There is always a race against the clock to tackle influenza outbreaks, both the seasonal global waves of disease and the occasional pandemic. “Somewhere in the world right now, influenza is causing a horrible problem and killing lots of people,” says Rick Bright, director of the US Biomedical Advanced Research and Development Authority (BARDA).
Better responses to flu outbreaks demand not just more-effective flu vaccines, but quicker ways to produce them. This is because catching the outbreak in time is crucial and the volumes of vaccines required are huge. In the United States, for instance, manufacturers are expected to make more than 160 million doses for the coming flu season. And to stem a pandemic, BARDA might need 600 million doses.
Most flu vaccines are made in chicken eggs in a process little changed for decades. “Just over 90% of the vaccines supplied for influenza come from eggs,” says Martin Friede, coordinator of the Initiative for Vaccine Research at the World Health Organization (WHO) in Geneva. Production takes six months—an eternity when there is a potentially deadly virus constantly mutating around the world.
But alternative manufacturing methods are emerging. Cell-based flu vaccines have been approved that can be made more quickly, and in some seasons these are more effective than eggbased vaccines because they can match more closely with target flu strains. More-radical production techniques are also approaching approval, such as growing vaccines in plants or delivering them using messenger RNA. But the road to commercial manufacturing is long and expensive, as each platform must show that the vaccines it produces can outperform conventional drugs and are cheaper to produce than egg-based vaccines.
NOT-SO-RAPID RESPONSE
Academic and industry researchers around the world are searching for a universal flu vaccine—one that works for several years at least, and ideally one that permanently guards against certain types of flu or protects particular populations. The Center for Infectious Disease Research and Policy at the University of Minnesota in Minneapolis is tracking about 80 flu-vaccine research efforts. “We are seeing the emergence of a renaissance around influenza vaccines,” says its director, Michael Osterholm. “And it’s not just cosmetic improvement in the current vaccines.”
Many research efforts are targeting manufacturing technologies that do not require eggs and so avoid the limitations of this decadesold technique. The biggest problem is time. It takes weeks to optimize viruses to grow well in eggs while ensuring that they remain effective and safe. Egg-based vaccine production also requires a massive number of eggs to grow the virus—a particular headache when a pandemic is looming. “Egg production is a huge bottleneck,” Friede says. “You can’t just call your local egg farm and say tomorrow I need 10 million more eggs.”
In the 2009 H1N1 swine-flu pandemic, most vaccines did not arrive in the United States and Canada until after the pandemic had peaked. The United States stockpiles vaccines in advance of the most worrisome pandemic threats. BARDA sometimes spends hundreds of millions of dollars on stockpiles that could treat 20 million people. But that is an expensive gamble, as became clear in 2016 when the agency learned that its vaccine stockpile for the H7N9 flu family would no longer be effective against the latest H7N9 strains, so it had to create a second stockpile.
Whether or not a flu pandemic seems to be imminent, “we’re continually identifying viruses that are emerging, characterizing them and making vaccine virus preparations,” says Daniel Jernigan, director of the influenza division at the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia.
The vaccines made available in the Northern Hemisphere each October are usually based on strains picked by the WHO and partner organizations worldwide the previous February, when seasonal flu remains active. This leaves months in which viruses can evolve fresh tricks to dodge the vaccines.
“We would love it if the production time of the vaccine was shorter,” says David Wentworth, chief of virology, surveillance and diagnosis at the CDC’s influenza division. “If we could push vaccine strain selection forward to the end of the influenza season in the Northern Hemisphere, we would have a much more complete picture of all the different viruses that are circulating.”
“Timing is still everything when it comes to responding to changes in the influenza virus and ensuring that the vaccine is performing as well as possible,” says Danuta Skowronski, epidemiology lead for influenza and emerging respiratory pathogens at the BC Centre for Disease Control in Vancouver, Canada. “Looking at that historic reliance on egg-based production is at the top of many lists.”
CELLS BEAT EGGS
The best-established alternative to egg-based production is to make vaccines in other types of cell. For example, the four-strain (quadrivalent) Flucelvax from Seqirus in Maidenhead, UK, is generated in mammalian cells and has been approved for seasonal flu in both Europe and the United States. Such vaccines might be a closer match to circulating human flu viruses than egg-based vaccines, making them more effective, says Bright. This is because during vaccine development, candidate viruses are passed through many generations, looking for one that grows quickly and lacks bad traits. During this process, egg-based vaccines evolve away from human flu strains towards ones that work well in chickens, something that is less likely to happen in mammalian cells.
Cell-based manufacturing might have a slight speed advantage too, he adds: “We’re not relying on 900,000 eggs coming in from a bunch of different farms and waiting 11 days to inoculate those eggs.” However, even vaccines produced in mammalian cells are based on candidates developed in eggs before they are repeatedly groomed for growth.
An alternative method of production that does away with chicken eggs altogether involves recombinant technology. The quadrivalent FluBlok vaccine developed by Sanofi Pasteur in Lyon, France, is manufactured in this way. To generate FluBlok, genetically modified baculoviruses are used to insert tailored RNA into insect cells, where the vaccine proteins are subsequently grown.
In a pivotal clinical study (L. M. Dunkle et al. N. Engl. J. Med. 376, 2427–2436; 2017) that led to its approval by the US Food and Drug Administration in 2016, FluBlok was at least 30% more efficacious than a standard flu vaccine in adults over the age of 50, who are generally more vulnerable than younger people, says John Shiver, senior vice-president of global vaccine research and development at Sanofi Pasteur in Swiftwater, Pennsylvania.
Because recombinant-protein platforms do not rely on chicken eggs at any point, manufacturers can take the genetic sequence of the target virus strain and begin to produce vaccines almost immediately, shaving weeks off the production time, Bright says.
PLANT PARENTHOOD
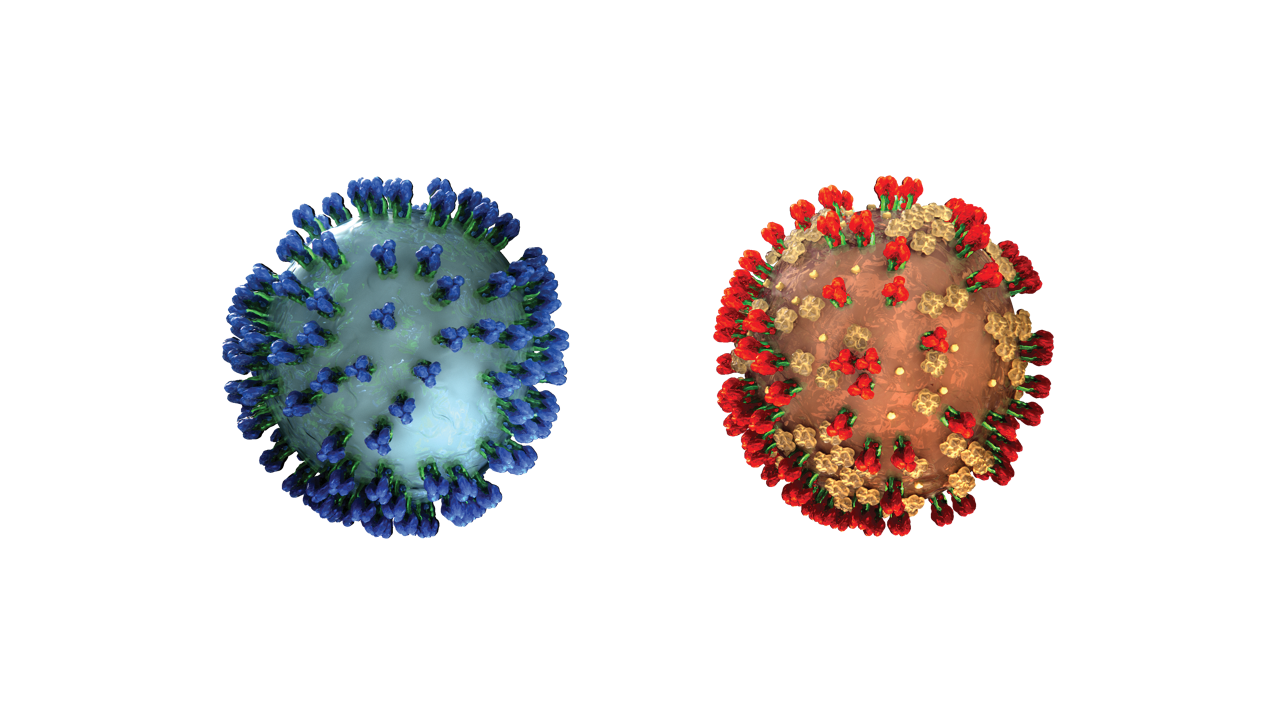
Many flu vaccines are designed as virus-like particles (VLPs). Under an electron microscope, VLPs look like viruses, and they can trigger similar immune reactions. But they are empty shells, lacking the RNA of an actual virus and posing no risk of infection.
VLPs can be generated in yeast or insect cells, but Medicago in Quebec City, Canada, takes a distinctive approach—growing the vaccines in tobacco leaves. “Plants are very complex systems and are capable of making very complex proteins,” says Nathalie Landry, the company’s executive vice-president for scientific and medical affairs.
Medicago produces its VLP vaccines by a process known as transient expression. Each plant is dipped into liquid that contains bacteria carrying recombinant DNA engineered to encode the desired proteins. A vacuum forces the bacteria into the leaves. The recombinant DNA enters the nucleus of leaf cells, where the protein is transcribed for a period of days. “This is a very quick process,” says Landry
Getting the recombinant DNA into the leaves takes just three to four minutes, and then the plants are incubated for five to seven days. “If we know which virus strain we need, we could start producing material five to six weeks after a declaration of a pandemic,” Landry says.
The results of phase II trials were positive and Medicago expects to complete its third phase III trial for flu this year. The company is preparing applications for regulatory approval in the United States and Canada, and is building a factory that would use its process to produce 30 million doses of quadrivalent vaccine each year.
KILLING BY MESSENGER
Another way to precisely match the target flu strains and have rapid, high-volume production is to use mRNA vaccines, but these are some way from regulatory approval. With mRNA, the final manufacturing steps occur not in a factory but in the person receiving the vaccine.
“The flu virus infects you and uses your body as a bioreactor to make itself,” says Hari Pujar, vice-president for technical development and manufacturing at Moderna Therapeutics in Cambridge, Massachusetts. “We are mimicking that path with an mRNA that encodes for flu proteins, so we are generating the vaccine inside the body.”
At its factory in Norwood, Massachusetts, Moderna can produce mRNA drugs on a pilot scale from raw materials. These vaccines do not require cells or proteins at all. Instead, workers make a DNA template to churn out the desired mRNAs in a bioreactor the size of a domestic water heater, rather than the giant tanks that are normally used to produce vaccines and other biological drugs. The mRNAs are then embedded in lipid nanoparticles. After injection into the recipient, the nanoparticles enter cells and deliver their mRNA cargos, which generate the proteins that constitute the vaccine.
As reported in May 2019, phase I clinical trials tested two first-generation Moderna mRNA vaccine candidates against two dangerous flu strains that lack approved vaccines. The studies found that the Moderna vaccines were safe and ought to be effective. Moderna is talking to potential industry and government partners about moving to commercial production.
Over at Sanofi Pasteur, Shiver sees several potential advantages of mRNA vaccines, which his company is investigating in collaboration with Translate Bio of Lexington, Massachusetts. He says that “mRNA probably has a good potential to scale up to very large scales, and frankly the same manufacturing facility could be used for more than one type of vaccine”. But he emphasizes that, given the huge investment required to turn vaccines into commercial products for seasonal flu, new manufacturing platforms such as mRNA must deliver improvements in the efficacy of vaccines.
The threat posed by pandemics is so great that government agencies such as BARDA might provide assistance for emerging vaccine platforms. “We’ve spent over US$6 billion on optimizing influenza vaccines, diversifying and augmenting the national supply chain,” says Bright. “We don’t think there is any pathogen on the planet that can devastate public health, lives, national security and our economic situation faster than a pandemic influenza virus.”
Eric Bender is a science writer in Newton, Massachusetts.

