Officials with London Health Sciences Centre are touting a new non-invasive procedure to repair life-threatening aortic aneurysms which drastically cuts down a patient’s recovery time.

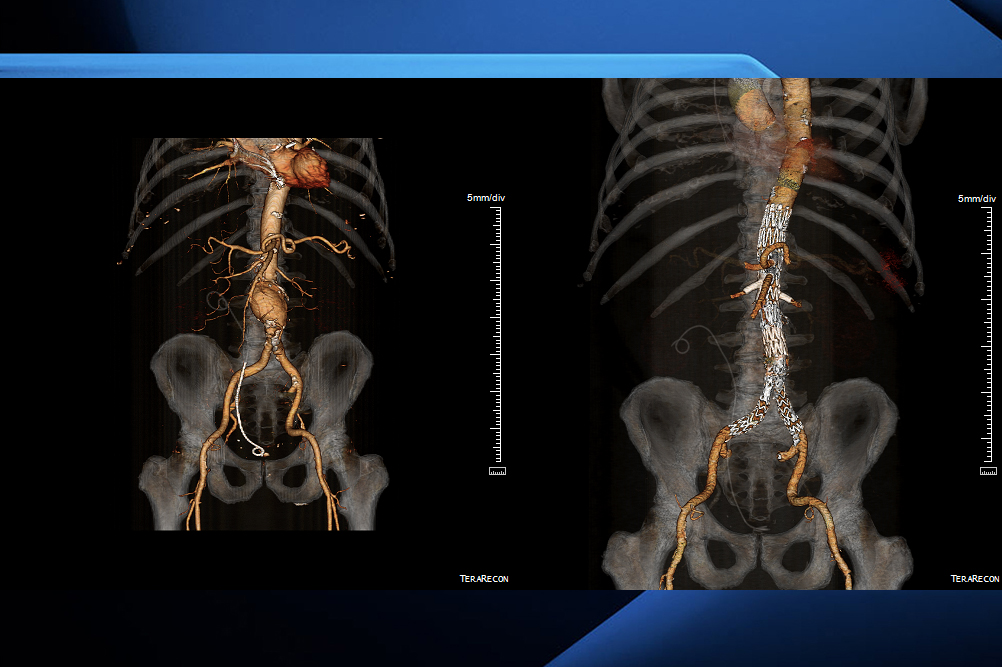
The procedure, a fenestrated endovascular aneurysm repair, or FEVAR for short, is carried out to repair extensive aneurysms in the aorta, the body’s largest artery, as well as in the chest and abdomen, LHSC officials say.
Previously, patients undergoing open surgery to repair the life-threatening aneurysms faced an 11-month recovery timeline, including several weeks in the hospital.
The new procedure reduces that hospital stay to a matter of days and the total recovery process to roughly a month.
LHSC says it’s the first health-care centre in the region to offer the procedure.
Officials with LHSC’s vascular surgery team have described the procedure as a “game changer,” saying it allows surgeons to remove an aortic aneurysm quickly and effectively compared to previous methods, which involved opening up the chest or abdomen, cutting the aneurysm out, and replacing it with a graft.
“In the mid-’90s to late-’90s we had, sort of, invented a way to replace them using X-ray guidance, and we would put in a fabric-covered stent … that would allow us to reline the inside of the aneurysm,” said Dr. John Landau, a vascular surgeon at LHSC, in an interview with Global News.
- Buzz kill? Gen Z less interested in coffee than older Canadians, survey shows
- ‘She gets to be 10’: Ontario child’s heart donated to girl the same age
- Bird flu risk to humans an ‘enormous concern,’ WHO says. Here’s what to know
- Canada updating sperm donor screening criteria for men who have sex with men
“But even that required us to make two fairly large incisions over the femoral artery in the groin to introduce the equipment that allowed us to place those stents.”
With FEVAR, LHSC officials say surgeons use a custom-made endovascular stent-graft that, with X-ray guidance, is placed in the aorta through a tiny incision near the groin roughly the size of a standard drinking straw.
“People have been doing these advanced branched grafts for at least ten years,” Landau said. “But to be able to do them percutaneously through these small holes with the combination of techniques and equipment that we have, doing a replacement this extensive is only something that’s been possible in the last year or two.”
Some patients will still need the conventional open procedure, Landau says, but being able to offer to those eligible the non-invasive option, which shortens recovery time and minimizes the risk of major complications, “is really a win for patients and the physicians treating them in the hospital overall.”
Highlighted was the case of Thomas Barker, 75, who underwent the procedure two and a half months ago after doctors discovered an aortic aneurysm following an aortic valve and coronary bypass operation in 2017.

“Mr. Barker’s case went up very close to all of these blood vessels that supply the major organs of the abdomen,” Landau said.
“We had a device that was custom made to incorporate all of those branch blood vessels to his major organs with additional branch stents that go into those blood vessels, (ensuring) that the entire system of stents that we put in exclude blood flow from the aneurysm.”
Speaking with Global News on Tuesday in a joint interview with Dr. Landau, Barker said that he was doing well and had gotten back to living a normal life.
The size of the aneurysm was such that Barker says he was “all for” the procedure, because not doing it would be potentially fatal.
“From the time it was diagnosed, (it was) about three years ’til it got to the point of surgery. Needless to say, the day of the surgery, it turned out one day of surgery, and two and a half days later, I was home,” he said.
“Today… we just checked over the the CT scan and everything is in order. I feel good and I’m looking forward now to continue on with my life.”
Following the success of the FEVAR procedure, LHSC says it has several similar surgeries booked for this fall.
— with files from Devon Peacock







Comments