Mammography and Other Radiologic Procedures: Appropriate Use and Interpretation
Routine mammography is generally not recommended in women younger than 30 years of age unless dictated by family history ( Table II ). This is because mammography is less likely to demonstrate occult lesions in young women, who tend to have dense breast tissue; further, radiation-exposure risks are higher in this age group than in older women.[22] Consequently, the benefits of mammography do not outweigh the risks in younger women unless the mass is clinically suspicious.
A mammogram should be performed in any woman older than age 30 in whom a palpable breast lump or thickening has been found. Although a mammogram cannot be used to distinguish whether a mass is cystic or solid, it is helpful in evaluating the breast tissue in the uninvolved portions of the breast and in the other breast.
Mammography can also help in characterizing the mass -- if it can be seen on the film. However, the false-negative rate of mammography ranges between 10% and 22%.[23,24,25] This rate can be as high as 30% to 35% in younger women[25] and is one of the most common clinical pitfalls cited by women who file a malpractice suit against a physician for failure to diagnose breast cancer. A false-negative result is usually due to dense breast tissue (Fig. 8).[1]
Mammogram demonstrating small infiltrating ductal carcinoma (note arrow). Film would have been interpreted as normal had density representing carcinoma been located nearer nipple, where breast tissue is dense. Reprinted with permission from Breast Imaging: A Guide for Clinicians, Slide Lecture Program: Slide 19, American College of Radiology Task Force on Breast Cancer.[27]
Dense breast tissue can be seen in premenopausal women, in postmenopausal women on HRT, and in some postmenopausal women who are not on HRT. For this reason, any palpable abnormality needs further workup, despite a normal mammogram.
After pregnancy, screening mammography is not recommended until a woman resumes menses. Diagnostic mammography can be done in lactating women, but the risk of a false negative may be higher than in women not lactating because of increased tissue density. However, the data do not definitely support this clinical recommendation. We, along with many others, question the clinical usefulness of this approach, except for women who have breast pain in luteal phase of their cycle. Cornelia Baines and her team[26] reported that mammograms taken during the luteal phase were twice as likely to be read as false-negative as were those taken during the follicular phase of the menstrual cycle (days 1 to 14).
Mammograms can be used to identify mass lesions, asymmetries, and microcalcifications. Radiologists often use the BI-RADS system developed by the American College of Radiology[27] to categorize mammograms, in addition to a narrative description of the characteristics of the image. The BI-RADS system assigns a mammogram to one of 5 categories:
Category I = Normal.
Category II = Benign-appearing abnormality.
Category III = Probably benign/possibly malignant.
Category IV = Suspicious for malignancy.
Category V = Malignant until proven otherwise.
If a mammogram is abnormal, it is critically important for the radiologist to be able to compare current findings with previous films. In addition, the radiologist often recommends additional mammographic views and/or ultrasound to further characterize the abnormality.
Cone compression is used to compress breast tissue selectively over the area where the mammographic abnormality is identified. This can differentiate superimposed breast tissue from a true abnormality. In palpable masses containing microcalcifications, magnification views may further characterize the lesion(s).
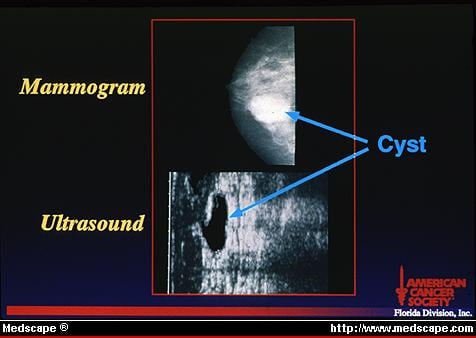
To distinguish cystic from solid masses, high-frequency ultrasound performed with a linear array transducer may be useful. A cyst appears round or oval with smooth walls and a dark or anechoic center (Fig. 9). In contrast, a solid mass will be echoic, that is, reflect the ultrasound waves. An ultrasound examination, however, may fail to visualize a palpable abnormality. As is the case with mammography, radiologists depend on tissue contrast to interpret films. If a lesion is isodense with surrounding tissue, it is not imaged by ultrasound, and a false-negative reading results. Therefore, any palpable abnormality warrants further evaluation, even with a normal ultrasound.
Breast cyst demonstrated by mammography and ultrasound. Generally, mammogram does not characterize whether mass is cystic or solid. By ultrasound, cyst appears round or oval with smooth walls and dark or anechoic center. Reprinted with permission from Love N: Primary Care Considerations in Breast Diagnosis, Slide Lecture Program: Slide 41, Copyright © 1992, American Cancer Society, Tampa, Florida Division, Inc.[6]
© 1999 Medscape
Cite this: Primary Care Guide to Managing a Breast Mass: Step-by-Step Workup - Medscape - Sep 01, 1999.







Comments