Research by scientists at the University of Campinas (UNICAMP) in Brazil has demonstrated how treatment using an antibacterial drug can boost metabolism and attenuate weight gain induced by a fatty diet in experimental mice. The studies, headed by Marcelo Mori, PhD, a professor at the university’s Biology Institute (IB-UNICAMP), showed that treatment with the broad-spectrum fluoroquinolone antibiotic enoxacin, triggered the animals’ white adipose tissue (WAT)—which normally stores surplus energy as fat—to behave like brown adipose tissue (BAT), by burning calories to generate heat (thermogenesis). This phenomenon, known as browning, was observed only when the animals were exposed to cold. The effects were similarly seen in vitro in both mouse and human cell models, and were linked to changes in microRNA (miRNA) production. The researchers are now looking for compounds that are structurally similar to enoxacin, for further development.
“The purpose of the study was to prove a principle, to show that it’s possible to increase energy expenditure and reduce the harmful consequences of obesity by acting pharmacologically on a metabolic pathway of interest,” Mori said. “We are not proposing use of this specific drug to combat weight gain. Our results point to ways of finding compounds that act on the same pathway more effectively and safely.”
Mori and an international team of collaborators reported on their findings in Science Advances, in a paper titled, “Enoxacin induces oxidative metabolism and mitigates obesity by regulating adipose tissue miRNA expression.”
Obesity affects more than 600 million people worldwide, the authors wrote. The condition effectively results from an imbalance between the amount of food consumed, and energy expenditure, leading to accumulation of the excess energy as lipids in adipocytes, the authors wrote. To date, the most effective and well-characterized potential approaches to boosting energy expenditure in rodents, and potentially in humans, include β-adrenergic pathway stimulators, and peroxisome proliferator–activated receptor γ (PPAR γ) agonists. However, the authors wrote, despite having promising effects on browning and energy expenditure, such drugs can have serious side-effects.
Mori said that some of these drugs excessively stimulate the adrenergic system, which regulates the fight-or-flight response to threats and can cause cardiac arrhythmia and even a heart attack. Others are even more dangerous, chemically uncoupling the inner mitochondrial membrane and increasing cellular energy expenditure. “The problem with current interventions is that they have systemic effects, acting on various cell types including even neurons and cardiomyocytes,” Mori said. “They can cause cell death and affect important processes in the organism.”
MicroRNAs (miRNAs) are small endogenous noncoding RNAs that target sequences within mRNAs to inhibit their translation and/or induce their degradation, and “… emerging evidence has suggested that miRNAs play essential roles in brown/beige adipocyte determination and function,” the scientists commented. “Previous studies in animal models and humans indicated that interventions capable of extending longevity and improving metabolic health, such as physical exercise and caloric restriction, promote this benefit by increasing adipose tissue’s capacity to process mirRNAs,” Mori continued. “In other words, these practices modulate the pathway responsible for miRNA biogenesis.”
For their newly reported studies, the team focused on the drug enoxacin, “ … a broad-spectrum antibacterial fluoroquinolone that has been shown to interfere with miRNA processing in eukaryotic cells.” While enoxacin has not been used in clinical practice since the emergence of more effective fluoroquinolone antibiotics some years ago, previous studies have shown that the drug can modulate the production of microRNAs in adipose tissue.
To investigate the effects of enoxacin on thermogenesis, the team carried out a series of in vitro studies in human and mouse preadipocytes—cells that store fat when mature and become part of white adipose tissue—and also tested enoxacin in experimental mice fed a high-fat diet.
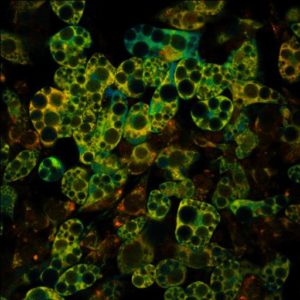
In the laboratory, cellular differentiation of preadipocytes into mature adipocytes takes about eight days and can be induced by a cocktail of chemicals and hormones. In one set of tests the researchers added enoxacin to the mix of differentiation factors, and at the end of the process compared the mature adipocytes with those in a control culture that hadn’t been exposed to enoxacin. The analysis showed that in white adipocytes the drug triggered expression of PPARGC1A and UCP1, genes that are significantly active in brown adipose tissue cells under normal circumstances. The proteins encoded by these two genes are considered molecular markers of thermogenesis. The researchers reasoned that enoxacin induced browning by reprogramming the white adipose cells to dissipate energy in the form of heat instead of storing it as fat.
“The protein UCP1 acts on mitochondria by uncoupling the electron transport chain used in the synthesis of ATP …” Mori said. “This makes the cells dissipate energy as heat. To understand the process better, we can compare it to the damming of a river to produce electricity. If holes are made in the dam, the difference in elevation that should be used to drive the turbine is dissipated without generating the desired energy.”
In the second set of in vitro tests, the differentiated adipocytes were exposed to enoxacin for 24 hours and then analyzed. The researchers found that the cells expressed the same markers of thermogenesis, showing that the white adipocytes now formed had also undergone browning. Functional tests indicated that both antibiotic treatment protocols led the white adipocytes to consume more oxygen than the untreated cells, even under the same conditions.”
The team also carried out a series of experiments in mice. “Since miRNAs have been involved in energy metabolism, we tested whether enoxacin treatment influences key regulators of thermogenesis and oxidative phosphorylation in vivo,” they wrote. Animals were treated using enoxacin administered by intraperitoneal injection, as oral administration of an antibiotic could alter the normal gut microbiota and interfere with the results. The team carried out several experiments. In one, the rodents were fed a high-fat diet (HFD) for a month before starting the treatment with enoxacin. The mice were then given the drug once a day from Monday to Friday for ten weeks, and the fatty diet was maintained throughout the period. At the end of the treatment period, the researchers found that while the placebo-treated control animals gained 13 g in weight on average, those treated with the antibiotic gained only 8 g. “Mice treated with enoxacin gained 31% less weight on HFD in comparison to vehicle-treated mice,” the authors noted. “This was accompanied by reduced WAT mass and no changes in BAT mass.”
Mori further commented, “The weight gain curve began diverging between the two groups as soon as administration of the drug began. The control group’s weight gain continued to rise strongly, while the treated group’s curve became less steep. At the end, we found the treatment also led to enhanced insulin sensitivity and glucose tolerance.”
As the authors noted, “Consistent with reduced adiposity, enoxacin treatment decreased fasting glucose levels, improved glucose tolerance, and increased insulin sensitivity, although no differences were observed in insulin levels.” Further analysis of the animals’ adipose tissue evidenced increased expression of thermogenesis marker genes PPARGC1A and UCP1 in both white and brown adipose cells.
However, the beneficial effect on the metabolism was observed only when the mice were exposed to mild cold stress (about 24° C) or severe cold stress (in the range of 6° C). “Enoxacin-treated mice were more thermotolerant than the vehicle group in both acute (within 6 hours of cold exposure; when thermogenesis is largely sustained by activation of pre-existing brown and beige adipocytes) and chronic (24 to 72 hours of cold exposure, when new beige adipocytes are recruited) challenges,” they wrote. “BAT of enoxacin-treated mice was browner and expressed higher levels of thermogenic genes … Together these results demonstrate that enoxacin potentiates the effect of cold to promote browning and activate thermogenesis …”
In contrast, when thermoneutrality was maintained (about 30° C, the ideal temperature for these mice), enoxacin was not found to be capable of activating thermogenesis, indicating that the drug intensified the action of cold. “The fact that the drug doesn’t work in thermoneutrality reduces its potential for use as a sole treatment for obesity, but it can help us understand the mechanisms involved in the process or be used as an adjuvant,” Mori acknowledged. “In any event, we expect to find a molecule with even more powerful thermogenic action and without the side-effects of an antibiotic.”
To find out whether the effect observed in the mice exposed to mild cold stress depended on the drug’s action on gut bacteria, which are known to influence weight gain, the researchers repeated the experiment using germ-free mice that had been bred under controlled laboratory conditions to be totally free of microbiota. The results showed that enoxacin also promoted thermogenesis in these animals. “Together, these results indicate that enoxacin mitigates diet-induced obesity and insulin resistance by a mechanism that does not involve changes in energy intake, energy loss, or depletion of the gut microbiota,” they wrote. “Our study shows that enoxacin induces energy expenditure in mice and counteracts diet-induced obesity. These effects are related to the activation of BAT, induction of browning in scWAT, and up-regulation of oxidative metabolism in skeletal muscle.”
The investigators in addition sequenced all the miRNAs expressed in the adipose tissue of the treated mice, as well as in adipose tissue from the control mice. The initial analysis showed that enoxacin treatment altered the expression of a few dozen miRNAs. “We cross-tabulated our results with data from public repositories in search of miRNAs regulated by both enoxacin and other interventions that induce browning,” Mori explained. “We eventually arrived at miR-34a-5p, which is consistently modulated both by the drug and by caloric restriction and cold stress.” Enoxacin may interfere in the processing and stability of miR-34a-5p, he added. Because it suppresses signaling by hormones, including FGF21, which promotes energy expenditure, a reduction in miR-34a-5p intensifies the thermogenic stimulus.
In their published paper, the team concluded, “Here, we provide proof-of-principle, preclinical evidence for a new class of drugs capable of promoting oxidative metabolism and inducing uncoupled respiration in adipose tissues and skeletal muscle, at least in part, by interfering with miRNA biogenesis.”
Researchers at AstraZeneca collaborated with Mori’s group for the reported studies, and on the basis of the findings, UNICAMP and the pharmaceutical company are testing molecules with similar structures to enoxacin but without antibacterial effects. In vitro experiments have had promising results, pointing to compounds with even stronger thermogenic action than the original molecule and without the antimicrobial effects.


