,” says Leshchiner. This approach allows him to reliably characterize subpopulations of cells. That is not to say there is no value in bulk analyses — they can be used to reconstruct major subpopulations of cells and assign detected mutations to them1, whereas single-cell DNA sequencing struggles at this task owing to the loss of large portions of the genome during the extraction process. “By using both bulk and single cell approaches we get a better picture of what is going on and can start to examine the effects of genetic mutations on disease kinetics,” Leshchiner says.

Tumour cells and beyond
Single cell sequencing has applications beyond the actual tumour cells. There is increasing evidence that non-malignant cells within and around tumours have important roles in disease progression. Research into this so-called tumour microenvironment has particular relevance for immunotherapies that target immune cells rather than the cancer cells themselves. Such immune-enhancing strategies have shown remarkable success against a number of cancers, including certain types of lymphoma, melanoma, leukaemia and lung cancer.
It is unclear, however, why most immunotherapies only work in some patients and often for a limited time. By studying the complex interactions between immune cells and cancer cells, researchers are starting to uncover the reasons behind these failures. “Single-cell RNA sequencing has truly revolutionized our understanding of the tumour microenvironment and of why immunotherapies can stop working,” says Paulson.
There are several reasons why patients might experience cancer recurrence after months of immunotherapy. For instance, cancer-killing immune cells may no longer be active or able to infiltrate tumours, or the cancer cells might have found a way to evade them. When Paulson and colleagues used bulk exome sequencing to investigate why two patients with metastatic skin cancer relapsed after a year of remission with immunotherapy, they couldn’t find any additional tumour-associated mutations that could explain their escape from the immune response.
When they used high-throughput single-cell RNA sequencing to examine the cells’ transcriptome, the researchers found that the tumour cells had reduced expression of a particular gene (either HLA A or B), making the cells invisible to the immune system2. The gene in question encoded a cell-surface protein that exposed the antigen targeted by the immune cells. Mutations in this gene had previously been shown to promote tumour growth by facilitating immune evasion. But these patients’ genes were not mutated. Instead, the gene’s expression was downregulated, which had the same effect of making the cancer cells resistant, just without a DNA change. By using multimodal (RNA and DNA) analysis, Paulson’s study had revealed a novel regulatory mechanism at the transcriptional level — and one that is potentially reversible by drug therapy.
Determining the sequence of events
How does immunotherapy induce such a response at the transcriptional level — and, is it reversible? These are questions that Ramanuj DasGupta, a cancer researcher at the A*STAR Genome Institute of Singapore, is tackling by examining the transcriptome and epigenome of single cancer cells pre- and post-treatment.
“Single-cell RNA-sequencing allows us to map the trajectories of individual cells as they evolve under the selective pressure of drugs,” says DasGupta. These trajectories are allowing him to determine whether the drug-resistant cell subpopulations were there from the start, before treatment, or whether they have emerged in response to therapy.
His team is finding that there are cancer cell clones bearing transcription-regulating chromatin marks on resistance-associated genes before treatment begins. These marks mean that the cells are ready to be epigenetically reprogrammed and change their gene expression. For instance, after these cells are exposed to the chemotherapeutic drug cisplatin, the researchers found that previously inaccessible regions of the cells’ genome had started to recruit transcription factors and activate gene expression3 — beginning the transition to resistance. The heterogeneity of cancer cells at the epigenetic level supports the use of drugs that target epigenetic regulators, such as acetyltransferase inhibitors, to prevent or reverse drug resistance.
Improvements in chromatin accessibility assays, such as ATAC-seq (assay for transposase-accessible chromatin using sequencing), mean that researchers can obtain genome-wide patterns of gene switch activity at the single cell level. Combining this information with genomic and transcriptomic data helps them to understand the role of mutations in regulatory regions and their resulting effects on gene expression.
Amassing this information is beyond the scope of one lab. DasGupta hopes to draw on data generated from collaborative programmes across Singapore. “We are in the process of developing a comprehensive cancer research strategy that combines single-cell sequencing efforts at the genomic, epigenomic and transcriptomic levels,” he says. He is enthusiastic about the volume of data that will be produced in the next five years and how it will advance knowledge on the mechanisms involved in resistance to immunotherapies or standard chemotherapies.
Adding another dimension
One of the areas in single-cell research that is most exciting scientists is the development of imaging technologies. Imaging allows the simultaneous visualization of the expression of thousands of genes in tissue sections, known as spatial transcriptomics. “By adding spatial resolution to the single cell transcriptomic signatures, we are able to see how cells interact and function within a tumour,” DasGupta says. Finding certain cell types or cell states in particular locations, in the periphery of the tumour or surrounded by T cells, for example, may offer new clues about the role of these cells in metastasis, T cell infiltration or T cell exhaustion.
DasGupta says this knowledge could lead to a shift from mutation-driven treatment strategies to ones that account for the transcriptomic signature of the tumour and its microenvironment. As single-cell sequencing approaches help to reveal the presence and features of non-tumour cells in many cancer types, spatial transcriptomics could shed further light on how their interactions with tumour cells influence disease progression. Already there are many candidates for investigation that could help prevent disease progression or recurrence, including cancer-associated fibroblasts4 and conserved myeloid populations in lung cancer5, osteoclasts and osteoblasts in prostate-cancer bone metastasis6, and pancreatic stellate cells in pancreatic-ductal-adenocarcinoma drug resistance7.
Looking ahead
Improved protocols for DNA and RNA amplification from single cells, together with the growing scale and declining cost of sequencing technologies are making single-cell methods more attractive and accessible to researchers. Steven Hoffman, segment marketing manager for single-cell sequencing at Illumina, a leading sequencing technology provider based in San Diego, has witnessed the growing demand first-hand. “The number of researchers adopting this approach with different requirements for sensitivity, data analyses and visualization is drastically increasing,” he says.
In the past ten years, there has been an exponential growth in the number of publications using single-cell sequencing technologies. “Illumina’s sequencing technologies are able to meet customers’ diverse requirements whilst providing the highest quality single-base read, which is terribly important when dealing with single cells,” Hoffman explains.
However, transforming the vast amount of data generated by single-cell sequencing technologies into useful information remains an important challenge. Novel bioinformatic approaches that ensure the accuracy and reproducibility of results will aid data interpretation and, says Hoffman, help single-cell sequencing technologies transition beyond the R&D space and into the clinic. “As single-cell methods are applied to clinical samples and become integrated into large-scale clinical trials, we hope they will start informing treatment decisions in the not too distant future.”



 Decoding the signs of response to cancer immunotherapy
Decoding the signs of response to cancer immunotherapy
 Cancer neoantigens provide new research leads for personalized vaccine development
Cancer neoantigens provide new research leads for personalized vaccine development
 Polygenic risk: What’s the score?
Polygenic risk: What’s the score?
 Beyond GWAS: Tackling the variant-to-function challenge
Beyond GWAS: Tackling the variant-to-function challenge