Abstract and Introduction
Abstract Background: Non-ergot dopamine agonists (NEDAs) have become the gold-standard agents for the treatment of restless legs syndrome (RLS). While the efficacy and safety of these drugs have been widely studied, their effect on patients' health-related quality of life (HRQoL) has not been fully elucidated.
Objective: To better define the usefulness of NEDAs by assessing their impact on HRQoL.
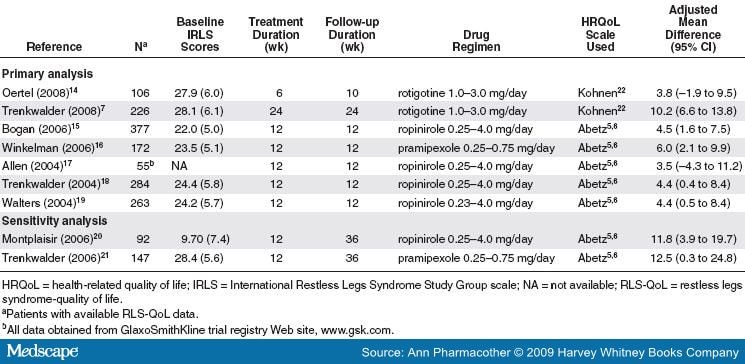
Methods: We performed a meta-analysis of randomized, double-blind, placebo-controlled trials evaluating the use of NEDAs in patients with RLS. A systematic literature search of MEDLINE, EMBASE, and Cochrane CENTRAL was performed from the earliest possible date through July 2008. Trials were included in the analysis if they evaluated NEDAs for the treatment of RLS and reported HRQoL using any RLS disease-specific HRQoL instrument. HRQoL data were pooled and evaluated using an inverse variance weighting approach as standardized mean differences (SMDs) and 95% confidence interval (CI). For trials reporting HRQoL data obtained using the Johns Hopkins RLS-QoL Questionnaire, adjusted mean difference data were pooled to calculate the weighted mean difference (WMD) and 95% CI.
Results: Seven trials (N = 1483) met all inclusion criteria. Patients with RLS taking NEDAs had significantly improved overall effect on HRQoL compared with those taking placebo (SMD 0.20; 95% CI 0.10 to 0.30; degree of inconsistency across studies [I2] = 0%). When analyzing trials using the Johns Hopkins RLS-QoL questionnaire, the results also showed improvement with NEDAs compared with placebo (WMD 4.72; 95% CI 2.96 to 6.47; I2 = 0%). Study conclusions were unchanged upon sensitivity analysis. The number of trials for each NEDA was small, limiting the usefulness of between-agent comparisons.
Conclusions: In patients with RLS, use of NEDAs showed improved HRQoL compared with placebo. Since pooled effect sizes observed in this meta-analysis appear to surpass accepted values for minimally important clinical differences, these improvements may be clinically relevant for the average studied patient. However, future studies evaluating long-term treatment of RLS with NEDAs are necessary, as are head-to-head comparative trials and economic assessments.
Restless legs syndrome (RLS) is a common disorder, with an estimated prevalence of 5-10% in the general population and increasing prevalence with age and in women.[1] Patients with RLS experience a strong urge to move their legs or other extremities while at rest. This urge is usually accompanied by an unpleasant sensation (creeping, crawling, tingling, pulling, pain) in the affected limb and may be temporarily relieved by movement. Symptoms are worse at night and are often diminished in the morning.
A number of agents have been used for the treatment of RLS symptoms, with a recent trend toward preferential use of non-ergot dopamine agonists (NEDAs) to attenuate both symptom severity and frequency.[2] Although NEDAs relieve some or all of the symptoms of RLS (eg, chronic sleep loss, disruptions to circadian pattern, disruptions to sedentary activities), they also may be associated with an increased risk of adverse effects.[3] Looking at these surrogate efficacy and adverse effect endpoints individually is worthwhile; however, the healthcare decision-maker cannot accurately discern how the interplay between these opposing variables will impact the terminal endpoint of health-related quality of life (HRQoL). HRQoL is an important endpoint in disorders such as RLS when the condition is not associated with terminal clinical outcomes (eg, mortality, stroke, myocardial infarction). While we recently performed a meta-analysis of controlled clinical trials demonstrating the impact of NEDAs as a class on efficacy and safety variables,[3] the impact of these drugs on overall HRQoL is not yet known.
Moreover, a recently published meta-analysis by Quilici et al.[4] suggested that pramipexole was superior to ropinirole in reducing RLS symptom severity (as depicted by greater reductions in mean International Restless Legs Syndrome Study Group [IRLS] scale scores and higher Clinical Global Impression-Improvement response rates) and resulted in significantly lower incidence of nausea, vomiting, and dizziness. Thus, different NEDAs (pramipexole, ropinirole, rotigotine) have differing effects on HRQoL in patients with RLS.[5,6,7]
In a meta-analysis evaluating HRQoL, differences between drugs in the class may be elucidated. Therefore, we conducted a meta-analysis of randomized controlled trials to better define the usefulness of NEDAs by assessing their impact on HRQoL as a class and by determining any differences noted between agents.
The Annals of Pharmacotherapy. 2009;43(5):813-821. © 2009 Harvey Whitney Books Company
Cite this: Effect of Non-Ergot Dopamine Agonists on Health-Related Quality of Life of Patients with Restless Legs Syndrome - Medscape - May 01, 2009.