Abstract
Alveolar ridge preservation (ARP) is a method of decreasing bone resorption following tooth extraction and facilitating prosthetically-driven implant placement. An understanding of the physiological responses occurring after extraction and the effects of ARP are important in order to implement clinical procedures. ARP is a predictable way to reduce undesirable horizontal and vertical ridge reduction following extraction when dental implant treatment is to be delayed. Guided bone regeneration, socket fillers, socket sealers and growth factors have been used satisfactorily. However, there is currently no consensus on case selection, best clinical technique and material choice. Management of tooth extraction sockets is presented, with a focus on decision-making.
Similar content being viewed by others
Key points
-
Alveolar ridge preservation can prove beneficial for implant and pontic sites in certain cases.
-
Provides an assessment of the evidence and materials involved.
-
Suggests a clinical protocol for alveolar ridge preservation.
Introduction
Alveolar ridge preservation (ARP) is 'a procedure to arrest or minimise alveolar ridge resorption following tooth extraction for future prosthodontic treatment including placement of dental implants'.1 ARP was first described as 'bone maintenance' in 1982,2 and is synonymous with socket preservation, ridge preservation, socket grafting and socket augmentation. ARP commits to delaying implant placement by at least three to six months after extraction,3,4 with potentially longer treatment times compared with immediate and early (up to four months) implant placement.
ARP involves the use of a variety of graft materials, whether host-derived or transplanted, in order to fill an extraction socket and, usually, cover it immediately following tooth removal.5 This contrasts with ridge augmentation, which aims to increase the ridge volume beyond the existing skeletal envelope either at the time of extraction, before, or at implant placement.6 The potential advantages of ARP include maintenance of the existing soft and hard tissue envelope, a stable ridge volume for optimising functional and aesthetic outcomes, and simplification of subsequent treatment procedures such as generation of good soft and hard tissue volume for the time of implant placement.6
The aim of ARP is to maintain horizontal and vertical alveolar ridge form using bone grafts (autografts, allografts, xenografts or alloplastic materials); soft tissue grafts; guided bone regeneration (GBR) (with resorbable or non-resorbable barriers), biologically-active materials (growth factors) or combinations7 to reduce the loss of coronal alveolar bone height and width.
Allografts are defined as grafts between the same species and xenografts from a different species. Autografts are those harvested and applied within one individual. Alloplasts are synthetic materials. With the advent of a growing array of choices in materials, there is much interest in the best material and technique for ARP. No less than ten systematic reviews on the subject have been published since 2009,1,3,7,8,9,10,11,12,13,14 and the literature does not support the use of one technique, or material, as superior.
There is currently no consensus for case selection, clinical technique, or material choice.1,9 Alternatives to ARP, such as immediate and early implant placements, offer similar implant outcomes in the shorter term.15 The key to successful implant outcomes, regardless of the time of implant placement, is planning how to manage the bone volume at the proposed site. Salama and Salama16 have made recommendations for the ARP method that should be utilised depending on the socket anatomy (Table 1).16 This article aims to outline the current underlying evidence and methods of ARP, and provide guidance to aid clinical decision-making.
Alveolar ridge changes following tooth extraction
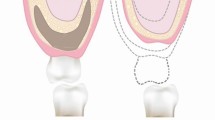
After extraction, a blood clot forms which is followed by formation of granulation tissue. Mineralisation then occurs, forming woven bone, which is later remodelled to lamellar bone.17 Bony changes after tooth extraction can occur for a number of months, with most changes occurring in the first three months.18 A summary of this process is shown in Figure 1.19,20,21 Bundle bone, also known as the lamina dura, lines the periodontal ligament around a tooth and is always resorbed after tooth extraction, regardless of whether an implant is placed immediately or not. Its thickness is 0.2-0.5 mm22 and it is fully resorbed by four weeks after extraction.23
A 50% reduction in the bucco-lingual width of bone has been estimated, in addition to a decrease in bone height at 12 months after extraction.18 Two-thirds of this reduction happens within three months. A recent systematic review reported mean alveolar bone resorption of 3.8 mm in width and 1.24 mm in height over the first six months following extraction.24 The buccal aspect of bone resorbs at a faster rate, resulting in a lingual shift in the bone crest with more pronounced resorption in the mandible.25,26,27 Where the buccal bone wall is 1 mm or narrower after tooth extraction, a median vertical bone loss of 7.5 mm of this buccal wall can be expected at eight weeks post-extraction. If buccal bone thickness is more than 1 mm after extracting a tooth, only 1.1 mm vertical loss of the buccal wall occurs.28 Ridge resorption has been suggested to occur due to disuse atrophy, a lack of blood supply and inflammation.29 Systemic and anatomical factors are likely to have an influence on the amount of resorption that occurs.17 These may include immunosuppression, impaired healing, genetics, smoking, periapical infection, chronic periodontitis, historical trauma, socket wall integrity, the number of adjacent teeth extracted, surgical trauma and prosthesis design.21,30
These physiological changes following tooth extraction can affect optimal dental implant positioning.31 An example is shown in Figure 2 which depicts a case with early implant placement. A narrow diameter fixture was placed in the 12 site that led to exposed palatal threads at an angulation requiring a cement-retained restoration. Although ARP could have slightly reduced the risk of these problems, there is limited evidence that further grafting is avoided or that the implant position is improved.9 The choice between a screw and cement-retained restoration is often limited by the apical aspect of the buccal envelope, not coronal ridge height and width. As ARP minimises the loss of coronal alveolar bone, it does not influence the prosthodontic implant restoration as much as the position of the alveolus.
Indications
The following indications are based on an Osteology Workshop's recommendations for ARP.6 ARP is used where tooth extraction is required and delayed dental implant placement in that site is likely at some point:
Implant placement is planned at a time point later than tooth extraction, such as:
- 1.
When immediate or early implantation is not recommended
- 2.
When patients are not available for immediate or early implant placement
- 3.
When primary stability of an implant cannot be obtained
- 4.
In adolescent people
- 1.
Contouring of the ridge for conventional prosthetic treatment; for example, pontic site development
The cost/benefit ratio is positive. Consideration may be given to the cost of ARP at the time of tooth extraction compared with the likelihood of GBR at a later date and its associated cost
Reducing the need for elevation of the sinus floor.
Some patients may be unable to commit financially to immediate or early implant placements and may therefore wish to keep their options for delayed implant placement open, in which case ARP may be an appropriate option.
Recently, a clinical decision tree described the clinical indications and limitations (Table 2),32 for soft tissue, hard and soft tissue, and hard tissue preservation. Hard tissue preservation was proposed for sockets with more than 50% loss of the buccal plate requiring ridge augmentation, and is therefore not part of our review.
Additionally, the authors would consider ARP when significant bone resorption is likely to impact on ideal implant placement. More than 1.8 mm of buccal bone is required following osteotomy for implants to minimise the risk of resorption.33 An evaluation of buccal bone thickness around teeth in the anterior maxilla showed that 90% had bone of less than 1 mm thickness.34 This suggests that ARP can be beneficial in these sites to provide a ridge with more than 1 mm thickness of buccal bone following osteotomy. A flowchart for decision-making regarding ARP is shown in Figure 3.
Evidence is lacking regarding predictive factors for the success of ARP. It is felt that routine surgical precautions should be taken and, in accordance with this, outcomes could potentially be affected by local and systemic factors. If extensive bone grafting is likely to be required in the future, the use of ARP techniques is most probably negated.
Outcomes
A recent Cochrane review identified eight studies with a follow-up of over six months assessing the outcomes of ARP using a variety of surgical methods, including with and without primary closure.1 Of the eight studies included, seven were at a high risk of bias and one was unclear. Consolidating the studies gave results from 233 extraction sites in 184 healthy adults. Exclusion criteria included significant infections in or close to the site, a full mouth plaque score over 30%, parafunction and participants smoking more than ten cigarettes per day. Most of the results were from four-walled sockets and implants were placed at least six months after ARP. Table 3 summarises the results of the systematic review. The studies showed ARP will decrease the amount of residual ridge resorption, however some bone loss will still occur.
ARP with xenograft or allograft showed around 2 mm less decrease in alveolar bone height and width compared with extraction alone. There was insufficient evidence to show differences between techniques regarding the amount of augmentation possible, complications, implant failure, changes in peri-implant bone levels and probing depths of neighbouring teeth. There are currently no trials assessing clinical attachment levels, aesthetic or prosthodontic outcomes with regards to ARP. The systematic review concluded that, at six-month follow-up, subjects have more bone, regardless of the materials or methods used for ARP.
While ARP was shown to be effective, some authors have argued that it causes hindrance of normal socket healing, has no benefit,35 and particles of different grafting materials may remain in the extraction socket for more than six months.36 A systematic review assessing the quality of grafted bone in sockets having undergone ARP with a variety of materials compared with naturally healed sockets identified eight studies, which showed considerable residual graft particles present (15-36%), at a mean of 5.6 months after ARP depending on the material used.37 A significantly decreased percentage of connective tissue (ranging from 17.9% to 33%) and an increased percentage of vital bone (ranging from 6.2% to 23.5%) was found in sockets having undergone ARP. Traditionally, a delay of six months has been advocated between ARP and implant placement, although the amount of vital bone available is similar at three and six months.38
Residual particles may interfere with normal healing and bone-to-implant contact. The degree of change in bone quality depends on the resorption rate of the graft material and its ability to encourage bone formation. Xenografts, which are increasingly used for ARP, have been shown to leave around 30% of residual material present, which is usually encapsulated within connective tissue.37,39,40 It is unknown whether this interferes with vital bone formation, but it is possible that decreased bone density caused by residual graft material could affect primary stability and additionally decrease implant-to-bone contact. In contrast, animal studies have shown that residual xenograft particles are separated from implant surfaces by mineralised bone.41,42 This would warrant further investigation.
A recent systematic review investigated the influence of ridge preservation on implant outcomes and concluded:9
- 1.
Alveolar ridge preservation procedures may decrease the need for further ridge augmentation during implant placement in comparison to unassisted socket healing
- 2.
There is no evidence to support the fact that implant placement feasibility is increased following ARP in comparison to unassisted socket healing
- 3.
The survival, success and marginal bone levels of implants placed in alveolar ridges following ARP are comparable to that of implants placed in untreated sockets
- 4.
No evidence was identified to inform on the possible superior impact of a type of ARP intervention (GBR, socket filler and socket seal) on implant outcomes. Currently, it is unknown if one biomaterial or treatment protocol is superior to another
- 5.
The majority of the studies evaluating implant-related outcomes after ARP procedures are presenting high or unclear risk of bias. Therefore, any clinical recommendation derived from these studies should be applied with caution.
Immediate and early implant placements offer the advantage of shorter implant treatment times. However, a recent systematic review has suggested that implants can be placed at 3-4 months after ARP, regardless of the bone substitute that is used, but the results and conclusions were based on a number of studies with no power calculations or intention to treat analysis.4 It is often an individual clinician's preference whether to place implants so early in grafted sites, but the clinical experience of the authors would suggest waiting at least six months before placing implants to allow graft maturation is preferable. The literature does not address the influence of preserving ridges on achieving ideal implant selection and position.9
Consent
ARP is carried out to maintain bone volume following tooth extraction, usually to aid prosthetically-driven implant placement. Patients should be informed of the procedure and specifically of the proposed materials to be used. They should be informed that ARP would involve a longer surgical time than extraction alone. Some patients may decline the use of xenograft materials due to religious or other beliefs and alternative materials can be utilised.
Surgical risks include bleeding, bruising, soreness, the need for sutures, infection, risk of damage to adjacent structures, recession, graft exposure, breakdown and failure. Additionally, patients should be informed that ARP cannot guarantee enough bone availability for implant placement and that further bone or soft tissue augmentation may still be required. The alternative option of extraction without ARP should also be discussed.
Materials
Methods include the use of a graft alone, the use of a graft and soft tissue graft/ membrane, or a membrane alone. Each method can be carried out with or without primary closure.
Guided bone regeneration (GBR)
The principle lies in preventing gingival epithelial and connective tissue from entering the defect via cell occlusive membranes in order to allow specific cells to regenerate lost tissues in the defect. A number of products are available for ARP and the materials often come in a number of different forms; some examples are shown in Table 4.
Barrier membranes are often utilised to maintain space for bone growth. These can be either resorbable or non-resorbable. Non-resorbable membranes show larger bone fill and favourable marginal tissue response. Resorbable membranes do not require second surgery for their removal and show good soft tissue healing.1
Non-resorbable membranes
These may be constructed of cellulose acetate filters (Millipore) or expanded polytetrafluoroethylene (e-PTFE or Teflon). Titanium has also been built into e-PTFE membranes to reinforce the structure and allow the membrane to tent up to maintain space for bony infill. e-PTFE alone has been shown to provide a gain in new bone formation of 1.5-5.5 mm at six to ten months.43
The negative aspects of non-resorbable membranes have meant they are less widely used more recently. A second surgery is required for their removal, which increases morbidity. Membrane exposure is relatively common due to extrusion, in turn significantly impairing healing and regeneration. To counteract this, high-density polytetrafluoroethylene (d-PTFE) has been developed. When left exposed for up to four weeks, no impairment of healing occurs. This means d-PTFE does not require releasing incisions to close the flap.44
Resorbable membranes
These include polyglycoside synthetic copolymers, collagen and calcium sulphate. These membranes have the advantage of not requiring a second surgical procedure for their removal. Collagen has the following benefits, which may assist in clot formation and stabilisation, and hence regeneration:
Acts as a haemostatic agent
Stimulates platelet attachment
Enhances fibrin linkage
Attracts fibroblasts
Easy to manipulate
Adapts to bone.
Despite these advantages, resorbable membranes have not been shown to give more or less bone than non-resorbable, although they are less likely to undergo exposure and infection.45,46
Acellular dermal matrix (ADM) is human skin tissue that has undergone repeated washing followed by freeze-drying. It was originally developed for burn victims and in dentistry is mostly used for mucogingival procedures in periodontal surgery. In ARP, ADM has been shown to preserve ridge thickness and this effect can be enhanced by the use of hydroxyapatite, which also helps to increase the width of keratinised tissues.47
Socket grafts
Socket graft materials work via osteoinduction and/or osteoconduction. Osteoinduction is the stimulation of bone growth via mesenchymal cells differentiating into osteoblasts. The most common material that facilitates this process is autogenous bone chips. Osteoconduction involves capillary and progenitor cell formation in and around the graft material, which acts like a scaffold. Most materials work via this method. Membranes can be used in combination with socket grafts.
Autografts
Extra-oral, for example, iliac crest and marrow block autografts, and intra-oral, for example, ramus of the mandible, maxillary tuberosity, post-extraction healing sites and bony exostoses are not used routinely for ARP due the relatively high morbidity.
Cancellous bone provides more osteogenesis than cortical bone, likely due to the abundance of cells in the marrow.48 Intra-oral autografts can be harvested as osseous coagulum, where bone is harvested with burs and mixed with blood, or bone blend, where harvested bone is triturated in a sterile amalgam capsule for 60 seconds.49 Commonly, bone is harvested via the use of a bone trap or scraping hand instruments, for example with a Rhodes back action chisel.
Allografts
The benefit is decreased morbidity due to the lack of a second surgical site. There are two types, mineralised frozen or freeze-dried bone (FDBA) and demineralised frozen or freeze-dried bone (DFDBA). FDBA works via osteoconduction and is resorbed more slowly than DFDBA. DFDBA may have the advantage of osteoinduction. These grafts are stored in tissue banks. These banks are not standardised, save for prevention of disease transmission, and allografts are obtained and prepared in a variety of ways.50 Tissue banks will screen and accept donors in a variety of ways, however all high risk groups for transmissible infections or Creutzfeld-Jakob disease are excluded as are donors with human immunodeficiency virus (HIV), hepatitis B, hepatitis C and Treponema pallidum (syphilis). Donors with malignancies are not specifically prohibited. In addition to taking a history, autopsies, blood tests and bone marrow cultures must be performed on potential donors. Autopsies have found considerable discrepancies compared with clinical diagnoses.50
DFDBA and FDBA show no difference in alveolar ridge dimension following ARP, however DFDBA shows greater vital bone (38.45% versus 26.63%) and less residual graft particles (8.88% versus 25.42%) at 4-5 months.51
The ideal particle size of these grafts has been suggested to be between 100-380 μm, as smaller particles are resorbed by macrophages and larger particles restrict space for vascularisation and additionally can be sequestered.52,53 Bone blend has the smallest particle size (21 x 105 μm), followed by osseous coagulum and FDBA (300-500 μm). Chiselled bone chips are the largest (789 x 1,559 μm).53 No differences have been found between DFDBA bone putty of different particle sizes in biopsies taken 20 weeks after ARP.54 When comparing cortical and cancellous FDBA, no difference in bone formation has been found but a greater loss of lingual ridge height was found in the cancellous group.55
Xenografts
DBBM is the most commonly used xenograft. Trade names include Bio-Oss, Cerabone, DirectOss and Hypro-Oss. Specimens taken nine months after ARP have demonstrated 26.4-35.1% vital bone, with coronal portions mostly formed of connective tissue (63.9%). The material was also present throughout the anterior maxillary sites, taking up approximately 30% of the volume.39 Most particles contact with cortical bone and minimally contact connective tissue. DBBM works primarily by osseoconduction56 and resorbs at a rate of 10% per year.57
Bio-Oss collagen, consisting of 90% DBBM and 10% porcine collagen, has been shown to act as a scaffold for tissue formation but does not encourage new bone formation. It preserves ridge shape and size but with decreased bone formation at 12 weeks compared with non-augmented sites (25% versus 44%).58 Other studies assessing this have given contradictory results.59 The authors speculate that this material may be used commonly, despite these equivocal results due to ease of use and marketing. Evidence suggests no difference in ARP between the use of membranes alone or membranes and deproteinised bovine bone material (DBBM).13,60
Alloplasts and growth factors
Examples include hydroxyapatite, tricalcium phosphate, calcium sulphate, bioactive glass polymers, polylactic acid, polyglycolic acid or collagen sponges. The materials are inert and work via osteoconduction.
Hydroxyapatite in combination with tricalcium phosphate, for example, Straumann Bone Ceramic, has shown similar results compared with DBBM when comparing alveolar bone crest levels assessed radiographically up to 32 weeks, histological assessment of sites at eight months, bone height, buccal and palatal wall thickness and the need for further grafting or periodontal indices around implants at one-year follow-up. A statistically significant difference of 1 mm in ridge width at eight months favouring the alloplast was found.61,62,63
Calcium sulphate has been shown to yield significantly less resorption and more mineralised bone when used in conjunction with platelet-rich plasma.64 When this combination was compared with a collagen plug alone, a significant difference in new vital bone of 66.5% versus 38.3% was found, respectively, at three months but no difference in ridge dimensions.65 Combining calcium sulphate with allografts does not appear to aid ARP.66
Sockets preserved with Bioglass, a silicate based glass, have shown a complete absence of new bone formation within the first six months, with lamellar bone infill at seven months.67
Hydroxyapatite has been shown to yield 31% vital bone at 6-8 months.68 Polylactic or polyglycolic acid (synthetic co-polymer) or collagen sponges can also be used and can be impregnated with other materials. Synthetic co-polymer sponges have shown similar ridge dimensions at three and six months compared with no ARP. The sites showed mineralised, well-structured bone with no residual graft material.69,70 Additionally, the Bio-Col technique involves placing DBBM particles followed by a collagen plug or membrane and has been shown to allow for implant placement.71 Collagen sponges combined with hydroxyapatite and cell-binding peptide or bone morphogenic protein have significantly higher mean bone density and greater bone augmentation (up to 2 mm mean ridge width) than collagen sponges alone.72,73 The addition of these proteins also meant sites were half as likely to require further grafting at implant placement. Similar percentages of bone vitality and ridge height changes were found.
Membranes and bone substitutes may,6,7,8,12,74 or may not,3,13,14,75 preserve more bone than bone substitutes alone, but it must be emphasised that the difference is not clinically significant.
Collagen sponges
Collagen sponges, for example, Haemocollagene, are usually type 1, non-denatured, freeze-dried collagen of bovine origin. They offer wound protection, blood clot stabilisation and facilitation of granulation tissue formation. These materials completely resorb within two weeks to three months. They can come in bullet shapes for ease of placement in sockets, and are cheaper than bone substitutes.
Although collagen sponges provide favourable bleeding control and graft protection, use of sponges alone appears to offer limited benefit compared with naturally healed sockets.76 Collagen sponges covering Bio-Oss77 and Puros78 (cancellous mineralised allograft) appear to offer significant ARP compared with extraction only.77,78 Gentamycin-soaked collagen sponges covered with free gingival grafts appear to offer borderline ARP compared with atraumatic extraction.79
Materials summary
Limited evidence is emerging to differentiate the various materials available.59 Findings from a recent systematic review of randomised control trials are summarised in Table 5.80 Other emerging materials, such as growth factors, human platelet-derived materials, platelet-rich fibrin, stem cells, cell therapy, enamel matrix derivatives and bone marrow require further evidence for validation.80
DBBM-containing materials covered by a membrane can currently be considered the 'gold standard' due to ready availability, lack of reported transmissible diseases, clinician acceptance and lasting effect.
Nevertheless, until more conclusive evidence is available, the choice will likely come down to operator preference, experience, case selection and material availability. Further research is required to assess any tangible differences in outcome between materials and methods. Slower resorbing bone substitutes, such as DBBM and bioactive glasses, appear to be preferable for longer planned delays in implant placement.
Socket sealing
This involves placement of a graft in the socket which is fully covered. Sockets may be sealed with coronally-advanced flaps, free or pedicle soft tissue grafts, ADM (for example, AlloDerm), xenografts (for example, Mucograft) or collagen sponges (for example, Haemocollagene). The need for primary closure to improve ARP outcomes is debatable from the literature, with some authors presenting results in favour of socket sealing,6,7,8,12 while others presenting results not in favour.3,13,14,75 However, particulate bone substitutes could easily become dislodged from extraction sockets, and some resorbable membranes require complete coverage, for instance, Bio-Gide. Raising a full thickness envelope flap and making adequate releasing incisions would allow tension-free coronal advancement with primary closure. The disadvantage of moving the mucogingival junction coronally could be subsequently overcome by apically repositioning a full thickness flap, either at first or second stage implant surgery.
An alternative technique is to use the hard palate to provide access to free and pedicle grafts. Free gingival grafts can be harvested with soft tissue punches of the appropriate size to cover the socket. Pedicle flaps are harvested from the palatal surfaces of the extraction socket, staying 3 mm away from the gingival margins of adjacent teeth. This is only suitable for maxillary teeth, and reduces the number of surgical sites and time. The pedicle will have its own vascular supply compared with free grafts. Xenografts can also be used and offer the advantage of colour match and no donor site morbidity. Mucograft Seal is a porcine-derived collagen membrane designed for primary closure in ARP. This membrane is thicker than the membranes used for regeneration and is designed to be left exposed to the oral environment.
Soft tissue grafting
Autogenous free gingival grafts and sub-epithelial connective tissue grafts appear to offer most predictable soft tissue grafting to preserve or gain keratinised tissue,81 when compared with resorbable membranes.82 Resorbable membranes offer the advantage of reduced morbidity and less surgical time. The colour match of the graft to adjacent tissues is also generally better with resorbable membranes compared to free gingival grafts.
Soft tissue grafting can be performed flapless or with minimal coronal advancement. A socket graft, for example, a collagen sponge, can be placed in the socket to support the soft tissue graft. Healing occurs in six to eight weeks, at which time implant placement can be commenced. Figure 4 shows placement of a sub-epithelial connective tissue graft at extraction of the left maxillary lateral incisor and canine and coronal advancement with primary closure.
An example of soft tissue grafting at time of extraction of 22 and 23 sites a) Pretreatment. b) Teeth extracted atraumatically. c Connective tissue graft with epithelialise collar sutured in situ. d) Wound closure. e) Buccal view of closed wound. f) Palatal site with dressing in place. g) Site after four weeks healing buccal view. h) Site at four weeks healing occlusal view
Socket shield technique
This is one type of technique that falls under a group of techniques termed 'partial extraction therapies' which also include the root submergence technique and pontic shield. These therapies aim to maintain the alveolar tissue using teeth themselves.83 The socket shield can act as an alternative to ARP, where a thin section of tooth is left in situ on the labial aspect and an implant is inserted into the socket on the palatal aspect of the tooth. The aim is similar to ARP in terms of maintenance of the buccal bone contour. Histological assessment of beagle dogs has shown cementum to regrow on the palatal aspect of the root fragment and onto the implant.84 Despite good implant survival rates at 4-5 years, with less than 0.5 mm vertical or horizontal bone loss in maxillary first premolar sites in ten patients, current four-year success rates are 80.5%.85,86 An alternative technique is the pontic shield, where part of a tooth is again left in situ; however, the socket is grafted instead of an implant immediately being placed, with a view to using the site underneath as a pontic. These techniques require further evidence for validation for routine clinical use and are mentioned here for completion.86,87
Clinical procedure
Based on the literature, it is difficult to give a precise protocol as there is no support for one technique over another. However, taking the evidence available into account, the authors would suggest the following protocol.
Pre-operative assessment of periodontal probing depths, bone sounding and radiographs can guide the clinician as to the likely anatomy of the socket. However, this should be confirmed clinically after tooth extraction before proceeding with ARP.
It has been reported that the effect of raising a flap on bone resorption remains unclear, however other studies have shown that the elevation of a full thickness flap can cause resorption of thin bone walls.30,37 This may occur as the buccal bone receives its blood supply from the periosteum and disruption of this affects its nutrient supply. The authors would advise avoiding raising a flap when planning ARP wherever possible.
With all methods, it is important to maintain an atraumatic extraction technique, maintaining as much bone as possible. Avoiding expansion of the socket can minimise the risk of fracturing thin bony walls. Applying circular, rotational or bucco-lingual forces with forceps is best avoided.30 Fine luxators, periotomes, piezo surgery and vertical tooth extraction systems may prove useful in this regard, although these are more relevant to individual, conical, straight roots. Multi-rooted teeth can be sectioned to aid extraction. The authors suggest avoiding any elevation or expansion on the buccal aspect in order to minimise the risk of any fractures of buccal bone. A common method for ARP is described below (Figures 5, 6, 7, 8, 9).
ARP of 11. a) Pre-treatment. b) Socket following atraumatic extraction of 11 and mechanical debridement. c) Deproteinised bovine bone material and porcine collagen 'plug'. d) 11 socket packed with bone graft material. e) 11 socket after closure with sutures. f) 11 socket one week after ARP. g) 11 socket two weeks following ARP
ARP of 37. a) Pre-operative radiograph showing 36 due for extraction and ARP. b) 36 sectioned. c) Use of periotome. d) Loosened fragments removed with no bucco-lingual force. e) Degranulation of sockets. f) DBBM with collagen ready for use. g) Sockets packed with DBBM and collagen mixture. h) Membranes held in situ with sutures. i) Socket healing at two week review
ARP of 22. a) 22 due for extraction and ARP due to vertical root fracture. b) Tooth extracted whole. c) Socket with buccal wall intact. d) Degranulation of socket. e) Porcine (Mucograft Seal) Membrane. f) DBBM in socket. g) Socket sealed with membrane. h) Site after three months healing with resin-retained bridge in situ showing buccal concavity of ridge 22 and highlighting instance of potential unpredictability with likely need for further grafting
Following tooth extraction, if existing granulation tissue is present this should be physically removed via debridement with a surgical instrument. Some operators prefer to irrigate the socket with saline, however a split-mouth study of 75 patients undergoing third molar extraction found a 3.5 times increased incidence of alveolar osteitis when irrigating, which could be due to the associated blood clot disruption.88 The authors suggest avoiding saline irrigation for this reason. Subsequently, enough grafting material to fill out the socket should be packed gently in, using an aseptic technique. The sockets should not be overfilled.89 Some clinicians prefer to moisten the graft material with saline or blood before use, in order to improve the handling. As the material picks up moisture in the socket, it will become easier to pack but others feel moistening the graft will reduce the capillary action of blood absorption onto the graft. The authors advise to place the graft material dry or to moisten it with blood rather than saline. Following placement of the graft material, it is beneficial to place sutures to help to hold the soft tissues in place. Additionally, cross sutures can help to stabilise the graft material. As an alternative, a membrane can be placed over the graft material, although it can be difficult to achieve primary closure to gain maximum benefit from the use of a membrane. A coronally-advanced, free or pedicle soft tissue flap, or xenograft materials can be used to achieve primary closure. This could be fixed in place with interrupted sutures. The authors advise utilising a membrane that has been designed to be left exposed to the oral cavity in order to seal the socket. This avoids the extra time and morbidity associated with either a coronally-advanced, free or pedicle flap and aids stabilisation and protection of the graft material from the oral cavity.
Routine post-operative instructions should be provided to the patient regarding analgesia and oral hygiene measures. The authors do not advocate the routine prescription of antimicrobials for ARP, given the risk of antimicrobial resistance and side effects. Sutures should be removed as soon as the wound is stable enough to decrease bacterial ingress and risk of wound infection.90 In the authors' experience, this is usually seven to ten days post-operatively.
Conclusions
ARP can be a beneficial method for maintaining bone volume to aid prosthetic delivery of implants. It is likely to maintain around 2 mm of bone width and height. A variety of materials and methods are available, which are summarised in this paper. Further research is still required to establish the influence of patient factors and different materials on ARP outcome, in addition to the long-term stability of graft materials. ARP would appear to be advantageous in cases where implant placement needs to be delayed, for example in young patients in whom growth is not yet completed, and for pontic sites around bridges. Slower resorbing graft materials, such as DBBM and bioactive glasses, would be preferable if the delay in implant placement is protracted by more than nine months. Implant outcomes in ARP appear to be comparable to immediate, early and delayed approaches. ARP could potentially reduce the need for a sinus lift. Complete preservation of the alveolar ridge after extraction is unlikely to be achieved, even if ARP techniques are used.
References
Atieh M A, Alsabeeha N H, Payne A G, Duncan W, Faggion C M, Esposito M. Interventions for replacing missing teeth: alveolar ridge preservation techniques for dental implant site development. Cochrane Database Syst Rev 2015; CD010176. DOI: 10.1002/14651858.CD010176.pub2.
Ashman A, Bruins P. A new immediate hard tissue replacement (HTR)TM for bone in the oral cavity. J Oral Implantol 1982; 10: 419-452.
Darby I, Chen S T, Buser D. Ridge preservation techniques for implant therapy. Int J Oral Maxillofac Implants 2009; 24 (Spec Iss): 260-271.
De Risi V, Clementini M, Vittorini G, Mannocci A, De Sanctis M. Alveolar ridge preservation techniques: a systematic review and meta-analysis of histological and histomorphometrical data. Clin Oral Implants Res 2015; 26: 50-68.
Jung R E, Philipp A, Annen B M et al. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol 2013; 40: 90-98.
Hammerle C H, Araujo M G, Simion M. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res 2012; 23 (Spec Iss): 80-82.
Horvath A, Mardas N, Mezzomo L A, Needleman I G, Donos N. Alveolar ridge preservation. A systematic review. Clin Oral Investig 2013; 17: 341-363.
Avila-Ortiz G, Elangovan S, Kramer K W, Blanchette D, Dawson D V. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res 2014; 93: 950-958.
Mardas N, Trullenque-Eriksson A, MacBeth N, Petrie A, Donos N. Does ridge preservation following tooth extraction improve implant treatment outcomes: a systematic review: Group 4: Therapeutic concepts & methods. Clin Oral Implants Res 2015; 26 (Spec Iss): 180-201.
Morjaria K R, Wilson R, Palmer R M. Bone healing after tooth extraction with or without an intervention: a systematic review of randomized controlled trials. Clin Implant Dent Relat Res 2014; 16: 1-20.
Ten Heggeler J M, Slot D E, Van der Weijden G A. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res 2011; 22: 779-788.
Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res 2012; 23 (Spec Iss): 22-38.
Vittorini Orgeas G, Clementini M, De Risi V, de Sanctis M. Surgical techniques for alveolar socket preservation: a systematic review. Int J Oral Maxillofac Implants 2013; 28: 1049-1061.
Weng D, Stock V, Schliephake H. Are socket and ridge preservation techniques at the day of tooth extraction efficient in maintaining the tissues of the alveolar ridge? Eur J Oral Implantol 2011; 4 (Spec Iss): S5-S10.
Chen S T, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants 2009; 24 (Spec Iss): 186-217.
Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles before implant placement: a systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent 1993; 13: 312-333.
Trombelli L, Farina R, Marzola A, Bozzi L, Liljenberg B, Lindhe J. Modeling and remodeling of human extraction sockets. J Clin Periodontol 2008; 35: 630-639.
Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 2003; 23: 313-323.
Cardaropoli G, Araujo M, Hayacibara R, Sukekava F, Lindhe J. Healing of extraction sockets and surgically produced - augmented and non-augmented - defects in the alveolar ridge. An experimental study in the dog. J Clin Periodontol 2005; 32: 435-440.
Al-Harbi S H. Minimizing trauma during tooth removal: a systematic sectioning approach. Eur J Esthet Dent 2010; 5: 274-287.
Wittneben J G, Weber H P. ITI treatment guide volume 6. extended edentulous spaces in the esthetic zone. New Malden: Quintessence, 2012.
Hubar J S. Quantification of the lamina dura. J Can Dent Assoc 1993; 59: 997-1000.
Araujo M G, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 2005; 32: 212-218.
Tan W L, Wong T L, Wong M C, Lang N P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 2012; 23 (Spec Iss): 1-21.
Cawood J I, Howell R A. A classification of the edentulous jaws. Int J Oral Maxillofac Surg 1988; 17: 232-236.
Pietrokovski J. The bony residual ridge in man. J Prosthet Dent 1975; 34: 456-462.
Atwood D A. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent 1971; 26: 266-279.
Chappuis V, Engel O, Reyes M, Shahim K, Nolte L P, Buser D. Ridge alterations post-extraction in the esthetic zone: a 3D analysis with CBCT. J Dent Res 2013; 92 (Spec Iss): 195S-201S.
Ashman A. Postextraction ridge preservation using a synthetic alloplast. Implant Dent 2000; 9: 168-176.
Araujo M G, Silva C O, Misawa M, Sukekava F. Alveolar socket healing: what can we learn? Periodontol 2000 2015; 68: 122-134.
John V, De Poi R, Blanchard S. Socket preservation as a precursor of future implant placement: review of the literature and case reports. Compend Contin Educ Dent 2007; 28: 646-653.
Jung R E, Ioannidis A, Hammerle C H F, Thoma D S. Alveolar ridge preservation in the esthetic zone. Periodontol 2000 2018; 77: 165-175.
Spray J R, Black C G, Morris H F, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol 2000; 5: 119-128.
Braut V, Bornstein M M, Belser U, Buser D. Thickness of the anterior maxillary facial bone walla retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent 2011; 31: 125-131.
Becker W, Clokie C, Sennerby L, Urist M R, Becker B E. Histologic findings after implantation and evaluation of different grafting materials and titanium micro screws into extraction sockets: case reports. J Periodontol 1998; 69: 414-421.
Carmagnola D, Adriaens P, Berglundh T. Healing of human extraction sockets filled with Bio-Oss. Clin Oral Implants Res 2003; 14: 137-143.
Chan H L, Lin G H, Fu J H, Wang H L. Alterations in bone quality after socket preservation with grafting materials: a systematic review. Int J Oral Maxillofac Implants 2013; 28: 710-720.
Beck T M, Mealey B L. Histologic analysis of healing after tooth extraction with ridge preservation using mineralized human bone allograft. J Periodontol 2010; 81: 1765-1772.
Artzi Z, Tal H, Dayan D. Porous bovine bone mineral in healing of human extraction sockets. Part 1: histomorphometric evaluations at 9 months. J Periodontol 2000; 71: 1015-1023.
Norton M R, Odell E W, Thompson I D, Cook R J. Efficacy of bovine bone mineral for alveolar augmentation: a human histologic study. Clin Oral Implants Res 2003; 14: 775-783.
Berglundh T, Lindhe J. Healing around implants placed in bone defects treated with Bio-Oss. An experimental study in the dog. Clin Oral Implants Res 1997; 8: 117-124.
Hockers T, Abensur D, Valentini P, Legrand R, Hammerle C H. The combined use of bioresorbable membranes and xenografts or autografts in the treatment of bone defects around implants. A study in beagle dogs. Clin Oral Implants Res1999; 10: 487-498.
Buser D, Bragger U, Lang N P, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res 1990; 1: 22-32.
Hoffmann O, Bartee B K, Beaumont C, Kasaj A, Deli G, Zafiropoulos G G. Alveolar bone preservation in extraction sockets using non-resorbable dPTFE membranes: a retrospective non-randomized study. J Periodontol 2008; 79: 1355-1369.
Carpio L, Loza J, Lynch S, Genco R. Guided bone regeneration around endosseous implants with anorganic bovine bone mineral. A randomized controlled trial comparing bioabsorbable versus non-resorbable barriers. J Periodontol 2000; 71: 1743-1749.
Chiapasco M, Zaniboni M. Clinical outcomes of GBR procedures to correct peri-implant dehiscences and fenestrations: a systematic review. Clin Oral Implants Res 2009; 20 (Spec Iss): 113-123.
Luczyszyn S M, Papalexiou V, Novaes A B Jr., Grisi M F, Souza S L, Taba M Jr. Acellular dermal matrix and hydroxyapatite in prevention of ridge deformities after tooth extraction. Implant Dent 2005; 14: 176-184.
Tomlin E M, Nelson S J, Rossmann J A. Ridge preservation for implant therapy: a review of the literature. Open Dent J 2014; 8: 66-76.
Diem C R, Bowers G M, Moffitt W C. Bone blending: a technique for osseous implants. J Periodontol 1972; 43: 295-297.
Malinin T I, Temple H T, Garg A K. Bone Allografts in Dentistry: A Review. Dentistry 2014; 4: 199-206.
Wood R A, Mealey B L. Histologic comparison of healing after tooth extraction with ridge preservation using mineralized versus demineralized freeze-dried bone allograft. J Periodontol 2012; 83: 329-336.
Shapoff C A, Bowers G M, Levy B, Mellonig J T, Yukna R A. The effect of particle size on the osteogenic activity of composite grafts of allogeneic freeze-dried bone and autogenous marrow. J Periodontol 1980; 51: 625-630.
Zaner D J, Yukna R A. Particle size of periodontal bone grafting materials. J Periodontol 1984; 55: 406-409.
Hoang T N, Mealey B L. Histologic comparison of healing after ridge preservation using human demineralized bone matrix putty with one versus two different-sized bone particles. J Periodontol 2012; 83: 174-181.
Eskow A J, Mealey B L. Evaluation of healing following tooth extraction with ridge preservation using cortical versus cancellous freeze-dried bone allograft. J Periodontol 2014; 85: 514-524.
Lee D W, Pi S H, Lee S K, Kim E C. Comparative histomorphometric analysis of extraction sockets healing implanted with bovine xenografts, irradiated cancellous allografts, and solvent-dehydrated allografts in humans. Int J Oral Maxillofac Implants 2009; 24: 609-615.
Tadjoedin E S, de Lange G L, Bronckers A L, Lyaruu D M, Burger E H. Deproteinized cancellous bovine bone (Bio-Oss) as bone substitute for sinus floor elevation. A retrospective, histomorphometrical study of five cases. J Clin Periodontol 2003; 30: 261-270.
Heberer S, Al-Chawaf B, Jablonski C, Nelson J J, Lage H, Nelson K. Healing of ungrafted and grafted extraction sockets after 12 weeks: a prospective clinical study. Int J Oral Maxillofac Implants 2011; 26: 385-392.
Barallat L, Ruiz-Magaz V, Levi P A Jr., Mareque-Bueno S, Galindo-Moreno P, Nart J. Histomorphometric results in ridge preservation procedures comparing various graft materials in extraction sockets with nongrafted sockets in humans: a systematic review. Implant Dent 2014; 23: 539-554.
Bashara H, Wohlfahrt J C, Polyzois I, Lyngstadaas S P, Renvert S, Claffey N. The effect of permanent grafting materials on the preservation of the buccal bone plate after tooth extraction: an experimental study in the dog. Clin Oral Implants Res 2012; 23: 911-917.
Patel K, Mardas N, Donos N. Radiographic and clinical outcomes of implants placed in ridge preserved sites: a 12-month post-loading follow-up. Clin Oral Implants Res 2013; 24: 599-605.
Mardas N, D'Aiuto F, Mezzomo L, Arzoumanidi M, Donos N. Radiographic alveolar bone changes following ridge preservation with two different biomaterials. Clin Oral Implants Res 2011; 22: 416-423.
Mardas N, Chadha V, Donos N. Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: a randomized, controlled clinical trial. Clin Oral Implants Res 2010; 21: 688-698.
Cheah C W, Vaithilingam R D, Siar C H, Swaminathan D, Hornbuckle G C. Histologic, histomorphometric, and cone-beam computerized tomography analyses of calcium sulphate and platelet-rich plasma in socket preservation: a pilot study. Implant Dent 2014; 23: 593-601.
Kutkut A, Andreana S, Kim H L, Monaco E Jr. Extraction socket preservation graft before implant placement with calcium sulphate hemihydrate and platelet-rich plasma: a clinical and histomorphometric study in humans. J Periodontol 2012; 83: 401-409.
Collins J R, Jimenez E, Martinez C et al. Clinical and histological evaluation of socket grafting using different types of bone substitute in adult patients. Implant Dent 2014; 23: 489-495.
Norton M R, Wilson J. Dental implants placed in extraction sites implanted with bioactive glass: human histology and clinical outcome. Int J Oral Maxillofac Implants 2002; 17: 249-257.
Froum S, Cho S C, Elian N, Rosenberg E, Rohrer M, Tarnow D. Extraction sockets and implantation of hydroxyapatites with membrane barriers: a histologic study. Implant Dent 2004; 13: 153-164.
Serino G, Biancu S, Iezzi G, Piattelli A. Ridge preservation following tooth extraction using a polylactide and polyglycolide sponge as space filler: a clinical and histological study in humans. Clin Oral Implants Res 2003; 14: 651-658.
Serino G, Rao W, Iezzi G, Piattelli A. Polylactide and polyglycolide sponge used in human extraction sockets: bone formation following 3 months after its application. Clin Oral Implants Res 2008; 19: 26-31.
Sclar A G. Preserving alveolar ridge anatomy following tooth removal in conjunction with immediate implant placement. The Bio-Col technique. Atlas Oral Maxillofac Surg Clin North Am 1999; 7: 39-59.
Neiva R F, Tsao Y P, Eber R, Shotwell J, Billy E, Wang H L. Effects of a putty-form hydroxyapatite matrix combined with the synthetic cell-binding peptide P-15 on alveolar ridge preservation. J Periodontol 2008; 79: 291-299.
Fiorellini J P, Howell T H, Cochran D et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol 2005; 76: 605-613.
Lekovic V, Kenney E B, Weinlaender M et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol 1997; 68: 563-570.
Wang R E, Lang N P. Ridge preservation after tooth extraction. Clin Oral Implants Res 2012; 23 (Spec Iss): 147-156.
Kim D M, Lim H C, Hong J Y et al. Validity of Collagen Plugs for Ridge Preservation in a Canine Model. Implant Dent 2017; 26: 892-898.
Kim Y K, Yun P Y, Lee H J, Ahn J Y, Kim S G. Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts. Implant Dent 2011; 20: 267-272.
Spinato S, Galindo-Moreno P, Zaffe D, Bernardello F, Soardi C M. Is socket healing conditioned by buccal plate thickness? A clinical and histologic study 4 months after mineralized human bone allografting. Clin Oral Implants Res 2014; 25: e120-e126.
Oghli A A, Steveling H. Ridge preservation following tooth extraction: a comparison between atraumatic extraction and socket seal surgery. Quintessence Int 2010; 41: 605-609.
Jambhekar S, Kernen F, Bidra A S. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: a systematic review of randomized controlled clinical trials. Journal Prosthet Dent 2015; 113: 371-382.
Thoma D S, Benic G I, Zwahlen M, Hammerle C H, Jung R E. A systematic review assessing soft tissue augmentation techniques. Clin Oral Implants Res 2009; 20 (Spec Iss): 146-165.
Thoma D S, Sancho-Puchades M, Ettlin D A, Hammerle C H, Jung R E. Impact of a collagen matrix on early healing, aesthetics and patient morbidity in oral mucosal wounds - a randomized study in humans. J Clin Periodontol 2012; 39: 157-165.
Gluckman H, Salama M, Du Toit J. Partial Extraction Therapies (PET) Part 1: Maintaining Alveolar Ridge Contour at Pontic and Immediate Implant Sites. Int J Periodontics Restorative Dent 2016; 36: 681-687.
Hurzeler M B, Zuhr O, Schupbach P, Rebele S F, Emmanouilidis N, Fickl S. The socket-shield technique: a proof-of-principle report. J Clin Periodontol 2010; 37: 855-862.
Baumer D, Zuhr O, Rebele S, Hurzeler M. Socket Shield Technique for immediate implant placement - clinical, radiographic and volumetric data after 5 years. Clin Oral Implants Res 2017; 28: 1450-1458.
Gluckman H, Salama M, Du Toit J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: Partial extraction therapy with up to 4 years follow-up. Clin Implant Dent Relat Res 2018; 20: 122-129.
Gluckman H, Salama M, Du Toit J. Partial Extraction Therapies (PET) Part 2: Procedures and Technical Aspects. Int J Periodontics Restorative Dent 2017; 37: 377-385.
Tolstunov L. Influence of immediate post-extraction socket irrigation on development of alveolar osteitis after mandibular third molar removal: a prospective split-mouth study, preliminary report. Br Dent J 2012; 213: 597-601.
Friedmann A, Dard M, Kleber B M, Bernimoulin J P, Bosshardt D D. Ridge augmentation and maxillary sinus grafting with a biphasic calcium phosphate: histologic and histomorphometric observations. Clin Oral Implants Res 2009; 20: 708-714.
Burkhardt R, Lang N P. Influence of suturing on wound healing. Periodontol 2000 2015; 68: 270-281.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalsi, A., Kalsi, J. & Bassi, S. Alveolar ridge preservation: why, when and how. Br Dent J 227, 264–274 (2019). https://doi.org/10.1038/s41415-019-0647-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0647-2
This article is cited by
-
Platelet-rich fibrin for rehydration and pre-vascularization of an acellular, collagen membrane of porcine origin
Clinical Oral Investigations (2024)
-
Characterization of bioactive substances involved in the induction of bone augmentation using demineralized bone sheets
International Journal of Implant Dentistry (2022)
-
A comparison between anorganic bone and collagen-preserving bone xenografts for alveolar ridge preservation: systematic review and future perspectives
Maxillofacial Plastic and Reconstructive Surgery (2022)
-
A 15-year unique observational study of intraligamentary local anaesthesia for posterior mandibular extractions
British Dental Journal (2021)