Gabriel de Erausquin first began to worry about the long-term impact of COVID on the brain when he read early reports out of Wuhan, China last January that survivors had lost two of their give senses--smell and taste. Worry turned to alarm when one of his medical assistants, a young mother who had come down with COVID-19 and had to be quarantined for a month, told de Erausquin, a neuroscientist, that she "couldn't care less" about being separated from her children.
Loss of smell, emotional detachment and other cognitive disorders among COVID-19 survivors has in recent weeks become an urgent medical issue. Some patients experience psychotic breaks. Others report strange neurological symptoms—tremors, extreme fatigue, phantom smells, dizziness and bouts of profound confusion, a condition known as "brain fog." In one early study of more than 200 patients in Wuhan, neurological complications were identified in 36 percent of all cases and in 45 percent of severe cases. Another study in France in the New England Journal of Medicine reported neurological symptoms in 67 percent of patients.
Although it's too early to tell what the long-term effects of COVID-19 will be on the cognitive health of survivors, scientists now fear the disease could feed a spike in dementia and other neurodegenerative diseases in the decades ahead. In addition, a growing number of COVID long-haulers already meet the clinical criteria for Chronic Fatigue Syndrome (CFS), a mysterious condition, also called myalgic encephalomyelitis, characterized by extreme fatigue, exercise intolerance and a whole host of other strange and debilitating neurological symptoms. Prior to COVID-19, CFS afflicted 2 million Americans.
If COVID long-haulers follow the trajectory of those who suffer from CFS, anywhere from 10-to-30 percent of those infected by SARS-CoV-2 may eventually experience long-term symptoms—a vast pool of additional millions with the condition who will place a new strain our healthcare burden, says Avindra Nath, clinical director of the National Institute of Neurological Disorders and Stroke (NINDS).
In recent months, the medical establishment has belatedly begun to respond to the crisis. Whereas COVID-19 was in early months considered mainly a respiratory virus, there's now a growing appreciation for its effect on other organs, including the brain. In addition, the media has increasingly begun to draw attention to the plight of long-haulers and their cognitive symptoms.
"The realization that there's a neurological effect has been really recent," says Nath. "I've been trying to beat that drum for quite some time. Patients have been complaining about it for months, but the scientists were not doing anything about it."
That is changing. Several large-scale initiatives to study the problem have been announced in recent weeks. The biggest question is how much money the National Institutes of Health (NIH) will devote to them. In December, Congress allocated roughly $1.25 billion to the agency for COVID-19 research, to be spent at the discretion of director Francis Collins. Although he has not yet stated whether he intends to fund brain research, agency officials told Newsweek that NIH will likely support large-scale studies that examine different recovery trajectories. (They spoke without attribution and declined to give specifics because the plans are still being hashed out.) An NIH spokesperson confirmed that NIH will "expand efforts to determine the scope of the post-acute COVID-19 symptoms, understand the biological processes involved and, ultimately, test methods to prevent and treat such symptoms."
Neuroscientists, meanwhile, are doing what they can and focusing their efforts on ways of intervening early in the onset of COVID-19 with treatments that minimize long-term damage to the brain. Once patients have lived for months or even years with the syndrome, treatment is more difficult. "That's what we'd like to avoid," says Dr. Walter Koroshetz, director of NINDS. "The sooner you can intervene, the greater effect your intervention is likely to have. People who are two and three years out and are still sick, it's a tougher road
A Landscape of Devastation
The connection between chronic neurological conditions and infectious viruses has long mystified scientists. In the wake of the 1918 Spanish Flu, an estimated 1 million people worldwide developed a mysterious, degenerative neurological syndrome known as encephalitis lethargica, which caused Parkinson-like muscle rigidity, psychosis and, in some cases, a zombie-like state. Neurologist-author Oliver Sacks featured the syndrome in a book that was the basis for the 1990 film Awakenings. The cause of this condition, which lingers for decades, is still not fully understood.
Prior to the introduction of antiviral therapies for HIV in the 1980s, dementia was observed in about 25 percent of infected patients. The AIDS virus often invaded the brain within the first two weeks of infection, smuggling itself in through infected immune cells and flooding the brain with neurotoxic proteins capable of laying waste to broad patches of neural real estate, according to Lena Al-Hartha of Chicago's Rush Medical College.

In the wake of the 2003 SARS and the 2012 MERS outbreaks, autopsies found that pathogens had penetrated the brains of some victims. NINDS' Nath, meanwhile, is currently following 200 former Ebola patients in Liberia still suffering from a mysterious set of chronic neurological symptoms that don't seem to be getting any better with time. Early efforts to investigate the strange effect COVID-19 seems to have on the brain of some victims have been hampered by the dangers of performing autopsies on deceased patients infected with a deadly pathogen that spreads through the air. In the first nine months of the pandemic, doctors performed only 24 studies involving brain autopsies of 149 individuals, according to one review.
Even so, those early studies, along with more recent ones, are beginning to provide clues.
Clare Bryce, a pathologist at Icahn School of Medicine at Mount Sinai, is part of a team that has so far managed to examine the brains of 63 autopsied patients. They work in a specially-sealed room, equipped with a ventilation system designed to keep air from escaping, accessible only to a single pathologist at a time clothed in a full-body protective suit and face shield.
In April, Bryce and her colleagues detailed the case of a 74-year-old Hispanic male who had arrived in the ER confused after experiencing several falls at home and, over the course of the following days, was variably "alert, agitated and combative." He died on day 11. When Bryce and her team examined his brain, it was shot through with dead patches of shrunken, discolored, oxygen-starved neurons, which were so fresh they had yet to be broken down by the brain's cellular maintenance crews—conditions they would see in roughly a quarter of the other 62 brains they examined in the months that followed. In an additional 11 patients, Bryce and her team found evidence of areas of devastation and cell death that were at least a couple weeks old. Some brains were swollen or shot through with clotted blood vessels.
"Sometimes there was a large area territory of dead tissue, but more commonly they're quite small and patchy within the periphery of the cortex, and also in the deep surfaces in the brain," Bryce says. "Some looked like they were anemic, some lacked oxygen and others had hemorrhages."
NINDS' Nath found similar damage in the fixed brain tissues of 16 deceased individuals shipped to him by the New York City Medical Examiner's office, which he examined through high-powered microscopes. He published the results in the New England Journal of Medicine.
Many of the patients Nath examined had died suddenly prior to seeking medical attention—one was found on the subway, another had been playing with his little sister—leading Nath to conclude their symptoms were so mild that they were unaware of being sick. Nevertheless, Nath also found their brains to be shot through with neuronal damage, inflammation and broken blood vessels.
The exact cause of this devastation remains a subject of vigorous debate among neuroscientists. It's also unclear whether the damage found in the brains of those who died from acute COVID-19 is mirrored in those who suffered milder cases and have since been hit with mysterious neurological aftereffects. The answers to those two questions could have major implications for future treatment.
An Invasion of the Brain
There are competing theories as to what might be causing the damage to the brain in COVID-19, but so far scientists are most concerned about two: viral infection and autoimmune reactions. The two are not mutually exclusive, and there could be other causes that vary from case to case.
The most ominous possibility is that SARS-CoV-2 takes up residence in brain cells, which appears to be the case in other viral diseases associated with chronic neurological problems. That would make it more likely that, over the long run, the COVID-19 virus might contribute to neurodegenerative conditions. Studies of large populations of people suggest a link between common viral infections, such as herpes simplex virus and the molecular level processes seen in Alzheimer's disease and dementia, says neuroscientist De Erausquin. Studies also show that some viruses burrow into the brain, lie dormant for a time and eventually reemerge.
That's why de Erausquin, an expert in neurodegenerative disorders at the University of Texas Health Center at San Antonio, was so alarmed early on—he feared that the perplexing clinical symptoms he was encountering might be explained by brain anatomy. Early in the pandemic, one of his medical residents, a young mother in her early 30s diagnosed with COVID-19 who'd experienced respiratory complications, fever and exhaustion, was forced to quarantine away from her young children in a hotel room for a month. As her acute symptoms began to fade, what troubled her most about the experience was not the separation itself, she told de Erausquin, but how she felt about it—she felt entirely detached.
"Cognitively, she realized that she should have been more concerned about her children, she should have been more concerned about her work," recalls de Erausquin. "But she couldn't care less. She had the lack of smell, the lack of taste and this profound emotional distancing, which bothered her a lot. It's very hard to explain that kind of emotional detachment, emotional dissociation, without having something going on in the amygdala."
The amygdala is a region deep inside the brain that's considered the seat of emotions. A loss of smell suggested a possible infection of the olfactory bulb, a small region of the brain accessed through the nose. The olfactory bulb happens to be located near those areas of the brain involved in memory and emotional processing, which could explain "brain fog" and the strange emotional disassociation.
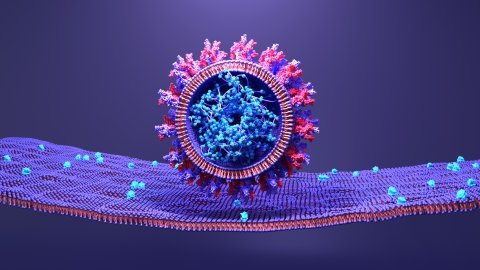
Scientists have recently found another reason to fear the brain effects of COVID-19. Although it was originally thought to be primarily a respiratory disease, it's now known to share some similarities with cancer in that it has the ability to metastisize, says Dr. Carlos Cordon-Cardo, director of the department of pathology at Mount Sinai Health System in New York City. It uses its famous spike-like proteins like grappling hooks to glom onto ACE2 receptors that are present in many types of human cells.
"The virus, even though it enters through the nose, can reach the lungs, the kidney, the liver, and now the brain because it goes into the blood vessels, it circulates, it travels into these tunnels," says Cordon-Cardo. "And then it can meet in a specific site to produce an extent of organ damage."
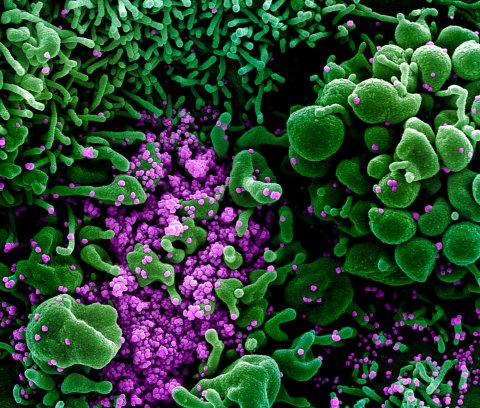
One alarming illustration of the potential destruction this might cause comes from the lab of Akiko Iwasaki, an immunobiologist at Yale. She and her collaborators created tiny colonies of stem-cell-derived neurons and the cells that support them, then exposed these "organoids" to the COVID-19 virus. It quickly infected some of the neurons, which then went into metabolic overdrive, and commandeered the cellular machinery to churn out copies of itself. In this frenzy of viral reproduction, the infected cells "sucked out all the oxygen" in the area, slowly starving the surrounding neurons of essential nutrients and sending them into a death spiral.
This "bystander" effect was also observed in experiments in brain organoids conducted by Alysson Muotri, a professor of pediatrics and cellular and molecular medicine at the University of California, San Diego. When he exposed his colonies of organoids to SARS-CoV-2, he found that the virus infected only a handful of neurons but had a dramatic impact. Within 48 hours, it had killed off 50 percent of the synaptic connections between various cells, which could wreak havoc in a living brain.
Virus that hides in brain cells might account for the delayed onset of some neurological symptoms. These infected cells, he suspects, may release some kind of neurotoxic or pro-inflammatory molecules capable of damaging the cells around them.
The evidence for the brain-infection hypothesis is inconsistent, however. In an autopsy of three patients with brain damage, Iwasaki and her collaborators found, only one had clearly been infiltrated by the pathogen. In the 63 brains that Bryce examined, she found viral fragments in only one, belonging to the initial Hispanic patient. And at NINDS, Nath has so far been unable to find any signs of brain infections, an outcome he calls a "major mystery."
"My expertise is in infection of the nervous system, so every pandemic I have studied the brain," Nath says. "I was very surprised was there was no virus that I could detect."

Immune Systems Run Amok
Nath suspects some long-haul symptoms might be explained by a hypothesis he favors for the cause of Chronic Fatigue Syndrome: The infection has left its victims with a persistent activation of the immune system, which has pushed the body into a low-level state of war with itself. Indeed, the many ways acute COVID-19 manifests in patients can be explained by how each individual's immune system reacts to the disease. The same may well be true in those suffering from chronic symptoms.
These two hypotheses for long-haul COVID-19—autoimmunity and direct brain infection—are "not mutually exclusive," Yale's Iwasaki notes.
She examined the impact of a special class of immune cells called "autoantibodies"—molecular-level cellular assassins that appear to be specially-designed and directed to seek out and attack proteins produced by the patient's own body. After analyzing autoantibodies based on blood samples culled from 194 patients and healthcare workers infected with the virus, and comparing them to blood drawn from 30 uninfected healthcare workers, she found the COVID-19 patients exhibited "dramatic increases" in autoantibody activity, with the specialized cells in many cases targeting other immune cells. Of the 15 patients who died during the study, all but one were found to have unleashed autoantibodies on other elements of the immune system needed to effectively fight off the disease. The autoantibodies also appeared to be attacking molecules involved in blood clotting, connective tissue and cells in the brain and central nervous system, mistakenly identifying them as invading pathogens that needed to be eliminated. Iwasaki published a report in the British Medical Association's flagship journal in December.
Indirect attacks may account for the cellular damage to brain tissue seen in autopsies. By some estimates, the human body is lined with 60,000 miles of blood vessels, and ACE2 receptors, which SARS-CoV-2's spike proteins target, are ubiquitous on the "endothelial" cells that line the outer surface of these blood vessels. "The brain," says NINDS' Koroshetz, "is the most vascularized organ in the body. It's basically like a gigantic complicated tangle of blood vessels."
Destruction of the outer lining of tiny capillaries in the brain, which has been spotted in a number of autopsies, could break down the blood-brain barrier, cause leakage, lead to blood clots and cause the whole brain to swell up "almost like a sponge put in water."
"That in itself is a problem because that allows things that are not supposed to go into the brain and the blood to actually get in, and that can set up problems in terms of the function of the brain tissue," Koroshetz says. "It also brings in an inflammatory response to kind of sop up the injury or sop up the proteins that are getting in that shouldn't be there."
In addition to pathogens, this breakdown can allow the unchecked infiltration of white blood cells, which Koroshetz describes as the "tanks" of the immune system, because they attack infected areas with far more firepower and far less specificity than the COVID-specific antibodies, which are the "guided missiles" of the immune arsenal.
The process of verifying these hypotheses, and myriad others to emerge from the study of the disease, is only just beginning.
More Work to Do
De Erausquin and other brain specialists like him have been largely unable to get people to listen to their concerns and pony up the money needed to answer what they see a series of urgent questions. These entail not only the long-term effects COVID-19 will have on the brains of survivors, but also to what extent chronic neurological symptoms will add to the burden the world's rapidly aging population is already expected to have on healthcare systems in the decades ahead.
That may be changing. In recent weeks, the media has turned the spotlight onto COVID-19 long haulers and the strange neurological symptoms that persist after the virus is cleared from their bodies.
Last month, de Erausquin and colleagues around the world unveiled the blueprint for a massive, international research study involving researchers from more than 30 nations, with as many as 40,000 participants that will follow survivors in the years ahead. The study, which will initially receive funding from the Alzheimer's Association and support from the World Health Organization and, hopefully, from national health authorities around the world, aims to explore the cause of the mysterious effects COVID-19 often seems to have on the brain, and track its long-term impact.
Others studies may follow. The NIH has allocated roughly $1.5 billion in COVID-related funds through the last COVID-19 relief bill and is likely to fund a major study aimed at examining the question of what constitutes a "normal recovery" and what differentiates that from the experience of so-called "long haulers," says NINDS' Koroshetz. And researchers are in the process of setting up collection methods and standardizing procedures between four different groups treating hundreds of long-haul patients, including at Mount Sinai Hospital, that will examine the neurological symptoms in the hopes of finding the causes, according to Iwasaki.
Research that starts with observations at early stages of the disease could be "an excellent opportunity" to increase understanding of chronic fatigue syndrome and other brain diseases, says Nath. But, he warns, insights won't necessarily come easy. "Look at Alzheimer's, we put billions of dollars in it every year, we've been studying it for decades, and we don't even know how to diagnose the disease, let alone treat it," he says. "Cracking neurological disease is not an easy task. It takes time."
Newsweek, in partnership with NewsGuard, is dedicated to providing accurate and verifiable vaccine and health information. With NewsGuard's HealthGuard browser extension, users can verify if a website is a trustworthy source of health information. Visit the Newsweek VaxFacts website to learn more and to download the HealthGuard browser extension.
Correction (2/11/2021, 3:55 pm EST): The NIH received $1.25 billion for COVID-19 in December, not $1.5 billion as previously stated.