Abstract
The objective of this study was to evaluate the bidirectional association between asthma and migraines using control subjects matched by demographic factors. The Korean Health Insurance Review and Assessment Service - National Sample Cohort from 2002 to 2013 was used. In study I, 113,059 asthma participants were matched with 113,059 control I participants. In study II, 36,044 migraine participants were matched with 114,176 control II participants. The hazard ratios (HRs) of migraines in the asthma patients (study I) and asthma in the migraine patients (study II) were analyzed using stratified Cox proportional hazard models after adjusting for depression and the Charlson comorbidity index. In study I, 5.3% (6,017/ 113,059) of the asthma group and 3.4% (3,806/ 113,059) of the control I group had migraines (P < 0.001). The asthma group demonstrated an adjusted HR of 1.47 for migraine (95% confidence interval (CI) = 1.41–1.53, P < 0.001). In study II, 15.4% (5,548/36,044) of the migraine group and 10.6% (15,271/144,176) of the control group had asthma (P < 0.001). The migraine group showed an adjusted HR of 1.37 for asthma (95% CI = 1.33–1.41, P value < 0.001). Asthma and migraines are reciprocally associated.
Similar content being viewed by others
Introduction
Asthma is a chronic airway disease associated with clusters of respiratory symptoms, including wheezing and dyspnea. Asthma is a common disease with different prevalences according to ethnicity that range from approximately 7% to 18.0%1. The incidence of asthma in the adult population (>20 years old) was estimated to be approximately 3.63–6.07 per 1,000 people in Korea2. Because the diagnosis of asthma is based on the functional deterioration of the lower airway, the underlying pathophysiologic causes of asthma have been reported to vary among asthmatic patients3. According to the pathophysiologic mechanisms, asthma is classified as two major endotypes of T-helper type 2 cell (TH2)-high and TH2-low diseases4. Thus, in addition to TH2-high related diseases, such as allergic rhinitis, other immune-related diseases could complicate asthma. In addition, both genetic factors and environmental triggering factors have been suggested to be related to asthma5,6.
Migraine disorder is another chronic disease characterized by multiple symptoms of headache and/or aura. As many as approximately 1.04 billion people suffer from migraines worldwide (95% uncertainty interval = 1.00–1.09)7. In Korea, approximately 6.0% of the adult population (19–69 years) suffers from migraines8. Migraines are characterized by recurrent episodic symptom sequences of a premonitory phase, an aura phase, a headache phase, and a postdrome phase9. The environmental triggering factors can hyper-activate the hypothalamic-pituitary-adrenocortical axis and autonomic nervous system in migraine susceptible subjects10. These hormonal and nervous changes induce vasodilation, the release of vascular factors, including growth factors, cytokines, nitric oxide, norepinephrine and calcitonin gene-related peptide, and interaction with endothelial cells, resulting in migraine symptoms11. The pathophysiology of the hormonal imbalance and environmental triggering factors are common in both migraines and asthma12,13,14. Due the these shared pathophysiology and recurrent symptoms, asthma was hypothesized as a acephalgic migraine or pulmonary migraine15,16. In addition, several epidemiologic studies reported the high rate of asthma in migraine patients and vice versa17,18.
Clinically, a considerable portion of asthma patients have comorbid headaches19,20, and it was questionable which disease was the first event. We postulated that asthma and migraine have reciprocal relationships with each other. To prove this hypothesis, we designed two independent studies. In study I, asthma patients were evaluated for the risk of subsequent migraine and compared to a nonasthmatic control group. In contrast, study II was designed to investigate the subsequent occurrence of asthma in migraine patients compared to a nonmigraine control group. No previous study has concurrently evaluated the bidirectional association between asthma and migraine. In addition, the control group subjects were matched with the study group subjects by age, sex, income, and region of residence. We adjusted for depression and the Charlson comorbidity index (CCI) to exclude potential confounding effects.
Results
Study I
The time duration from the index date to a migraine was 43.8 months (SD = 33.5) in the asthma group and 43.0 months (SD = 34.5) in the control I group. The rate of migraine was higher in the asthma group (5.3% [6,017/113,059]) than in the control I group (3.4% [3,806/113,059], P < 0.001, Table 1). The rate of migraines with aura and migraines without aura in the asthma group were also higher than those in the control I group (S1 Table). The general characteristics (age, sex, income, and region of residence) of the participants were exactly the same due to matching (P = 1.000).
The adjusted HRs of migraines in the asthma group were 1.47 (95% CI = 1.41–1.53, P < 0.001, Table 2 and Fig. 1(a)). The adjusted HRs of migraines with aura and migraines without aura in the asthma group were 1.54 (95% CI = 1.33–1.78, P < 0.001) and 1.46 (1.40–1.53, P < 0.001), respectively. The adjusted HRs of migraine in asthma group were 1.96 (95% CI = 1.70–2.26) and 1.96 (95% CI = 1.63–2.37) after considering interactions with age and sex, respectively (S2 Table).
In all subgroup analyses, higher adjusted HRs for migraine were observed in the asthma group (all P value < 0.001, Table 3). The adjusted HR was 2.05 (95% CI = 1.67–2.54) in <40-year-old men, 1.64 (95% CI = 1.49–1.79) in <40-year-old women, 1.73 (95% CI = 1.49–2.01) in 40–59-year-old men, 1.33 (95% CI = 1.24–1.43) in 40–59-year-old women, 1.45 (95% CI = 1.27–1.66) in ≥60-year-old men, and 1.39 (95% CI = 1.28–1.50) in ≥60-year-old women. These higher HRs of migraine in the asthma groups were also consistent during the follow-up periods (S3 Table).
Study II
The time duration from the index date to asthma was 42.4 months (SD = 33.2) in the migraine group and 43.0 months (SD = 33.8) in the control II group. The rate of asthma was higher in the migraine group (15.4% [5,548/36,044]) than in the control II group (10.6% [15,271/144,176], P < 0.001, Table 1). The rate of asthma in the migraines with aura group and migraines without aura group was also higher than that in the control II group (S4 Table). The general characteristics (age, sex, income, and region of residence) of the participants were exactly the same due to matching (P = 1.000).
The adjusted HR of asthma in the migraine group was 1.37 (95% CI = 1.33–1.41, P value < 0.001, Table 4 and Fig. 1(b)). The adjusted HRs of asthma in the migraines with aura and migraines without aura groups were 1.39 (95% CI = 1.25–1.55, P < 0.001) and 1.37 (1.32–1.41, P < 0.001), respectively. The adjusted HRs of asthma in migraine group were 1.68 (95% CI = 1.49–1.88) and 1.80 (95% CI = 1.56–2.08) after considering interactions with age and sex, respectively (S2 Table). In all subgroup analyses, higher adjusted HRs for asthma were observed in the migraine group (all P value < 0.001, Table 5). The adjusted HR was 1.65 (95% CI = 1.40–1.95) in <40-year-old men, 1.42 (95% CI = 1.32–1.52) in < 40-year-old women, 1.57 (95% CI = 1.41–1.75) in 40–59-year-old men, 1.31 (95% CI = 1.25–1.38) in 40–59-year-old women, 1.45 (95% CI = 1.30–1.62) in ≥60-year-old men, and 1.27 (95% CI = 1.19–1.35) in ≥60-year-old women. These higher HRs for migraine in the asthma groups were also consistent during the follow-up periods (S5 Table).
Discussion
The present study demonstrated a bidirectional relationship between asthma and migraine in an adult population. The migraine patients demonstrated a 1.47 times higher hazard ratio of asthma than the control participants without migraines. However, the asthma patients showed a 1.37 times higher risk of migraines than the non-asthmatic control participants. All age and sex subgroups showed consistent results for both the risk of asthma in migraine patients and the risk of migraine in asthmatic patients. This study is the first to investigate the bidirectional relationship between asthma and migraines using matched control subjects and adjustment for the CCI. In addition, the migraine groups were classified based on the presence of aura.
In line with the present results, several previous studies have reported an association between asthma and migraine. A recent meta-analysis reported that asthmatic patients had 1.62 times higher odds of migraines than control subjects (95% confidence interval [95% CI] = 1.43–1.82)21. However, the migraine patients showed a 1.56 times higher risk of asthma than the control subjects (95% CI = 1.51–1.60, P < 0.00001)21. Using national health insurance data, a Taiwanese group demonstrated a 1.37-fold increased risk of asthma in migraine patients (95% CI = 1.21–1.56)17. Another study reported a 1.45-fold higher risk of migraine in asthma patients (95% CI = 1.33–1.59)18. However, their control groups were not matched with their study groups for socioeconomic factors and past medical histories. The study groups demonstrated higher rates of low economic status and comorbidities including rhinitis, sinusitis, atopic dermatitis, and chronic obstructive pulmonary disease. Although we adjusted for these covariates, the confounding effects of these covariates could not be excluded. Moreover, the importance of a past medical history of cardiovascular disease was not considered in these studies. The present study improved these previous findings by using control subjects who were matched for their past medical histories and demographic factors. Although future studies are warranted to delineate the biological pathophysiological mechanisms, a few plausible causes can be postulated from a number of prior studies.
The common pathophysiologic factors of inflammation and immune dysfunction between asthma and migraine could contribute to the bidirectional association between asthma and migraine. For instance, atopy, parasympathetic hyperactivity, and elevated neuropeptide secretion contribute to both asthma and migraines22. Allergic responses triggered by allergens, such as specific grass, pollen, and even hypertonic saline, evoke airway hypersensitivity responses mediated by mast cells in asthmatic patients23. In migraines, mast cells in the dura, which are activated by allergens, are presumed to excite meningeal nociceptors and initiate the activation of nearby trigeminal afferents24. In addition, parasympathetic hyperactivity is another shared feature of both asthma and migraine. An increased cholinergic tone in non-respiratory systems, which manifests as anxiety, reflux, heartburn, and abdominal pain, precedes asthma symptoms and has been suggested to trigger bronchospasm in asthma25. Parasympathetic afferents have been suggested to release acetylcholine, vasoactive intestinal polypeptide, and pituitary adenylate cyclase-activating polypeptide, which directly activate trigeminal nerves or provoke the degranulation of mast cells at meningeal levels in migraine26.
The shared triggering and environmental factors between asthma and migraine could induce a subsequent disease. Environmental factors including air pollutants impact both asthma and migraine. Air pollutants, including particulate matter, nitrogen dioxide, ozone, and carbon monoxide, are associated with the occurrence or aggravation of asthma, most likely due to oxidative stress affecting the airways27. Similarly, particulate matter, nitrogen dioxide, ozone, and carbon monoxide concentrations are related to the rate of emergency department visits for migraines (odds ratio = 1.053, 95% CI = 1.022–1.085 for nitrogen dioxide)28. Moreover, several lifestyle factors including obesity and smoking have been speculated to induce both asthma and migraine. In obese patients, due to the increased proportion of adipose tissue, systemic inflammation, metabolic changes, such as insulin resistance, and immune disturbances accompanied by microbiome changes occur and influence the occurrence of asthma29. For migraine, a recent meta-analysis reported that obesity increased the risk of migraine (odds ratio = 1.27, 95% CI = 1.16–1.37, P < 0.001)30.
Emotional stress, which is related to asthma and migraines, can promote the occurrence of other diseases. Stress or psychological distress, such as depression, due to asthma could increase an individual’s susceptibility to migraines and vice versa. Asthma was associated with a 1.35 times greater risk of depression in a previous study (95% CI = 1.31–1.40)31. Depression and stressful events are important modifiable risk factors for migraines32.
According to age and sex, all subgroups demonstrated a reciprocal association between asthma and migraines in the present study. Although the prevalence of migraines is higher in women than in men, the impact of asthma on migraines and the impact of migraines on asthma might be consistent regardless of sex33. In addition, both migraines with aura and migraines without aura were associated with the increased risk of asthma and vice versa in this study. Migraines with aura are suggested to be more associated with a family history of migraines and elevated risk of myocardial infarction, atrial fibrillation and stroke than migraines without aura34,35,36. Thus, migraines with aura might be more associated with cardiovascular and cerebrovascular compromise and related inflammatory responses. Therefore, the current study demonstrated higher HRs for migraines with aura in asthma patients (study I) and for asthma in migraines with aura patients (study II) compared to those with migraines without aura. In the present study, the risk of migraine associated with asthma (study I) was higher in both men and women (Table 3). There might have sex difference for the risk of migraine in asthma patients due to the higher rate of related comorbidities of migraine, thereby more other contributing factors for migraine, besides of asthma, in women than men. It was reported that women had more frequent headache and migraine-related comorbidities than men37,38. On the other hands, the risk of asthma related with migraine (study II) was also higher in both men and women (Table 5). The risk of asthma in migraine patients could be different according to sex due to the effect of sex hormone on the development of asthma. Estrogen was suggested to increase which testosterone was suggested to decrease Th2-mediated airway inflammation in asthma39. Both the risk of migraine associated with asthma and the risk of asthma related with migraine were decreased with aging in this study. The increase of comorbidities in elderly could attenuate the impact of asthma or migraine on the risk of migraine or asthma in this aged population. In the present study, the reciprocal associations between asthma and migraine were consistent after considering the interactions with age and sex (S2 Table).
The present study used a large study population, which provided a large number of control subjects. Due to this large population, random selection could be performed, including matching the control group participants for age, sex, income, and region of residence. Matching for socioeconomic status was crucial in this study based on health insurance codes because medical accessibility might be considerably determined by socioeconomic status. Because all Koreans are legally registered and reimbursed their medical costs by the Korean NHIS, no missing participants were anticipated. For the classifications of asthma and migraine, both diseases were diagnosed by physicians twice or more, and medication prescriptions were checked for asthma. Moreover, migraines were classified according to the presence of aura. Approximately 8% of migraine patients had aura in this study. This figure was lower than that reported in a previous study involving a Han Chinese population33. These objective and multiple inclusion criteria enhanced the fidelity of the present study. However, largely due to the limits of information included in the NHIS database, a few limitations of this study should be considered when interpreting the present results. Because the current study based on the health claim data, there is a limitation on the sensitivity and specificity of the definition of asthma. Approximately 20–70% of asthma patients were estimated to be undiagnosed and untreated, while about 30–35% of physician-diagnosed asthma patients were suggested not to have current asthma in a review study40, Subclinical or mild asthma or migraine patients might have been missed due to the lack of clinical visits. The severity or subtypes of asthma and migraine and each patient’s compliance to treatment could not be assessed. For instance, “allergic” asthma and “non-allergic” asthma could not be differentiated in this study. Detailed medication histories could not be considered for both diseases. The chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) in migraine patients could influence the occurrence of NSAID-induced asthma. In addition, lifestyle factors including obesity, smoking, and alcohol consumption were not available.
In conclusion, migraines increase the risk of asthma. Asthma was also associated with an elevated risk of migraine.
Materials and Methods
Study population and data collection
This study was ratified by the Ethics Committee of Hallym University (2017-I102). All analyses were conducted according to the guidelines and regulations of the ethics committee of Hallym University. The written informed consent was excused by the institutional review board.
The Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC) was used as described in the prior studied41,42.
Participant selection
The participants who were diagnosed with asthma (ICD-10: J45) or status asthmaticus (J46) from 2002 through 2013 were enrolled in this study, among the 1,125,691 cases with 114,369,638 medical claim codes. Among them, the asthma group was defined by a physician-diagnosis more than 2 times and the asthma-related medication histories, including inhaled corticosteroids (ICSs), ICSs combined with long-acting β2-agonists (LABAs), oral leukotriene antagonists (LTRAs), short-acting β2-agonists (SABAs), systemic LABAs, xanthine derivatives, and systemic corticosteroids (n = 230,764), similarly to a previous study43.
Migraine was defined based on the ICD-10 code (G43). Migraines were classified as migraines with aura and migraines without aura (ICD-10: G431). The participants who were treated for migraine ≥2 times (n = 45,587) from 2002 through 2013 were included. Both asthma and migraine were selected if participants were diagnosed with these conditions ≥2 times. The initial diagnosis was clinically determined by a diagnostic work-up including laboratory and imaging studies, and the confirmative diagnosis was performed at the second clinical visit.
Study I
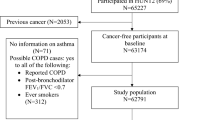
Asthmatic participants were matched 1:1 with the participants (control I) without asthma. The control participants were randomly extracted from the original population as previous studies (n = 894,927)41,42. The participants were matched by age, group, sex, income group, region of residence, and past medical history (hypertension, diabetes, and dyslipidemia). In the asthma group, 5,692 participants were excluded. The asthma participants who lacked enough matched controls were excluded (n = 21,587). The <20 years of participants were excluded (n = 90,426). The mean follow up time was 80.7 months (Standard deviation [SD] = 41.1) for asthma group and 80.5 months (SD = 41.4) for control I group. As results, the 113,059 asthmatic participants and 113,059 control I subjects (nonasthmatic subjects) were included (Fig. 2(a)). The risks of migraine in the asthma and control I groups were analyzed.
Schematic illustration of the participant selection process that was used in the present study. (a) Of a total of 1,125,691 participants, 113,059 asthma patients were matched with 113,059 control I participants by age group, sex, income group, region of residence, and past medical histories. (b) Of a total of 1,125,691 participants, 36,044 migraine patients were matched with 144,176 control II participants by age group, sex, income group, and region of residence.
Study II
Migraine patients were matched 1:4 with the control II group without migraine. The control participants were randomly extracted from the original population as previous studies (n = 894,927)41,42. The participants were matched for age, group, sex, income group, region of residence, and past medical history (hypertension, diabetes, and dyslipidemia). In the migraine group, 6,889 participants were excluded. The migraine participants who lacked enough matched controls were excluded (n = 55). The <20 years of participants were excluded (n = 2,599). The mean follow up time was 82.5 months (SD = 41.5) for migraine group and 81.9 months (SD = 41.7) for control II group. As results, the 36,044 migraine participants and 144,176 control II participants (nonmigraine participants) were included (Fig. 2(b)). The risks of asthma in migraine and control II groups were analyzed.
Variables
The participants’ age group, income group, and region of residence was categorized as described in our prior studies41,42.
We adjusted for depression in the analysis due to its reciprocal association with asthma as revealed in our previous study44. Depression was classified as previously detailed44. CCI was counted, except for pulmonary disease, which includes asthma45.
Statistical analyses
The general characteristics between the asthma and control groups (study I) and between the migraine and control groups (study II) were compared using the Chi-square test.
In study I, to analyze the hazard ratio (HR) of asthma for migraine, a stratified Cox proportional hazard model was used. In study II, to analyze the HR of migraine for asthma, another stratified Cox proportional hazard model was applied. In these analyses, crude and adjusted (depression and CCI) models were applied. These analyses were stratified for age, sex, income, and region of residence, and the 95% CIs were calculated. A Kaplan-Meier analysis and Log-rank test were conducted.
The participants were divided according age and sex (<40 years, 40–59 years, and 60+ years; male and female) to confirm these associations in different age and sex groups.
Two-tailed analyses were performed. The statistical significance was defined as P < 0.05. The SPSS v. 21.0 (IBM, Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) were used.
References
Akinbami, L. J., Rossen, L. M., Fakhouri, T. H. I., Simon, A. E. & Kit, B. K. Contribution of weight status to asthma prevalence racial disparities, 2–19 year olds, 1988–2014. Annals of epidemiology 27, 472–478 e473, https://doi.org/10.1016/j.annepidem.2017.07.004 (2017).
Shin, J. Y. et al. Changing patterns of adult asthma incidence: results from the National Health Insurance Service-National Sample Cohort (NHIS-NSC) database in Korea. Sci Rep 8, 15052, https://doi.org/10.1038/s41598-018-33316-y (2018).
Skloot, G. S. Asthma phenotypes and endotypes: a personalized approach to treatment. Current opinion in pulmonary medicine 22, 3–9, https://doi.org/10.1097/MCP.0000000000000225 (2016).
Stokes, J. R. & Casale, T. B. Characterization of asthma endotypes: implications for therapy. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology 117, 121–125, https://doi.org/10.1016/j.anai.2016.05.016 (2016).
Park, H. W. et al. Assessment of genetic factor and depression interactions for asthma symptom severity in cohorts of childhood and elderly asthmatics. Exp Mol Med 50, 77, https://doi.org/10.1038/s12276-018-0110-5 (2018).
Zheng, Y. et al. A meta-analysis of the association between CTLA-4 genetic polymorphism and susceptibility of asthma. Medicine 97, e11380, https://doi.org/10.1097/MD.0000000000011380 (2018).
Collaborators, G. B. D. H. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17, 954–976, https://doi.org/10.1016/S1474-4422(18)30322-3 (2018).
Kim, B. K., Chung, Y. K., Kim, J. M., Lee, K. S. & Chu, M. K. Prevalence, clinical characteristics and disability of migraine and probable migraine: a nationwide population-based survey in Korea. Cephalalgia 33, 1106–1116, https://doi.org/10.1177/0333102413484990 (2013).
Charles, A. The evolution of a migraine attack - a review of recent evidence. Headache 53, 413–419, https://doi.org/10.1111/head.12026 (2013).
Sauro, K. M. & Becker, W. J. The stress and migraine interaction. Headache 49, 1378–1386, https://doi.org/10.1111/j.1526-4610.2009.01486.x (2009).
Jacobs, B. & Dussor, G. Neurovascular contributions to migraine: Moving beyond vasodilation. Neuroscience 338, 130–144, https://doi.org/10.1016/j.neuroscience.2016.06.012 (2016).
Gupta, V. K. Recurrent syncope, hypotension, asthma, and migraine with aura: role of metoclopramide. Headache 45, 1413–1416, https://doi.org/10.1111/j.1526-4610.2005.00276_2.x (2005).
Ozge, A., Uluduz, D. & Bolay, H. Co-occurrence of migraine and atopy in children and adolescents: myth or a casual relationship? Current opinion in neurology 30, 287–291, https://doi.org/10.1097/WCO.0000000000000439 (2017).
Steinemann, A. National Prevalence and Effects of Multiple Chemical Sensitivities. Journal of occupational and environmental medicine 60, e152–e156, https://doi.org/10.1097/JOM.0000000000001272 (2018).
Hayashi, T. Asthma and migraine–is asthma a part of acephalgic migraine? A hypothesis. Annals of allergy 60, 374 (1988).
Tucker, G. F. Jr. Pulmonary migraine. The Annals of otology, rhinology, and laryngology 86, 671–676, https://doi.org/10.1177/000348947708600524 (1977).
Peng, Y. H. et al. Association of migraine with asthma risk: A retrospective population-based cohort study. The clinical respiratory journal 12, 1030–1037, https://doi.org/10.1111/crj.12623 (2018).
Peng, Y. H. et al. Risk of Migraine in Patients With Asthma: A Nationwide Cohort Study. Medicine 95, e2911, https://doi.org/10.1097/MD.0000000000002911 (2016).
Turan, M. O., Susuz, C. C. & Turan, P. A. Presence of Headache and Migraine in Asthma Patients. Turkish thoracic journal 18, 47–51, https://doi.org/10.5152/TurkThoracJ.2017.16008 (2017).
Gungen, A. C. & Gungen, B. Assessment of Headache in Asthma Patients. Pakistan journal of medical sciences 33, 156–161, https://doi.org/10.12669/pjms.331.11720 (2017).
Sayyah, M. et al. Which came first, the risk of migraine or the risk of asthma? A systematic review. Neurol Neurochir Pol 52, 562–569, https://doi.org/10.1016/j.pjnns.2018.07.004 (2018).
Martin, V. T. et al. Asthma is a risk factor for new onset chronic migraine: Results from the American migraine prevalence and prevention study. Headache 56, 118–131, https://doi.org/10.1111/head.12731 (2016).
Tomljenovic, D. et al. Females have stronger neurogenic response than males after non-specific nasal challenge in patients with seasonal allergic rhinitis. Medical hypotheses 116, 114–118, https://doi.org/10.1016/j.mehy.2018.04.021 (2018).
Levy, D., Burstein, R., Kainz, V., Jakubowski, M. & Strassman, A. M. Mast cell degranulation activates a pain pathway underlying migraine headache. Pain 130, 166–176, https://doi.org/10.1016/j.pain.2007.03.012 (2007).
Liccardi, G. et al. Can bronchial asthma with an highly prevalent airway (and systemic) vagal tone be considered an independent asthma phenotype? Possible role of anticholinergics. Respiratory medicine 117, 150–153, https://doi.org/10.1016/j.rmed.2016.05.026 (2016).
Mikhailov, N., Mamontov, O. V., Kamshilin, A. A. & Giniatullin, R. Parasympathetic Cholinergic and Neuropeptide Mechanisms of Migraine. Anesthesiology and pain medicine 7, e42210, https://doi.org/10.5812/aapm.42210 (2017).
Guarnieri, M. & Balmes, J. R. Outdoor air pollution and asthma. Lancet 383, 1581–1592, https://doi.org/10.1016/S0140-6736(14)60617-6 (2014).
Lee, H. et al. Ambient air pollution exposure and risk of migraine: Synergistic effect with high temperature. Environment international 121, 383–391, https://doi.org/10.1016/j.envint.2018.09.022 (2018).
Gomez-Llorente, M. A., Romero, R., Chueca, N., Martinez-Canavate, A. & Gomez-Llorente, C. Obesity and Asthma: A Missing Link. International journal of molecular sciences 18, https://doi.org/10.3390/ijms18071490 (2017).
Gelaye, B. et al. Body composition status and the risk of migraine: A meta-analysis. Neurology 88, 1795–1804, https://doi.org/10.1212/WNL.0000000000003919 (2017).
Choi, H. G. et al. Association between asthma and depression: A National Cohort Study. The journal of allergy and clinical immunology. In practice, https://doi.org/10.1016/j.jaip.2018.10.046 (2018).
May, A. & Schulte, L. H. Chronic migraine: risk factors, mechanisms and treatment. Nature reviews. Neurology 12, 455–464, https://doi.org/10.1038/nrneurol.2016.93 (2016).
Lin, Q. F. et al. Prevalence of migraine in Han Chinese of Fujian province: An epidemiological study. Medicine 97, e13500, https://doi.org/10.1097/MD.0000000000013500 (2018).
Sen, S. et al. Migraine with visual aura is a risk factor for incident atrial fibrillation: A cohort study. Neurology 91, e2202–e2210, https://doi.org/10.1212/WNL.0000000000006650 (2018).
Androulakis, X. M. et al. Migraine Age of Onset and Association With Ischemic Stroke in Late Life: 20 Years Follow-Up in ARIC. Headache, https://doi.org/10.1111/head.13468 (2019).
Adelborg, K. et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. Bmj 360, k96, https://doi.org/10.1136/bmj.k96 (2018).
Lipton, R. B. et al. Migraine in America Symptoms and Treatment (MAST) Study: Baseline Study Methods, Treatment Patterns, and Gender Differences. Headache 58, 1408–1426, https://doi.org/10.1111/head.13407 (2018).
Song, T. J. et al. Sex Differences in Prevalence, Symptoms, Impact, and Psychiatric Comorbidities in Migraine and Probable Migraine: A Population-Based Study. Headache 59, 215–223, https://doi.org/10.1111/head.13470 (2019).
Fuseini, H. & Newcomb, D. C. Mechanisms Driving Gender Differences in Asthma. Current allergy and asthma reports 17, 19, https://doi.org/10.1007/s11882-017-0686-1 (2017).
Aaron, S. D., Boulet, L. P., Reddel, H. K. & Gershon, A. S. Underdiagnosis and Overdiagnosis of Asthma. American journal of respiratory and critical care medicine 198, 1012–1020, https://doi.org/10.1164/rccm.201804-0682CI (2018).
Kim, S. Y. et al. Bidirectional association between gastroesophageal reflux disease and depression: Two different nested case-control studies using a national sample cohort. Scientific reports 8, 11748, https://doi.org/10.1038/s41598-018-29629-7 (2018).
Kim, S. Y., Lim, J. S., Kong, I. G. & Choi, H. G. Hearing impairment and the risk of neurodegenerative dementia: A longitudinal follow-up study using a national sample cohort. Scientific reports 8, 15266, https://doi.org/10.1038/s41598-018-33325-x (2018).
Kim, S. et al. Healthcare use and prescription patterns associated with adult asthma in Korea: analysis of the NHI claims database. Allergy 68, 1435–1442, https://doi.org/10.1111/all.12256 (2013).
Choi, H. G. et al. Association Between Asthma and Depression: A National Cohort Study. The journal of allergy and clinical immunology. In practice 7, 1239–1245 e1231, https://doi.org/10.1016/j.jaip.2018.10.046 (2019).
Quan, H. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. American journal of epidemiology 173, 676–682, https://doi.org/10.1093/aje/kwq433 (2011).
Acknowledgements
This work was supported in part by a research grant (NRF-2018-R1D1A1A02085328 and 2017R1C1B1007696) from the National Research Foundation (NRF) of Korea. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization, H.G.C.; methodology, H.G.C., C.M. and D.J.O.; formal analysis, C.M. and D.J.O.; writing—original draft preparation, H.G.C. and S.Y.K.; writing—review and editing, H.G.C., J.S.L. and S.Y.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S.Y., Min, C., Oh, D.J. et al. Bidirectional association between asthma and migraines in adults: Two longitudinal follow-up studies. Sci Rep 9, 18343 (2019). https://doi.org/10.1038/s41598-019-54972-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-54972-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.