The Paramedic’s Guide to Blood Oxygen and the Apple Watch Series 6
The heavy-duty portable air conditioners were doing an admirable job, considering we were sitting in vinyl tents in the middle of a black asphalt parking lot.
My team of medical professionals was next to a hospital in Puerto Rico after one of the most devastating hurricanes in history. Thanks to the judicious use of some shop vacs and sump pumps, you couldn’t even tell it had flooded the night before after torrential rains. While I enjoyed the cool air, I most definitely wasn’t enjoying my struggle to get a good blood oxygen reading on my patient.
She was an elderly diabetic suffering from severe dementia who was also quite dehydrated since she had stopped eating and drinking for no apparent reason. Between diabetes and dehydration, the peripheral circulation in her fingertip was pretty weak, and the hard-plastic clamshell sensor simply wasn’t working. The O2 reading would pop in and out, and when I looked at the waveform that measured the strength of her blood flow, it showed a weak and unreliable signal.
I tried switching to the disposable sensor, hoping the adhesive would form a tighter fit for a better reading, but it still didn’t work well enough, even when I tried it on her toes. Our patient wasn’t doing well, and we couldn’t even get a single solid reading to record with her vital signs, much less the continuous monitoring we needed for someone in her condition.
Since I was in the second wave of responders on this mission, I wasn’t sure how well our tents were stocked, but I managed to dig around and find a disposable earlobe sensor. They don’t always stay on well if the patient moves around, but they can often pull a decent signal due to the thinner tissue of the earlobe that allows more of the red and infrared light to pass through. But even that didn’t do what we needed. In the end, we had to put up with poor readings until we put enough IV fluids in her to increase her blood volume and improve her circulation.
As a paramedic, I have worked with pulse oximeters for thirty years in conditions ranging from sterile hospitals to mountaintops and ditches on the side of roads. I’ve watched them evolve from large, in-hospital devices to portable ambulance units to sub-$30 devices you can buy on Amazon and toss in your pocket. I’ve used them on many hundreds of patients under nearly any imaginable condition, and a few that would probably strain your credulity.
Perhaps this is why I find the new blood oxygen sensor in the Apple Watch Series 6 interesting and surprisingly accurate, even if it’s far from providing the same health and wellness value as the watch’s heart rate and ECG sensors. The use cases for recording data from an always-available pulse oximeter just aren’t as clear as those for measuring heart rate and finding cardiac arrhythmias.
What You Should Know about Oxygen Saturation
This might come as a surprise to some, but oxygen is incredibly toxic. Oxygen is highly reactive and can cause all sorts of cell damage when there is too much of it in the body. On the other hand, without it, we die within a few minutes. Our bodies are wonderfully optimized to take oxygen out of the atmosphere through respiration, transport it to cells through perfusion, and then move it into the cells, where it is used in respiration. Oxygen performs a final, critical step in cellular respiration, the process that provides our cells with the energy to function. (For the bio geeks out there, oxygen is the preferred electron acceptor in the electron transport chain that creates most of the ATP our cells use for energy).
For medical professionals, tracking how the body is using oxygen can provide a lot of information on overall health. Too little oxygen in the body can be caused by external factors like a lack of air pressure (not enough oxygen in the environment), breathing issues (not enough oxygen moved by the lungs), circulatory issues (blood isn’t pumped at the right rate to grab oxygen from the lungs or release it to enough cells), or metabolic problems (red blood cells have trouble accepting or releasing the oxygen molecules). Since our bodies use oxygen prodigiously, tracking blood oxygen levels is a powerful tool to help us figure out what’s wrong with patients, how bad they are, and if they are getting better or worse. It doesn’t tell us everything, but it tells us a lot.
There are several kinds of oxygen measurements, but the one we primarily focus on is arterial oxygen saturation (SaO2), the percentage of hemoglobin receptors currently carrying oxygen in our arteries. It’s a great measurement since it tells us roughly how much oxygen is available for our cells to use. That said, it isn’t perfect because it doesn’t tell us if there is enough hemoglobin in the first place, but when we draw blood and look at lab values, we can also count the hemoglobin (in a lab) and get a fuller picture.
There’s a problem with SaO2, however. To get a reading, we need to draw arterial blood and send it to the lab (venous blood has little oxygen since it’s all used up by then). The data is useful, but it provides only a point-in-time picture. If I have an asthma patient or someone having a heart attack in front of me, what I really want is a continuous picture of how they are doing. Oxygen levels can change incredibly quickly, so only a minute or two can mean the difference between life and death. Fortunately, while we can’t measure SaO2 without taking blood, we can use pulse oximetry to measure nearly the same thing by passing light of the right wavelengths through the body and seeing how much is absorbed and how much is reflected. We call this number SpO2, and it is nearly always the same as SaO2. Technically, SpO2 is an estimate of SaO2, but it’s instantaneous, non-invasive, and very accurate under most conditions.
How Medical Professionals Use Pulse Oximetry
Tracking a patient’s oxygen saturation (we just say “O2 sat” instead of SpO2) is one of the core vital signs, right up there with heart rate, respiratory rate, and blood pressure. As most of you probably know thanks to all the COVID-19 media coverage, a healthy person’s oxygen saturation is around 95–99%. It drops a bit at altitude, where I spend most of my career working. When I’m evaluating a patient at low or medium altitude, I tend to start paying attention when they are at 95%, I start thinking about treating them when their O2 sat drops below 93%, and I’m definitely taking action if they fall below 90%, usually by providing supplemental oxygen. The supplemental oxygen won’t fix the problem, but it buys me more time while I’m trying to understand and mitigate the underlying root cause.
We mostly use fingertip sensors since they are quick to apply and provide immediate results. In medical scenarios, we tend to use sensors attached to larger monitors that are certified to provide accurate results. Still, nearly every medical pro I know also has their own standalone fingertip sensor that they probably bought on Amazon or at a drugstore. These sensors provide pulse rate and O2 sat, and usually show a little waveform that helps us understand if we have a good reading (bigger waves equate with a stronger signal). They are also fiddly as all heck. If a patient is cold, is wearing nail polish, or has bled all over the floor, we aren’t going to get a good reading. I can’t tell you how much time I’ve spent messing around with and repositioning sensors to try to get a good number. Bouncing ambulances? A patient who rolls over and sleeps on their arm, reducing circulation? All of these will mess up the results and sound the alarms.
Problems aside, measuring blood oxygen is pretty definitive. If it’s low, there’s a problem, often one that we need to address right away. In the prehospital environment and the emergency room, I put a pulse oximeter on every patient. It’s typically most useful for respiratory and cardiac issues, or other issues like drug overdoses or diabetic emergencies that affect breathing or circulation. Anesthesiologists use them to keep sedated patients healthy. Sleep centers use them to help identify sleep apnea since if you stop breathing while you sleep, that will affect your O2 saturation.
The Limits of Consumer Blood Oxygen Tracking
As wonderful as a pulse oximeter is in a medical setting, it doesn’t tell us much about a healthy person, unlike, for example, tracking heart rate. Heart rate is wonderful for tracking workouts and exertion. It can tell us a lot about how well conditioned we are (resting heart rate), how well we are recovering (heart rate variability), and working out enough or too hard.
Blood oxygen? It doesn’t tell us anything about a workout. It won’t drop below normal levels since we just increase our breathing and circulation to keep the body in balance. It doesn’t tell us anything about recovery, our conditioning level, or nearly anything else. It is only an indicator of general health if you are suffering from some condition and need to see a doctor right away.
Remember, as a medical professional, I mostly use oxygen saturation to figure out how sick someone is and if I need to intervene immediately. I’ll use it to figure out if an asthma attack is severe and the inhaler isn’t working. To see if that chronic lung disease has gotten so bad that the patient needs to up their oxygen or get checked out. And yes, it’s so essential for COVID-19 patients that many facilities send patients home with a fingertip sensor and tell them to come back to the hospital if the number drops below 90%.
There are only four “wellness” situations where I think personal oxygen saturation tracking might help:
- Tracking it while you sleep could help identify sleep apnea.
- If you have a known lung disease or are otherwise worried about your immediate respiratory health, it can tell you if you are very sick or getting worse. However, it can’t prove you are healthy, just if things are problematic.
- If you suspect a respiratory problem, like COVID-19 or pneumonia, it can tell you if you need immediate help.
- It’s fun to watch it drop at altitude. Once. Maybe. On a slow day.
The Apple Watch 6 Is Surprisingly Accurate, for What That’s Worth
So what about the blood oxygen sensor on the Apple Watch 6? Tracking SpO2 on the wrist is tricky since you are evaluating only reflected light. The beams of light can’t pass all the way through the wrist as they do with a pulse oximeter sensor on the fingertip or earlobe. It’s a more challenging problem to solve due both to relying totally on reflected light and to the differences in positioning, ambient light, and movement. As my opening story highlights, SpO2 can be tough to measure even with advanced, clinical-grade fingertip sensors.
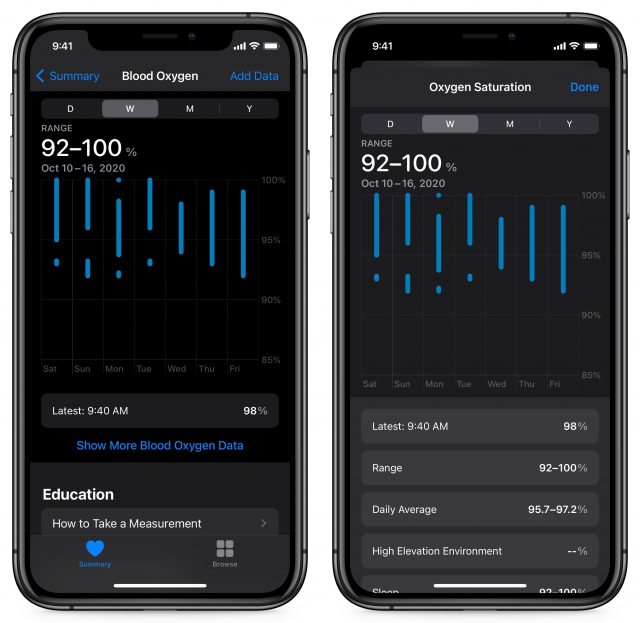
I’ve been testing the blood oxygen sensor on the Apple Watch Series 6 for the past few weeks under a range of conditions. I’ve been comparing my results against two consumer-grade fingertip sensors that I keep in my jump kits. Both my wife and I upgraded our watches so I could also track the differences between the two of us. And thanks to a weekend trip, I was able to evaluate how the Apple Watch worked at altitude. We wore them and took readings all day, during workouts, during hikes, while sleeping, and under different lighting conditions indoors and outside.
For the most part, the Apple Watch Series 6 is accurate when positioned well and without any movement. Readings typically directly matched my fingertip sensors or were within a single percentage point. Although Apple recommends taking readings only while your arm is resting on a flat surface, I found that I still get decent results if my band is snug and I hold my arm still and parallel to the ground.
Aberrant readings are usually obvious. If I see 100% or any number below 95%, I’ll reposition and try again. The Apple Watch will throw an error if you move too much or have a terrible reading, but its error checking isn’t consistent in marginal situations. My wife sees similar results, and although we have the same skin tone, I have a lot more arm hair in the way and her wrist is much thinner.
Tightening the watch band is just as likely to throw a bad result as loosening it too much, probably because it reduces blood flow slightly. If there is a lot of ambient light, as there is outside in the Arizona sunshine, I need to be more careful with my wrist positioning but can still get good results. I did get some strange looks when I stopped in the middle of a hiking trail to put on my fingertip sensor and compare the readings with the Apple Watch, but I also dress up as a Star Wars stormtrooper for a hobby, so I’m not overly sensitive to double-takes from passersby.
Our results while sleeping aren’t as similar. My readings consistently measure above 90%, with most of the automatic evening readings in the usual 96–98% range and a few aberrant low readings on some nights. My wife’s results aren’t nearly as consistent. She has a fair number of readings below 95% at night, with a few around 88–90%. That could be an indicator of sleep apnea, or maybe it’s just because she sleeps on her arm more, or perhaps her band is looser, or… you see the problem. Based on the Apple Watch alone, we just can’t use this data to make any wellness determinations.
This is the challenge faced not just by Apple, but also by Garmin, Fitbit, and all the other companies adding a blood oxygen sensor to their fitness trackers. How do they make this information useful to their customers? What kind of health and wellness decisions are informed by knowing your blood oxygen? Here’s my take on how to use it today and where I think it is headed.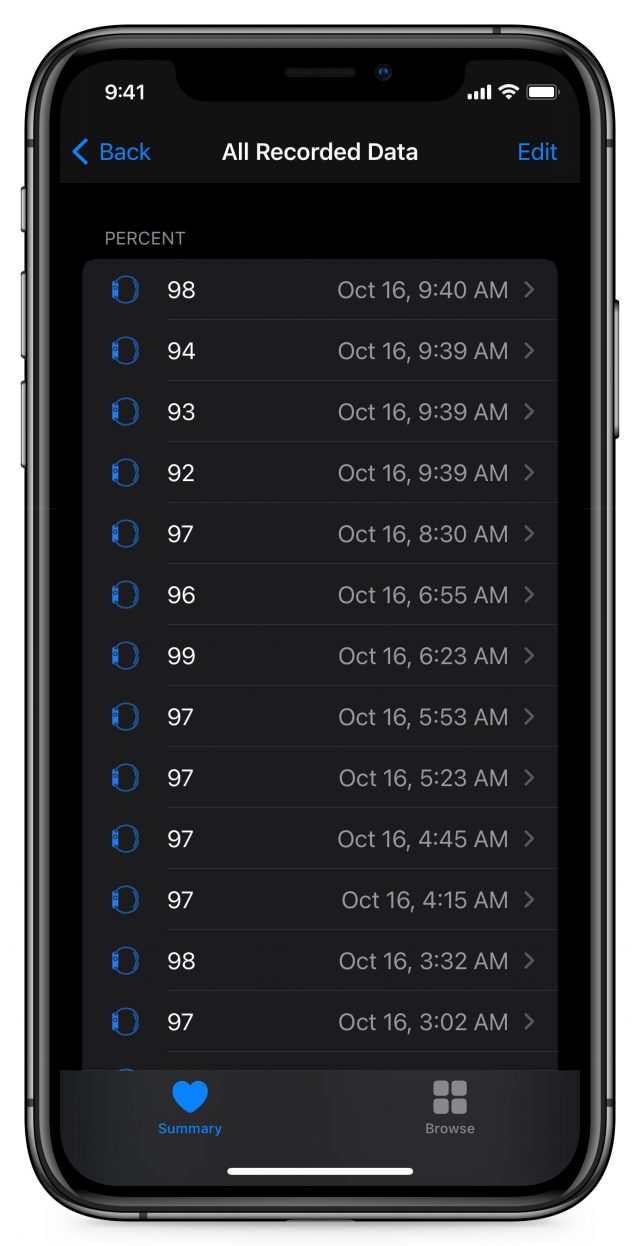
Right now, if you are sick or have a known respiratory issue, the Apple Watch Series 6 appears to be accurate enough to provide a quick indication that you should go dig out a dedicated pulse oximeter. It’s a matter of convenience—I’m nearly always wearing my watch, whereas my pulse oximeter is always in a bag or a cabinet. If you’ve used the Apple Watch Series 6’s blood oxygen sensor a lot and understand how it works for you, you might be comfortable relying on its numbers, but I’d be very cautious and take multiple readings. Like any other tool, you need to know how it works for you under good conditions before you rely on it when you might be sick. As someone who is periodically exposed to people suffering from COVID-19, I’m glad to have something so convenient if I need it, but I certainly wouldn’t use it to make any definitive medical decisions even if I were to get sick.
If you are healthy, the data produced by the blood oxygen sensor is just… interesting. You can’t use it to draw any conclusions on your health or wellness. I’m a quantified fitness freak, and there isn’t a darn thing I can learn about myself by tracking my blood oxygen levels while healthy.
The one area I think could eventually be compelling is helping to identify sleep apnea. Right now, its data isn’t sufficient for that, but the combination of the motion sensor, heart rate sensor, and blood oxygen sensor may someday improve enough to help identify an issue that degrades the health of millions but is hard to diagnose without an invasive sleep study.
Just as the Apple Watch’s heart rate sensor and ECG can help identify atrial fibrillation, tracking blood oxygenation while sleeping may indicate sleep apnea. I think this is where Apple is headed since the watch already takes background readings at night. The problem is that while its good readings are really good, we can’t tell the difference between bad readings and low readings. I strongly suspect this is something Apple can improve, perhaps by taking multiple serial readings and correlating with the heart rate sensor to better estimate if there is proper positioning.
Thanks to COVID-19, the world is far more aware of pulse oximetry and blood oxygen levels. Apple’s timing in releasing the Apple Watch 6 with a blood oxygen sensor was inadvertently impeccable. But while the Apple Watch Series 6 is accurate as long as you pay just a modicum of attention to proper positioning, it still needs to show it can provide more value to improving wellness. Knowing your blood oxygen level simply doesn’t tell you anything if you’re healthy. It’s a critical tool for evaluating serious illness, but in most situations, if you feel that bad, you should seek medical attention no matter what your watch tells you. Despite those limitations, I do think watch-based pulse oximetry shows promise for eventually helping identify sleep apnea, and having always-available readings may be useful if you have a respiratory illness and want to know when to take a deeper look.


That’s a really interesting comparison Rich. I had read elsewhere that the Apple Watch measurements weren’t that reliable for blood oxygen. But it seems to do pretty well. My partner suffers from sleep apnea but the lack of any alarm function on the Apple Watch when the reading drops (which the cheap finger devices offer) prevents it being much use except in review.
Thank you for that, that was a very instructive read and I found it really valuable.
Thanks for a good article based upon hands on experience. I to found the Watch 6 to match simultaneous Masimo readings with an occasional reading being 1 percentage point lower.
The automatic readings showed greater variation but I’ve not compared them as trying to wear the fingertip device over the same time frames is bit of a pain. So I’m impressed and intrigued but then I didn’t buy the watch for just O2 saturation—it’s another benefit.
I do find that using Apple’s Health App isn’t the best experience. Try viewing a specific measurement over the last month, my flicking finger sure gets a workout. I’d love to see Apple do a better job in data presentation, with ability to show variability ranges over the selected time period but perhaps also show the latest period over historical data over all your data—current month daily mean over all readings. But that’s just the data nerd in me…
Oh i forgot the question I had… elevation ranges, what does Apple consider to be a medium or high elevation reading? I always thought 3000 feet was medium while 8000 was high l yet I get a high readings at 7056 on the Donnor Pass.
I have extensive experience of one particular fingertip blood pulse oximeter and a variety of hospital and ambulance ones, from the patient perspective.
As an electronic engineer, I was interested to calibrate my cheap HKD100 (about USD13) fingertip blood pulse oximeter against the hospital one that looked like it was built for battle. The readings were never more than 2% different - and those reading from different fingers, which can give different readings - and usually identical, but that was in ideal conditions such as constant ward temperature of 19C/66℉ and me comfortable and at rest.
Lowest recorded SpO2 in hospital was about 63% briefly - probably under-reading of my actual oxygen saturation in my body core, but I have poor circulation in extremities when cold.
In one ambulance trip at 3am on a cold winter night, I saw my SpO2 measured by the ambulance oximeter plummet from low 90’s - 80’s - 70’s - 60’s etc and finally settled at 25%, where it stayed for at least 10 seconds, though it seemed like longer. I prayed hard and concentrated on controlled breathing with all my strength.
Obviously I survived, but one doctor pointed out that such a reading could be expected from “a dead fish” and was probably meaningless, saying more about my blood circulation than my oxygen saturation in core organs.
The point of this being that finger pulse oximeters of any type - fingertip or “military grade” looking instruments - can easily fail to give meaningful absolute readings - even when correctly attached to the “best” finger (index or middle finger of handwriting hand), but are still useful for relative readings to indicate a trend.
In such conditions as I described - a person with poor circulation when cold especially - I wonder if the Apple Watch may actually give a more meaningful reading, as the wrist would get better blood supply than the fingertips?
Your wrist certainly has better circulation, but taking a measurement from reflected light is more difficult than from light transmitted through a body part.
This is one of those questions that I think will only be answered by actual usage, not theoretical assumptions.
Replying to my own post. A little test of the watch reveals that Apple uses 1,500 meters (4,921 feet) as the point where it records as being a high altitude measurement. I live at around 4,515 feet so on the cusp… I’m. thinking it would be good for Apple to record/reveal the recording altitude in the Health App as it does for barometric pressure.
After purchasing and using the Apple Watch Series 6, I called Apple and they confirmed there is an alarm for low blood oxygen while sleeping. However, they would not tell me the low reading numbr that would trigger the alarm.