ASC-US
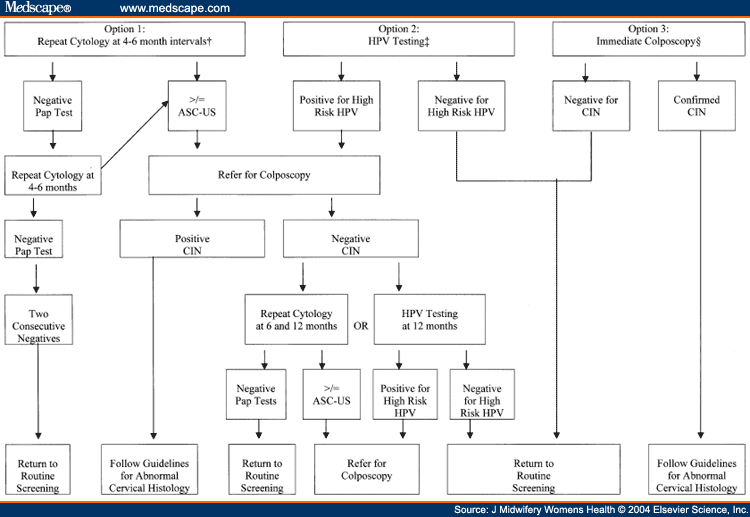
Following a routine Pap result of ASC-US, there are three options for patient management: 1) referral for colposcopy, 2) repeat cytology, or 3) HPV testing for high-risk strains (Figure 2). HPV DNA testing is the preferred approach when performed as a reflex test of liquid-based sample or when a co-collected sample is obtained during the initial Pap test.[15]
Figure 2.
Triage of women with ASC-US Pap test results.
*Management of pregnant women and non-pregnant women is the same.
†For postmenopausal women, cytology may be repeated approximately 1 week after a course of intravaginal estrogen.
‡HPV testing is the preferred approach when liquid-based cytology or co-collection of HPV sample is performed.
§Recommended for immunosuppressed women.
Many clinicians prefer immediate referral for colposcopy following an ASC-US result, arguing that a more conservative approach may result in delayed or missed diagnosis of significant disease and loss to follow-up. This is based on the rationale that a small percentage of women with ASC-US harbor underlying moderate to severe CIN.[19,20] Universal referral for colposcopy is a clinically aggressive approach to women with ASC-US. Although highly sensitive (96%) in revealing significant disease, other providers think colposcopy is impractical and expensive, especially considering the high prevalence of ASC-US and spontaneous regression rate of approximately 90%. Prevention of unnecessary inconvenience, anxiety, and discomfort is an important consideration. This interventionist approach confers the potential for unnecessary overdiagnosis and overtreatment of many healthy women. Immediate colposcopy is recommended for women with immune suppression.[2,3,15]
Repeat cytological testing is another common approach to ASC-US follow-up. The sensitivity of a single repeat Pap test is low, at 67% to 85% in several studies using liquid-based cytology. As a result, providers often choose to repeat the test at specified intervals. Women then return to routine screening after two or more consecutive negative results or are referred for colposcopy if the abnormality persists. This method of follow-up is based on the reasoning that many women with ASC-US have either no lesion or have HPV-related mild CIN, which is likely to regress.[15,16,17,18,19,20]
ASC-US follow-up with serial cytologic screening has several disadvantages. There are few data to support or define appropriate timing intervals for repeat Paps or the number of repeat tests necessary. Furthermore, this algorithm often requires several follow-up office visits and can delay discovery of serious disease for the 5% to 17% women with ASC-US who have underlying moderate to severe CIN. Non-adherence to recommendations for repeat testing and loss to follow-up also present problems. Colposcopy is indicated for a subsequent Pap test finding of ASC-US or other abnormality of greater significance. As a result, 32% to 59% of women will ultimately be referred for colposcopy.[15,16,17,18]
Results from a recent survey of nearly 500 American College of Obstetricians and Gynecologists fellows illustrate the lack of consensus and controversy regarding management of patients with ASC-US Pap results. Twenty-three percent of those surveyed chose colposcopic follow-up after the first mildly abnormal result, whereas 23% chose to rescreen within 3 months and 52% chose to rescreen in 3 to 6 months.[20] It is evident the threshold for colposcopy and cytologic evaluation is not well defined, lending further support to the need for adjunct or alternative screening tests for cervical cancer. Careful consideration must be given to triage and follow-up of women with ASC-US to successfully identify and diagnose the small number who are at risk with a true cancer precursor.[18]
Since the development of HPV DNA testing, this approach has been under intense study to evaluate its role in the triage and treatment of women with irregular cervical cytology. Two landmark clinical trials have been critical in demonstrating the value of HPV testing in ASC-US follow-up. The first, by Kaiser Permanente[17] with a sample of 995 women, compared follow-up with HPV testing to repeat Pap test screening using liquid cytology. The HPV test had greater sensitivity for detection of HSIL and cancer (89%) than a repeat Pap test (76%) and resulted in approximately the same number of referrals for colposcopy (40%).[17] The second landmark study, the ALTS trial, followed 3,488 women and reported that HPV testing demonstrated sensitivity for severe CIN over 96%, referring 54% of women for colposcopy. In comparison, liquid-based cytology with an ASC-US threshold for referral was only 86% sensitive and referred 59% of women for colposcopy.[51] In both studies, HPV testing for women with ASC-US was more highly sensitive and resulted in significantly fewer colposcopy referrals than follow-up with repeat cytology.
HPV testing has proved to be most useful in determining appropriate triage of women with ASC-US. These and other studies illustrate that HPV testing for high-risk viral strains is more sensitive in detecting moderate and severe CIN (89%100%) than a single liquid-based or conventional repeat Pap.[15,16,17,18] Just one HPV test is comparable to two serial Pap tests for detection of high-grade squamous intraepithelial lesions.[18] With a negative predictive value of 98% or more, a negative HPV test result proves to be more definitive in reassuring both patient and provider that no significant lesion is present.[15]
Several investigators have addressed the cost of HPV testing in the clinical setting, but few have examined the HPV test in the broad context of the newly released guidelines.[19,42,49] Investigation of ASC-US follow-up costs indicates that immediate colposcopy is the most expensive approach and reflex HPV testing is the least expensive, due to elimination of a follow-up office visit. Overall, compared with colposcopy and repeat cytology, reflex HPV is the most cost-effective strategy for women with ASC-US while conferring the same or greater health benefits.[19]
Numerous sources indicate that 31% to 60% of women with ASC-US will test positive for high-risk HPV.[15,16,17,18] According to the new guidelines, these patients should be referred for colposcopic evaluation. Considering the drawbacks of Pap slide interpretation, decreased sensitivity, and the time line required to perform serial cytology, HPV testing is a quicker and more objective triage approach, resulting in approximately the same or fewer referrals for colposcopy as repeat cytology. Reflex HPV testing of liquid-based cytology specimens or HPV cocollection at the time of initial screening eliminates the cost, inconvenience, anxiety, and discomfort of return office visits and repeat speculum exams; thus, it is the preferred approach for follow-up of an ASC-US Pap test.[15]
J Midwifery Womens Health. 2004;49(1) © 2004 Elsevier Science, Inc.
Cite this: The Role of Human Papilloma Virus Testing in Cervical Cancer Prevention - Medscape - Jan 01, 2004.





Comments