Abstract
Introduction
Spinal epidural abscesses are most commonly treated with surgical decompression and antibiotics or in specific instances managed medically with antibiotic therapy alone. Image-guided percutaneous aspiration as an alternative to surgery has only rarely been reported in the literature.
Case presentation
We report two cases of successful fluoroscopy-guided needle aspiration of posterior epidural abscesses. Case 1 is a 48-year-old man who presented with several days of escalating back pain and constitutional symptoms with MRI showing a posterior epidural abscess at L2–L3 causing spinal stenosis. The patient remained neurologically intact. Percutaneous needle aspiration of the collection provided dramatic pain relief with the aspirate growing methicillin sensitive Staphylococcus aureus. The patient made a full recovery on antibiotic therapy. Case 2 is an 81-year-old man who presented with worsening upper back pain and was found to have osteomyelitis/discitis with a large posterior epidural abscess in the thoracic spine. Needle drainage was performed with the sample growing Bacteroides fragilis. This patient also responded successfully to nonsurgical management with full recovery after appropriate antibiotic therapy.
Discussion
In carefully selected patients, image-guided needle aspiration of posterior epidural abscesses may be a viable and less invasive alternative to surgery.
Similar content being viewed by others
Introduction
Spinal epidural abscesses are an uncommon but serious condition that require prompt diagnosis and management to prevent long-term neurologic compromise. Traditional risk factors include intravenous drug use, diabetes mellitus, epidural injection or catheter placement, and spinal instrumentation [1, 2]. The initial clinical presentation may be non-specific, and diagnosis is often delayed [3, 4]. The symptoms and physical exam findings of spinal epidural abscesses are divided into four clinical stages: stage (1) back pain at the site of infection; stage (2) radicular pain emanating from the involved spinal segment; stage (3) motor weakness or other neurologic deficit; and stage (4) paralysis [2]. Treatment is most commonly surgical decompression and drainage with long term antibiotic therapy [5, 6]. Tissue and fluid samples obtained during surgical treatment can guide antibiotic choice. Staphylococcus aureus is the most common causative organism, followed by other skin flora such as Streptococcal species, although a wide variety of organisms have been reported [2, 7, 8].
In specific instances, surgery may be relatively contraindicated and medical management with long-term antibiotic therapy pursued [9, 10]. This may include when surgical risk is unacceptably high, patients who refuse surgery, patients with small epidural abscesses and stage 1 or stage two symptoms, or in patients with prolonged paralysis that is unlikely to be reversed by surgery. In these circumstances, image-guided needle aspiration of the abscess serves several purposes. Fluid sampling allows culture results to guide antibiotic therapy, decompression of the abscess may accelerate relief of pain, and drainage can assist with local source control of infection increasing the likelihood of successful conservative therapy and avoiding the morbidity of surgery. Despite this, abscess aspiration under fluoroscopy or computed tomography (CT) has only been described in a few published case reports [11,12,13]. In the current report, we describe two patients with spinal epidural abscesses who were successfully treated with fluoroscopy-guided percutaneous abscess aspiration and antibiotic therapy without surgery.
Case reports
Case number one is a 48-year-old man who presented to our institution’s Emergency Department with a 7-day history of rapidly worsening back pain that radiated into his legs. He had been evaluated in urgent care a few days earlier and prescribed cyclobenzaprine for presumed back spasm but had received no antibiotics prior to his presentation in the Emergency Department. He described episodes of sweating and subjective fevers but denied any lower extremity weakness. He was obese but otherwise healthy without co-morbidities and did not have a history of intravenous drug use. On physical exam, he maintained full 5/5 strength in both the upper and lower extremities. Sensation to light touch was maintained and long tract reflexes were normal. Straight leg raise test was positive. Temperature at presentation was 37.9 degrees Celsius. Laboratory evaluation showed a mild leukocytosis with white blood cell count of 12 and elevated inflammatory markers with ESR of 105 and CRP of 40. MRI of the lumbar spine with and without contrast demonstrated a rim enhancing fluid collection in the posterior epidural space at the L2–L3 level with resulting spinal canal stenosis (Fig. 1). As the patient was neurologically intact and the abscess was small and accessible in the posterior epidural space, nonsurgical management was pursued. Aspiration of the collection was performed under fluoroscopic guidance (Fig. 2) yielding two milliliters of purulent fluid. Antibiotics were held prior to aspiration to maximize the yield of culture. Immediately after the procedure broad spectrum antibiotic coverage with IV cefepime and vancomycin was started. Culture results returned methicillin-sensitive Staphylococcus aureus and coverage was narrowed to IV oxacillin by hospital day three. The patient’s pain improved rapidly within the 48 h following aspiration and he remained neurologically intact. He was discharged on a 6-week course of IV oxacillin followed by 6 weeks of step-down therapy on oral dicloxacillin. Although he briefly required narcotic pain medication during his hospitalization, by time of discharge his pain was well controlled with ibuprofen and Tylenol. Follow up MRIs showed decreasing size of the collection with eventual resolution (Fig. 3).
A 48-year-old man (patient 1) with fever and back pain. Sagittal T2 fat-suppressed (a), sagittal T1 fat-suppressed post-contrast (b), axial T1 fat-suppressed post-contrast (c). MR images of the lumbar spine demonstrate a rim enhancing fluid collection in the posterior epidural space (arrowheads) at the L2–L3 level with associated spinal canal stenosis
A follow up MRI in patient 1 obtained 6 months after presentation. Sagittal T2 fat-suppressed (a) and sagittal T1 fat-suppressed post-contrast MR images of the lumbar spine demonstrate complete resolution of the abscess collection. A small amount of residual enhancing inflammatory tissue is present in the L2–L3 interlaminar space (arrowheads in b)
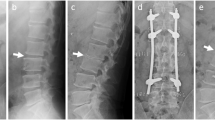
Case number two is an 81-year-old man who presented to the Veterans Affairs Hospital Emergency Department with gradually progressive upper back pain and constitutional symptoms that developed insidiously over a 3-week period prior to admission. He had not been previously evaluated for these symptoms. He had multiple co-morbidities including heart disease, diabetes mellitus, prior thromboembolic stroke, and atrial fibrillation on anti-coagulation therapy. His medications included narcotics for chronic pain, but he had not received antibiotics prior to admission. At presentation he was afebrile. On physical exam, he had full 5/5 strength in the upper and lower extremities. Sensation to light touch was maintained in all distributions. Patellar reflexes could not be elicited on either side but upper extremity reflexes including biceps and triceps were intact. Straight leg raise test was not performed. There were no gait abnormalities. Initial laboratory evaluation demonstrated a white blood cell count of 5 and elevated CRP and ESR at 10 and 120, respectively. An MRI of the thoracic spine with and without contrast demonstrated an elongated rim enhancing fluid collection in the posterior epidural space crossing multiple levels in the thoracic spine as well as findings of osteomyelitis and discitis at T6–T7 (Fig. 4). His medical co-morbidities placed him at increased surgical risk, and he had no neurologic deficit on physical exam. For these reasons, the decision was made to trial nonsurgical management with close monitoring. His anti-coagulation was reversed, and fluoroscopy-guided aspiration of the posterior epidural collection was performed at the T3–T4 interspinous level targeting the largest portion of the fluid collection posterior to the T3 vertebral body (Fig. 5). Aspiration yielded four milliliters of purulent fluid. Similar to the first patient, he was immediately started on broad-spectrum antibiotics following the procedure with IV cefepime and vancomycin and his neurologic exam monitored closely. The aspirate grew Bacteroides fragilis and his antibiotic coverage was narrowed to IV Meropenem. The patient’s upper back pain gradually improved following aspiration and he suffered no neurologic deficit. His recovery was gradual, requiring a hospitalization of several weeks but he was eventually discharged and continued on a prolonged course of outpatient antibiotic therapy including a total of 12 weeks of IV Meropenem and a short 2-week course of step-down therapy with oral Augmentin. His upper back pain had resolved by discharge although he continued on his previous outpatient narcotic prescription for his pre-existing chronic joint pain. His white blood cell count normalized within a few days of starting treatment. His ESR and CRP declined more gradually but had normalized prior to the end of his antibiotic course. Given his complete clinical recovery, his managing physician opted not to obtain follow up imaging.
An 81-year-old man (patient 2) with escalating upper back pain and constitutional symptoms. Sagittal T2 fat-suppressed (a), sagittal T1 fat-suppressed post-contrast (b), axial T1 fat-suppressed post-contrast (c), and axial T2 MR images of the thoracic spine demonstrate edema and enhancement centered at the T6 and T7 vertebral bodies compatible with osteomyelitis/discitis (arrow in a and b). There is an elongated, rim-enhancing fluid collection in the posterior epidural space extending across much of the upper thoracic spine (arrowheads in a and b). The axial plane images demonstrate the location of the abscess collection in the midline posterior epidural space (arrowheads in c and d) and show the associated spinal canal stenosis
Discussion
We report two cases of patients with spinal epidural abscesses who were successfully treated with image-guided percutaneous drainage and antibiotic therapy thus avoiding the need for surgery. Both of our patients had no neurologic deficits on exam and had epidural abscesses that were in the posterior epidural space where they were accessible for aspiration. In patient number one, the small size of the collection and his overall stability allowed image-guided aspiration to be pursued as a less invasive option to surgery. Patient number two was at elevated surgical risk because of his co-morbidities and was also without neurologic deficit. The neurologic status of both patients was monitored carefully following the procedure. Developing neurologic compromise would be an indication for rapid surgical decompression.
Image-guided aspiration of posterior epidural abscesses should be performed by personnel experienced in accessing the epidural space. If possible, antibiotics should be held prior to the procedure to maximize culture yield. Broad spectrum antibiotics can be started immediately post-procedure and coverage narrowed when culture data is available. Any coagulopathy should be reversed. At our institution we typically perform these procedures with conscious sedation unless the patient’s co-morbidities are serious enough to warrant general anesthesia. Either fluoroscopy or CT can be used for intra-procedural imaging guidance based on the preference of the interventionalist [12, 14, 15]. At our institution we typically use fluoroscopy, but CT may be useful when hypertrophic bone from degenerative spondylosis makes interlaminar access more challenging or for interventionalists who are accustomed to gaining epidural access with CT guidance. Ultrasound may be useful for the drainage of abscess collections in the posterior paraspinal soft tissues but is not helpful for accessing the epidural space. Pre-operative imaging should be carefully reviewed to plan the approach and to determine the optimal imaging modality for procedure guidance. For the procedure, the patient is placed prone on the fluoroscopic table with the aid of a bolster to widen the interlaminar space. If the interspinous space is wide enough, a midline approach is straightforward as was used in both of these cases. If the interspinous space is too narrow, a paramedian approach is an alternative and the side can be chosen based on the patient’s anatomy and the location of the collection. A larger bore 20 g or 18 g needle should be used as abscess contents are likely to be viscous. After standard skin preparation and local anesthesia, the needle is advanced into the posterior epidural space under careful fluoroscopic control using the loss of resistance technique. Advancing the needle too deeply and entering the subarachnoid space may result in spread of infection and meningitis, a serious complication that should be avoided by thorough pre-procedural review of the patient’s imaging, cautious needle advancement, and monitoring of needle depth on the lateral fluoroscopic view. Once the epidural space is accessed, aspiration can be performed. Some authors advocate use of a two-needle technique and possible placement of an epidural catheter with saline irrigation of the epidural space [13]. Other techniques include the placement of multiple needles and irrigation with antibiotic solution [14]. Post-procedural care should include meticulous monitoring of the patient’s neurologic exam, appropriate wound care, and monitoring of any catheters left in situ.
It should be emphasized that in the majority of patients, surgical decompression and drainage often remains as the first line treatment. Nonsurgical management can be considered in patients with no neurologic deficits and when surgery is unacceptably invasive or risky as a first line approach. This may include patients with high-risk comorbidities, pediatric patients, or stable patients with early stage symptoms [16]. In this context, needle abscess drainage of accessible posterior epidural collections may play an important supportive role both in identifying the causative organism for targeted antibiotic therapy and providing source control at the site of infection. This may increase the likelihood of successful medical management [14]. Treatment of these complex patients requires a well-coordinated multidisciplinary team. Because urgent surgical decompression may be warranted if clinical or neurological deterioration should occur despite aspiration, a spinal surgeon should be involved early in the course. The infectious disease physician can provide guidance on appropriate initial broad-spectrum empiric antibiotic coverage as well as managing the patient’s long-term targeted antibiotic therapy.
The spinal epidural abscess is an uncommon but serious condition with a high risk of neurologic morbidity and even mortality unless promptly diagnosed and treated. Although surgical decompression remains the mainstay of treatment for most patients, image-guided percutaneous needle aspiration is a viable alternative that can be considered in a subset of patients and should be considered part of the treatment armamentarium for clinicians managing this condition.
References
Pereira CE, Lynch JC. Spinal epidural abscess: an analysis of 24 cases. Surg Neurol. 2005;63(Suppl 1):S26–9.
Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006;355:2012–20.
Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC, et al. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004;26:285–91.
Mackenzie AR, Laing RB, Smith CC, Kaar GF, Smith FW. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry. 1998;65:209–12.
Curry WT Jr., Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: clinical presentation, management, and outcome. Surg Neurol. 2005;63:364–71.
Rigamonti D, Liem L, Sampath P, Knoller N, Namaguchi Y, Schreibman DL, et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999;52:189–96.
Suppiah S, Meng Y, Fehlings MG, Massicotte EM, Yee A, Shamji MF. How Best to manage the spinal epidural abscess? A current systematic review. World Neurosurg. 2016;93:20–8.
Kaufman DM, Kaplan JG, Litman N. Infectious agents in spinal epidural abscesses. Neurology. 1980;30:844–50.
Siddiq F, Chowfin A, Tight R, Sahmoun AE, Smego RA Jr. Medical vs surgical management of spinal epidural abscess. Arch Intern Med. 2004;164:2409–12.
Sorensen P. Spinal epidural abscesses: conservative treatment for selected subgroups of patients. Br J Neurosurg. 2003;17:513–8.
Walter RS, King JC Jr., Manley J, Rigamonti D. Spinal epidural abscess in infancy: successful percutaneous drainage in a nine-month-old and review of the literature. Pediatr Infect Dis J. 1991;10:860–4.
Tabo E, Ohkuma Y, Kimura S, Nagaro T, Arai T. Successful percutaneous drainage of epidural abscess with epidural needle and catheter. Anesthesiology. 1994;80:1393–5.
Perez-Toro MR, Burton AW, Hamid B, Koyyalagunta D. Two-tuohy needle and catheter technique for fluoroscopically guided percutaneous drainage of spinal epidural abscess: a case report. Pain Med. 2009;10:501–5.
Ran B, Chen X, Zhong Q, Fu M, Wei J. CT-guided minimally invasive treatment for an extensive spinal epidural abscess: a case report and literature review. Eur Spine J. 2018;27(Suppl 3):380–5.
Lyu RK, Chen CJ, Tang LM, Chen ST. Spinal epidural abscess successfully treated with percutaneous, computed tomography-guided, needle aspiration and parenteral antibiotic therapy: case report and review of the literature. Neurosurgery. 2002;51:509–12
Spernovasilis N, Demetriou S, Bachlitzanaki M, Gialamas I, Alpantaki K, Hamilos G, et al. Characteristics and predictors of outcome of spontaneous spinal epidural abscesses treated conservatively: a retrospective cohort study in a referral center. Clin Neurol Neurosurg. 2017;156:11–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ross, A.B., Tang, J.Y., Rosas, H.G. et al. Fluoroscopy-guided percutaneous needle aspiration of posterior epidural abscesses: a report of two cases. Spinal Cord Ser Cases 5, 43 (2019). https://doi.org/10.1038/s41394-019-0190-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-019-0190-z