Abstract
Background:
The Prostate Health Index (phi) outperforms PSA and other PSA derivatives for the diagnosis of prostate cancer (PCa). The impact of phi testing in the real-world clinical setting has not been previously assessed.
Methods:
In a single, large, academic center, phi was tested in 345 patients presenting for diagnostic evaluation for PCa. Findings on prostate biopsy (including Grade Group (GG), defined as GG1: Gleason score (GS) 6, GG2: GS 3+4=7, GG3: GS 4+3=7, GG4: GS 8 and GG5: GS 9–10), magnetic resonance imaging (MRI) and radical prostatectomy (RP) were prospectively recorded. Biopsy rates and outcomes were compared with a contemporary cohort that did not undergo phi testing (n=1318).
Results:
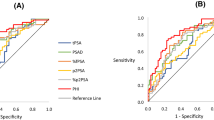
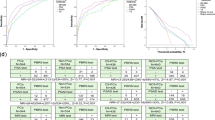
Overall, 39% of men with phi testing underwent prostate biopsy. No men with phi<19.6 were diagnosed with PCa, and only three men with phi<27 had cancer of GG⩾2. Phi was superior to PSA for the prediction of any PCa (area under the receiver operating characteristic curve (AUC) 0.72 vs 0.47) and GG⩾2 PCa (AUC 0.77 vs 0.53) on prostate biopsy. Among men undergoing MRI and phi, no men with phi<27 and PI-RADS⩽3 had GG⩾2 cancer. For those men proceeding to RP, increasing phi was associated with higher pathologic GG (P=0.002) and stage (P=0.001). Compared with patients who did not undergo phi testing, the use of phi was associated with a 9% reduction in the rate of prostate biopsy (39% vs 48%; P<0.001). Importantly, the reduction in biopsy among the phi population was secondary to decreased incidence of negative (8%) and GG1 (1%) biopsies, whereas the proportion of biopsies detecting GG⩾2 cancers remained unchanged.
Conclusions:
In this large, real-time clinical experience, phi outperformed PSA alone, was associated with high-grade PCa, and provided complementary information to MRI. Incorporation of phi into clinical practice reduced the rate of unnecessary biopsies without changing the frequency of detection of higher-grade cancers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
American Cancer Society. Cancer facts & Figures. 2014. (http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf).
Cooperberg MR, Moul JW, Carroll PR . The changing face of prostate cancer. J Clin Oncol 2005; 23: 8146–8151.
Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Zappa M, Nelen V et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014; 6736: 1–9.
Loeb S, Bjurlin MA, Nicholson J, Tammela TL, Penson DF, Carter HB et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol 2014; 65: 1046–1055.
Tosoian J, Loeb S . PSA and beyond: the past, present, and future of investigative biomarkers for prostate cancer. ScientificWorldJournal 2010; 10: 1919–1931.
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R et al. Systematic review of complications of prostate biopsy. Eur Urol 2013; 64: 876–892.
Jansen FH, van Schaik RHN, Kurstjens J, Horninger W, Klocker H, Bektic J et al. Prostate-specific antigen (PSA) isoform p2PSA in combination with total psa and free psa improves diagnostic accuracy in prostate cancer detection. Eur Urol 2010; 57: 921–927.
Le BV, Griffin CR, Loeb S, Carvalhal GF, Kan D, Baumann NA et al. [-2]Proenzyme prostate specific antigen is more accurate than total and free prostate specific antigen in differentiating prostate cancer from benign disease in a Prospective Prostate Cancer Screening Study. J Urol 2010; 183: 1355–1359.
Stephan C, Vincendeau S, Houlgatte A, Cammann H, Jung K, Semjonow A . Multicenter evaluation of [-2]proprostate-specific antigen and the Prostate Health Index for detecting prostate cancer. Clin Chem 2013; 59: 306–314.
Foley RW, Gorman L, Sharifi N, Murphy K, Moore H, Tuzova A V et al. Improving multivariable prostate cancer risk assessment using the Prostate Health Index. BJU Int 2016; 117: 409–417.
Filella X, Giménez N . Evaluation of [-2] proPSA and Prostate Health Index (phi) for the detection of prostate cancer: a systematic review and meta-analysis. Clin Chem Lab Med 2013; 51: 729–739.
Bruzzese D, Mazzarella C, Ferro M, Perdonà S, Chiodini P, Perruolo G et al. Prostate Health Index vs percent free prostate-specific antigen for prostate cancer detection in men with ‘gray’ prostate-specific antigen levels at first biopsy: systematic review and meta-analysis. Transl Res 2014; 164: 444–451.
de la Calle C, Patil D, Wei JT, Scherr DS, Sokoll L, Chan DW et al. Multicenter evaluation of the Prostate Health Index to detect aggressive prostate cancer in biopsy naïve men. J Urol 2015; 194: 65–72.
Lazzeri M, Haese A, de la Taille A, Palou Redorta J, McNicholas T, Lughezzani G et al. Serum isoform [−2]proPSA derivatives significantly improve prediction of prostate cancer at initial biopsy in a total PSA range of 2–10 ng/ml: a Multicentric European Study. Eur Urol 2013; 63: 986–994.
Loeb S, Sanda MG, Broyles DL, Shin SS, Bangma CH, Wei JT et al. The Prostate Health Index selectively identifies clinically significant prostate cancer. J Urol 2015; 193: 1163–1169.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA . The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason Grading of Prostatic Carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 2016; 40: 244–252.
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C et al. A Contemporary Prostate Cancer Grading System: a validated alternative to the Gleason Score. Eur Urol 2015; 69: 428–435.
Catalona WJ, Partin AW, Sanda MG, Wei JT, Klee GG, Bangma CH et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J Urol 2011; 185: 1650–1655.
Cantiello F, Russo GI, Ferro M, Cicione A, Cimino S, Favilla V et al. Prognostic accuracy of Prostate Health Index and urinary prostate cancer antigen 3 in predicting pathologic features after radical prostatectomy. Urol Oncol 2015; 33: 163.e15–23.
Guazzoni G, Nava L, Lazzeri M, Scattoni V, Lughezzani G, Maccagnano C et al. Prostate-specific antigen (PSA) isoform p2PSA significantly improves the prediction of prostate cancer at initial extended prostate biopsies in patients with total PSA between 2.0 and 10 ng/ml: results of a prospective study in a clinical setting. Eur Urol 2011; 60: 214–222.
Porpiglia F, Russo F, Manfredi M, Mele F, Fiori C, Bollito E et al. The roles of multiparametric magnetic resonance imaging, PCA3 and Prostate Health Index-which is the best predictor of prostate cancer after a negative biopsy? J Urol 2014; 192: 60–66.
Tosoian JJ, Ross AE, Sokoll LJ, Partin AW, Pavlovich CP . Urinary biomarkers for prostate cancer. Urol Clin North Am 2016; 43: 17–38.
Nichol MB, Wu J, Huang J, Denham D, Frencher SK, Jacobsen SJ . Cost-effectiveness of Prostate Health Index for prostate cancer detection. BJU Int 2012; 110: 353–362.
Acknowledgements
AER is supported by a DOD PRTA award (W81XWH-13-1-0445) as well as a PCF Young Investigator Award and Patrick C. Walsh Investigator Grant. EMS is supported by NIH U01CA196390-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tosoian, J., Druskin, S., Andreas, D. et al. Use of the Prostate Health Index for detection of prostate cancer: results from a large academic practice. Prostate Cancer Prostatic Dis 20, 228–233 (2017). https://doi.org/10.1038/pcan.2016.72
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.72
This article is cited by
-
Relationships between holmium laser enucleation of the prostate and prostate cancer
Nature Reviews Urology (2023)
-
Prostate health index (PHI) as an accurate prostate cancer predictor
Journal of Cancer Research and Clinical Oncology (2023)
-
Liquid biomarkers for early detection of prostate cancer and summary of available data for their use in African-American men
Prostate Cancer and Prostatic Diseases (2022)
-
The Prostate Health Index aids multi-parametric MRI in diagnosing significant prostate cancer
Scientific Reports (2021)
-
Combining prostate health index and multiparametric magnetic resonance imaging in the diagnosis of clinically significant prostate cancer in an Asian population
World Journal of Urology (2020)