Bipolar Disorder
How lithium became a treatment for bipolar disorder
Or, the man who ate the first oyster
Posted February 26, 2020
Lithium is the lightest metal—indeed, it can float on water—with a variety of uses in the modern world, including as the negative electrode in lithium batteries, a coolant inside nuclear power plants, an aerospace alloy, and the red color in fireworks. In our context, it is a mainstay in treating manic episodes and maintenance therapy for bipolar disorder and is a beautiful example of how useful drugs have often been discovered for the wrong reasons.
Indeed, it came about while searching for a treatment for "brain gout," a non-existent disease. Because the history of lithium is so deeply interconnected with gout, let’s take a moment to talk about this venerable disease.
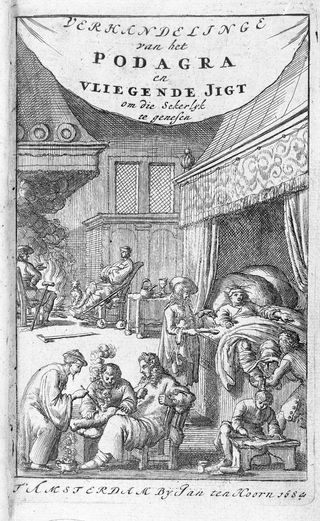
One of the oldest recognized illnesses, going back to the ancient Egyptians, gout was referred to as the "unwalkable disease" by Hippocrates, due to the painful, arthritic nodules of the toe, heels, or ankles. Antoni van Leeuwenhoek (1632–1723), one of the first microscopists, described tiny crystals inside the painful nodules, which later turned out to be urate, a result of the chemical breakdown of purines, one of the constituents of DNA. Purines are dietary substances found in beer, meats, and seafood, so historically gout became known as an affliction of the well-to-do.
In 1859, Alfred Baring Garrod (1819-1909), who later went on to become Queen Victoria’s physician, reported that persons with gout had very high levels of uric acid in the blood. This finding appeared to be unique to gout, as it was not present in similarly painful joint diseases, such as acute rheumatism. Interestingly, he reported using lithium to treat gout and speculated that it might be helpful in mental disorders.
To put this in perspective, during the 19th and early 20th century, it was speculated that besides arthritic gout, there existed a condition known as "uric acid diathesis," an inflammatory disorder which could produce "brain gout." Indeed, some physicians, such as Charles Bland Radcliffe from Queen Square, London, had been using potassium bromide for seizures, which he considered to be a "semi-gouty" condition.
Lithium salts had been used for some time to treat, and hopefully dissolve, kidney and gall stones, and Garrod’s suggestion for using lithium for mental disorders was a natural consequence. In 1871, William A. Hammond (1828-1900), a former Surgeon General in the Union army, described successfully treating manic patients at Bellevue Hospital with lithium bromide, though he commented that "It is difficult to determine in retrospect whether it was the lithium or the bromide that was the critical agent."1
In some ways, Hammond was like "the man who ate the first oyster," a doctor who found something he believes is good but does not have the backing of a body of scientific literature. (The phrase is attributed to John Jennings of the U.S. Food and Drug Administration.) Even though Carl Lange (1834-1900), a Danish physician, gave lithium carbonate to 2,000 patients for preventing recurrent depression and described positive results, lithium was largely forgotten by the medical community.
It was not until 1949 that lithium was rediscovered by Australian psychiatrist John Cade (1912-1980) and eventually moved into mainstream psychiatry. Cade was the son of a general practitioner who served in World War I and returned with what was then called "war-weariness." Rather than continuing his practice, he became the director of a series of mental hospitals.
It was often customary for the director to live on the grounds of such facilities, and it seems likely that at a young age, John was exposed to seeing the consequences of chronic mental illness. He followed in his father’s footsteps and went to medical school, received psychiatric training, and then, a few years later at the outbreak of World War II, entered the Australian Army Medical Corps in a surgical capacity.
He was sent to Singapore in 1941, and after its capture by the Japanese, he became a prisoner of war until 1945. After recuperating, he resumed psychiatric work at Bundoora Repatriation Mental Hospital, a veterans’ facility near Melbourne. It was there, in his makeshift laboratory in an empty kitchen, that Cade rediscovered the use of lithium in mental disorders.
Cade was interested in the possibility that manic depressive illness (now known as bipolar disorder) might be due to a toxic substance, which in excess might cause mania and if depleted might result in depression. In view of Garrod’s studies, he wondered if this substance might be related to uric acid. In an effort to test his theory, he injected the urine from manic patients and mentally healthy persons into guinea pigs and found that the former was much more likely to be harmful.
Among the various substances found in urine, including creatinine, urea, and uric acid, he found that urea was the most toxic. The puzzle was that the amount of urea was similar in manic and healthy persons, so he focused his interest on the notion that some other substance in the urine of manic patients increased the harm done by urea, and he guessed that this might be uric acid. He decided to see if uric acid made the animals sicker than if they were given urea alone.
Initially, he had difficulty dissolving the uric acid in sufficient concentrations, so he came upon the idea of using the much more soluble lithium urate. To his surprise, lithium urate had the opposite effect from his prediction, greatly reducing the harmful effects of urea. He then chose to separate out the effects of lithium itself and experimented with lithium carbonate, finding that it made guinea pigs very quiet. Thus began the long process of developing a medicine for humans.
Although lithium had been given to humans for many years, Cade administered it to himself to determine safe doses. He then gave it to 10 manic patients and reported in a 1949 paper in the Medical Journal of Australia that their symptoms were much improved, and five of these persons with longstanding illness were able to be discharged.
In a manner that might have felt familiar to his lithium predecessor William A. Hammond, there was initially little interest outside Australia in this potentially important discovery. Cade experimented, giving other elements such as cerium and rubidium without success. He was also discouraged by the death of one of his patients, which was attributed by the coroner to lithium toxicity, and he went off to pursue other areas.
In 1954, however, a Danish team led by psychiatrist Mogens Schou published the very positive results of a carefully done study and greatly increased the interest in lithium. In those years, its use was limited, because the therapeutic dose was very close to the toxic dose, and there was no reliable way to determine the correct amount to give. This changed in 1958 with the development of an effective test for blood levels, making it much safer, and the results more consistent. It was gradually accepted over the course of the 1960s and 1970s and remains one of the mainstays of treatment of mania and prevention of recurring episodes of bipolar disorder, although a number of other "mood stabilizer" drugs are now available.
Adapted from The Curious History of Medicines in Psychiatry by Wallace B. Mendelson, M.D.
References
1. W.A. Hammond: A treatise on diseases of the nervous system. D. Appleton, 1871, p. 516.




