Eight scientists are poised to receive their doctorates and embark on careers tackling problems in human disease through biomedical research. Their years of dedication and training will be recognized on May 18, 2022, when they will be awarded their PhD degrees from the Gerstner Sloan Kettering Graduate School of Biomedical Sciences (GSK). This year’s commencement marks the school’s 11th graduating class since admitting its first students in 2006.
GSK offers the next generation of biomedical investigators an intensive doctoral program that trains them to study and attack cancer through the twin lenses of basic research and real-life clinical challenges. The graduates will receive their diplomas as part of Memorial Sloan Kettering Cancer Center’s 43rd annual academic convocation, bringing the total number of GSK’s alumni to 90.
“This is an ambitious and talented group of students with bright futures who deserve to be celebrated,” says GSK Dean Michael Overholtzer. “They have already made important discoveries during their time here, and I’m eager to see their promising careers and scientific accomplishments unfold.”
This year’s graduation will feature a special commencement address from Levi Garraway, Executive Vice President, Head of Global Product Development, and Chief Medical Officer of Roche and Genentech. He is known for pioneering and championing the application of genomics to cancer research, diagnosis, drug development, and treatment, including landmark discoveries in the mechanisms driving tumor growth and resistance to therapy.
“Dr. Garraway’s leadership and extraordinary achievements in cancer research have made a major impact in the field,” says Dr. Overholtzer. “Our graduates and the entire GSK community are looking forward to his insightful remarks.”
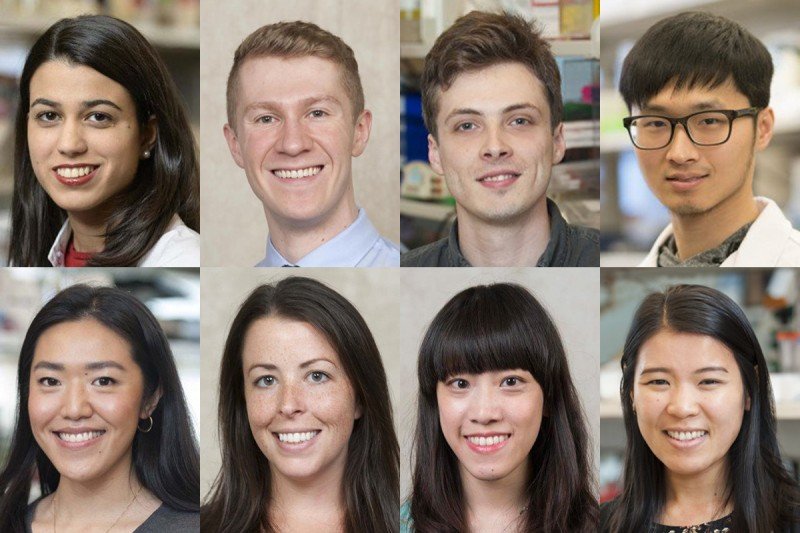
GSK will award doctorates to Corina Amor Vegas, Kevin M. Boehm, Jacob A. Boyer, Hsuan-An Chen, Rui Gao, Emily Kansler, Amy Shyu, and Sarah Tang. Throughout the past year, the students successfully defended their dissertations, the final requirement in earning their doctorates. Learn more about their thesis investigations below.
Corina Amor Vegas

I completed my thesis research in the laboratory of Scott W. Lowe, Chair of the Cancer Biology and Genetics Program at Memorial Sloan Kettering Cancer Center (MSK). His lab studies tumor-suppressor networks and how their disruption influences the development of cancer.
I developed a new technique using immunotherapy to selectively eliminate nondividing cells known as senescent cells. These cells promote inflammation and have been implicated in many age-related diseases, such as lung and liver fibrosis, atherosclerosis, and osteoarthritis.
Chimeric antigen receptor (CAR) T cell therapy is an approach that uses one’s own immune cells to fight cancer. Developed by MSK immunologist Michel Sadelain and colleagues, it has shown remarkable efficacy in treating people with certain types of blood cancers. However, the application of CAR T cell therapy beyond cancer has not been explored.
My research centers on whether CAR T cells can also be harnessed to eliminate senescent cells. Previous attempts to kill senescent cells have focused on using small molecules to treat cancer. However, these compounds lack potency and produce significant side effects.
We developed a unique approach to selectively eliminate senescent cells. To achieve this, we identified uPAR as a protein that is broadly upregulated in senescent cells, and we engineered senolytic CAR T cells to target it. Our results showed for the first time that these senolytic CAR T cells were able to target senescent cells and produce a therapeutic response in mouse models of both liver fibrosis and lung cancer.
This work, which resulted in a patent and a publication in the July 2020 issue of Nature, opens up a completely new strategy to eliminate senescent cells. More research is needed to identify additional CAR targets and CAR construct designs, and to shed light on optimal approaches. Senolytic CAR T cells may have broad therapeutic potential for cancer and the so-called senescence-associated diseases.
I am now an Independent Fellow at the Cold Spring Harbor Laboratory in Cold Spring Harbor, New York.
Kevin M. Boehm

I am a Tri-Institutional MD-PhD Program graduate and completed my dissertation work under the mentorship of Sohrab Shah, Chief of Computational Oncology and Director of MSK MIND (Multimodal Integration of Data). His lab studies cancer evolution and response to treatment through high-density genomics, coupled with advanced computational methods.
As patients undergo cancer diagnosis and treatment, physicians acquire many types of data, ranging from genomic sequencing to computed tomography and digitized histopathology images. These data profile the patient’s tumor and overall health from multiple vantages but remain largely untapped.
My work aims to advance our understanding and management of cancer by designing machine learning methods to integrate big data generated during the delivery of care. Together with colleagues, I recently outlined this paradigm of harnessing multimodal data integration to advance precision oncology in Nature Reviews Cancer.
During my thesis research, I assembled a multimodal data set of radiologic images, pathologic specimens, and tumor sequencing for patients with ovarian cancer. We designed models to extract features from each of these and infer how long patients were likely to survive after standard chemotherapy and surgery. We found that our multimodal model was better than other models at accurately identifying patients at risk of poor outcomes. Upon further validation, such insights may help oncologists and patients in making decisions around therapy, clinical trials, and frequency of follow-up imaging.
For this work, I received a Ruth L. Kirschstein National Research Service Award (NRSA) from the National Institutes of Health and the Grayer Fellowship from MSK. The resulting manuscript is in press.
I was drawn to GSK and the broader MSK community by its focused commitment to understanding cancer and its mission to improve the quality of life for patients afflicted with it. It has been a privilege to learn from thought leaders in computational oncology and clinical practice in such a nurturing training environment. I am delighted to be continuing my clinical and scientific training at MSK via the Transitional Year Internship and Radiation Oncology Residency programs.
Jacob A. Boyer

I conducted my dissertation research in the laboratory of physician-scientist Neal Rosen. He is a medical oncologist whose lab studies signal transduction pathways that cause the dysregulation of growth and inhibition of apoptosis (cell death), which are hallmarks of advanced cancer.
Broadly, my research interests center on understanding protein translation in mammalian biology. My thesis shed light on the mechanism by which the estrogen receptor alpha is translated in breast cancer and identified the protein eIF4A as an essential factor for this process.
Most breast cancers depend on the hormone estrogen for their growth and survival. Estrogen exerts its action through the estrogen receptor (ER), which is found in breast and reproductive tissue, as well as many other organ types.
Drugs that compete with estrogen for receptor binding, or cause receptor degradation, are successful treatments for ER-positive breast cancer. However, patients with advanced disease often relapse, necessitating the development of new therapies.
Translation is the final step in gene expression and is the process by which mRNA is used to synthesize cellular proteins. We found that ER is translated in a noncanonical manner and depends on the translation initiation factor eIF4A for its expression. Drugs that inhibit eIF4A block estrogen receptor activity and expression and impede cell growth, even in models resistant to existing ER-directed targeted therapies.
Our results showed that chemical inhibition of eIF4A was able to significantly reduce tumor growth in cell and mouse models of breast cancer, highlighting eIF4A as a possible therapeutic target. This work informed the decision to include patients with relapsed ER-positive breast cancer in a clinical trial using an eIF4A inhibitor that launched at MSK this year.
In a separate project, we developed the first selective inhibitors of mTOR complex 1 (mTORC1). These drugs have allowed us to begin to explain how different complexes that contain mTOR impact the development of cancer and therapeutic outcomes. This work was key in providing the scientific rationale for a current clinical trial involving the mTORC1 selective inhibitor RMC-5552.
I was drawn to the GSK program because of its streamlined requirements, small class size, and world-class science. The support provided by GSK administration and faculty exceeded my high expectations and has helped me formulate the research interests I will pursue in my next position as a Ludwig Cancer Fellow in the laboratory of Joshua Rabinowitz at Princeton University. I will continue to study protein translation, specifically how it is selectively adapted to various therapies and nutrient-restricted diets.
Hsuan-An Chen

I completed my thesis research in the laboratory of Scott Lowe, Chair of the Cancer Biology and Genetics Program at the Sloan Kettering Institute (SKI), Chair of the Geoffrey Beene Cancer Research Center, and Investigator at the Howard Hughes Medical Institute. His lab uses genetically engineered mouse models to study how genetic alterations in cancer cells contribute to tumor development, alter treatment response, and create molecular vulnerabilities that may be targeted therapeutically.
My thesis work centered on nondividing cells known as senescent cells. Cellular senescence is a stress-response program characterized by a stable cell-cycle arrest and a distinctive secretory program known as the senescence-associated secretory phenotype (SASP). As such, cells undergoing senescence not only exhibit intrinsic phenotypic changes but also remodel their tissue environment to orchestrate a diverse range of physiological and pathological processes.
In the context of cancer, senescence can exert a potent tumor-suppressive effect by causing growth arrest, as well as trigger an immune-mediated killing of damaged, premalignant, or cancer cells — a phenomenon called senescence immune surveillance. When this process is impaired, senescent cells can accumulate within tissues and, paradoxically, promote cancer and other age-related diseases. However, the specific mechanisms underlying the effective immune targeting of senescent cells, and how this process is altered during cancer development, are still not fully understood.
My project aimed to investigate how senescent tumor cells interact with their microenvironment, and to identify mechanisms that promote and mediate anti-tumor immunity. To do so, we used a genetic model of liver cancer with an intact immune system. It allowed us to induce suppression of the tumor suppressor gene p53 and then reverse it to specifically reinstate the senescence program in advanced cancer cells.
We found that senescence induction in advanced liver cancer triggers remodeling of their immune landscape. This leads to potent tumor regressions through activation of adaptive and innate immunity.
Through investigating the underlying mechanisms, one of the striking features we uncovered is that, in addition to the SASP, senescent cells also undergo a substantial rewiring of their surfaceome (surface proteins), predicted to fundamentally alter their environmental sensing capacity. This is exemplified by an enhanced sensitivity to interferon gamma (IFN-γ), a cytokine crucial for anti-tumor immunity, in senescent cells. This appears to be a general feature of senescence across different models and species we have tested. Importantly, senescent cells cooperate with extracellular IFN-γ to show an increased capacity for antigen processing and presentation critical for adaptive anti-tumor immunity.
At a functional level, disruption of IFN-γ sensing by senescent cells blunts their immune-mediated clearance without disabling their characteristic secretory program or immune cell recruitment. This contradicts the previously held thought that excessive immune infiltration is sufficient for immune surveillance. Therefore, our results demonstrate that senescent cells have an enhanced ability to both send and receive environmental signals, and imply that each process is required for their effective immune surveillance.
Overall, our work identifies a novel interplay between tissue remodeling and tissue sensing programs that can be engaged by senescence in advanced cancers to render tumor cells more visible to the adaptive immune system. Our findings provide new insight into how senescent tumor cells interact with the microenvironment and how this interplay can be induced therapeutically to enhance anti-tumor immunity.
I was drawn to GSK because of its integrative environment that bridges basic and translational research, and the leading-edge scientists who work on almost every aspect in cancer biology. I am grateful for the world-class training I have received at GSK, which has prepared me for the next stage of my career as an independent researcher.
After graduation, I will continue my research as a joint postdoctoral fellow in the laboratories of virologist Charles Rice at The Rockefeller University and immunologist Joseph Sun at MSK.
Rui Gao

I completed my thesis research under the mentorship of cancer biologist Andrea Ventura. He studies noncoding RNAs in cancer and development and has a long-standing interest in modeling different types of genomic abnormalities in mice.
During my time in Dr. Ventura’s lab, I spearheaded three different research projects using CRISPR-Cas9 and other gene-editing technologies to study genetic abnormalities found in colorectal cancer, glioblastoma, and chronic lymphocytic leukemia.
The bulk of my thesis centered on modeling and trying to dissect the mechanism of a type of chromosomal alteration that had been discovered many decades ago, but whose role in cancer is just beginning to be characterized. These chromosomal structural changes, called extrachromosomal circular DNAs (ecDNAs), are often found harboring oncogenes in patient samples across different types of cancers.
Using CRISPR-Cas9-based methods, we designed and implemented a new system that would allow us to engineer ecDNA formation in cells as well as in mice to observe the behavior of these ecDNAs over time and in response to selective pressure. The design of our system allows us to induce ecDNA formation almost anywhere in the genome so that we can investigate almost any oncogene of interest.
Using the new germline and somatic mouse models that I helped to generate, Dr. Ventura’s lab is now addressing the question of whether oncogene-carrying ecDNAs have tumorigenic potential.
My graduate training at GSK has taught me to think like a scientist: analytically, critically — and most important — optimistically! This is a skill that applies to so many aspects of life. I also greatly enjoyed my time in New York City, forged unforgettable memories, and developed some of my closest friendships with fellow classmates.
I am currently a technical specialist at Finnegan, Henderson, Farabow, Garrett & Dunner, LLP in Washington, D.C.
Emily Kansler

I conducted my dissertation research in the laboratory of immunologist Ming Li, who studies how the immune response is regulated under different conditions, such as cancer and infection.
My research aimed to uncover how a subset of immune cells called cytotoxic innate lymphocytes are regulated in the tumor microenvironment. I studied this in human kidney cancer, also known as renal cell carcinoma (RCC), as well as in a mouse model of breast cancer.
My research showed that two subtypes of kidney cancer have distinct immune cell profiles. While clear cell (ccRCC) tumors had a conventional CD8 T cell response, chromophobe (chRCC) tumors lacked this response and instead had an abundance of cytotoxic innate lymphocytes. My studies revealed that this cytotoxic innate lymphocyte response was directly controlled by the availability of the cytokine IL-15.
The presence of these innate lymphocytes was associated with better overall patient survival, and the expression of IL-15 correlated with the innate lymphocyte response.
Using the mouse model of breast cancer, I was able to show that the critical source of IL-15 surprisingly came from the tumor cells themselves, not surrounding immune cells or stromal cells. We therefore uncovered a novel immunosurveillance mechanism whereby cytotoxic innate lymphocytes can detect and eliminate cancer cells by directly sensing their expression of IL-15.
These discoveries have been accepted for publication in Nature Immunology and have important implications for future cancer immunotherapy strategies.
I chose GSK because of the amazing immunology research being conducted at MSK and the supportive graduate school community. I was honored to be selected as the 2016–2017 Olayan Fellow.
I am now a Science Policy Analyst in the Office of Public Policy and Government Affairs at the American Association of Immunologists (AAI) in Rockville, Maryland.
Amy Shyu

I completed my thesis research in the laboratory of immunologist Ming Li. His lab studies how immune response is regulated under different conditions, such as cancer and infection.
My work centers on investigating how cellular metabolism influences the function of immune cells and their response in combatting infections and cancers.
T cells are immune cells that provide a critical defense against diseases. Their activity is impacted by the availability of nutrients, as well as by the metabolism of nutrients like glucose and serine. Upon activation, T cells undergo rewired metabolism as part of their normal physiological processes, but the underlying mechanisms remain unresolved. In my dissertation research, I used genetic mouse models to study how glucose and serine influence T cell functions.
We found that LDHA-mediated glycolysis, a key metabolic pathway for glucose, was critical for conventional T cell responses against cancer but dispensable for regulator T cells in chronic viral infections and tumors. Furthermore, by genetically enhancing glucose metabolism through T-cell-specific ablation of the von Hippel-Lindau (VHL) tumor suppressor gene, we were able to improve anti-tumor immunity.
Our research showed with genetic evidence that distinct modes of metabolic dependency exist for different T cell subsets, and that LDHA-mediated glycolysis has a critical role in supporting T cell functions in an environment that challenges the immune system.
Glucose also supports cell growth through its conversion into different amino acids, including serine, relying on a process called de novo synthesis for cell anabolism. Through genetic ablation of PHGDH, a serine de novo synthesis enzyme, we found that de novo synthesis supports optimal T cell activation and differentiation in environments with restricted serine. In addition, we demonstrated that CD8 T cells, which are dependent on serine for their activation, expansion, and effector cell expansion, required proper Akt and mTORC1 signaling to function correctly.
Thus, we reveal that proper metabolic reprogramming of T cells depends not only on fluctuating nutrient availability but also on optimal and sustained T cell signaling. Our findings further substantiate the current understanding of how nutrient metabolism and signaling can cross-talk to support optimal T cell responses.
I was drawn to GSK by its interdisciplinary research across basic and clinical studies, offering unique opportunities to translate lab research findings into potential treatment for people with cancer. It is gratifying to know that my dissertation findings provide a better understanding of how the immune system functions in infections and cancers, which may ultimately lead to improved therapeutic design.
I am currently a consultant at McKinsey & Company, where I provide strategic advice to help advance drug development in pharmaceutical and biotechnology companies. I look forward to using my scientific training to support the goal of eliminating cancer and impacting patient outcomes.
Sarah Tang

I conducted my dissertation research in the laboratory of physician-scientist Ingo Mellinghoff. He is a neuro-oncologist whose lab studies abnormalities in cell signaling pathways driving the development of primary brain tumors and their resistance to treatment.
For my dissertation, I studied an aggressive lymphoma of the brain called primary central nervous system lymphoma (PCNSL). PCNSL is a type of diffuse large B cell lymphoma that grows within the central nervous system. Many people with PCNSL respond well to ibrutinib, a drug that targets Bruton’s tyrosine kinase (BTK). BTK is a protein that is expressed in all B cells and promotes cell survival through the B cell receptor (BCR) signaling pathway. However, ibrutinib is only effective in some B cell malignancies, such as PCNSL.
My thesis aimed to better understand the pathway driving BTK dependence in PCNSL. Using PCNSL cell line- and patient-derived xenograft models developed in our lab, I identified a signature of genes that were regulated by BTK and uncovered pathways downstream of BTK that may be important for the development of PCNSL.
Despite the initial effectiveness of ibrutinib, many patients relapse due to drug resistance. To study the mechanisms of resistance, I established PCNSL cell line models and characterized genetic mutations in genes that were detected only in drug-resistant cells.
I found that certain mutations restored signaling through the BCR pathway, and I evaluated drug combinations to resensitize cells to ibrutinib. Taken together, this research has increased our understanding of the molecular dependency on BTK in PCNSL.
I chose GSK for my PhD studies because of the highly dedicated, intelligent, and inspiring scientists and physicians in the GSK community. The program has a unique focus on translational research that enables students to see the impact of their research on the lives of people with cancer. During my PhD journey, I have learned to have patience, perseverance, and an open mind, and to always let the data guide the way.
I am now a biologist at Neomorph Inc., a growing biotech company in San Diego, focused on developing molecular glue degraders to treat human diseases. My work involves characterizing targets of potent compounds in the early drug discovery stage, determining drug mechanisms of action, and developing assays and cell line models to support ongoing projects in the pipeline.