- New research shows that all hormonal birth control methods raise your risk for developing breast cancer.
- Researchers found that your risk increases with advancing age.
- Experts explain what you should know if you’re currently on the pill or have been in the past.
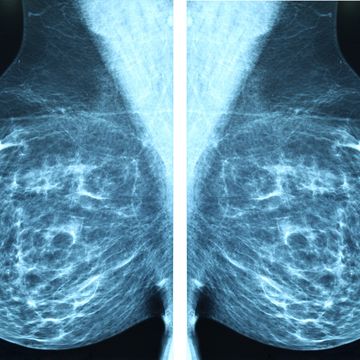
The effects of hormonal birth control on breast cancer risk have been studied for decades. Many studies over the years have shown that hormone-containing birth control options, specifically estrogen and progesterone, may slightly raise your risk of developing breast cancer later in life. However, new research is shedding light on the risk associated with progestogen-only contraceptives, such as intrauterine devices (IUD) or the mini pill, whose usage has increased substantially in recent years.
A new study published in PLOS Medicine by researchers at Oxford Population Health’s Cancer Epidemiology Unit found that use of progestogen-only hormonal contraceptives is associated with a 20-30% higher risk of breast cancer.
The researchers analyzed data from 9,498 women who developed invasive breast cancer between ages 20 to 49 and 18,171 women without breast cancer who acted as controls. The data were collected by the Clinical Practice Research Datalink (CPRD). It found that 44% of women with breast cancer and 39% of women without breast cancer included in the study had a prescription for a hormonal contraceptive an average of three years before diagnosis, around half of whom were last prescribed a progestogen-only contraceptive.
Researchers found that there was a significant increase in risk of breast cancer associated with hormonal contraceptive use, regardless of the type of hormonal contraceptive. They found a 23% increased risk in women who used a combined (estrogen and progestogen) pill, 26% increased risk in women who used a progestogen-only pill, 25% increased risk in women who used an injected progestogen, and 32% increased risk in women who used a progestogen-releasing IUD.
Researchers also found that the increased risk of breast cancer associated with oral contraceptive use declined after stopping use, decreasing the risk by half after five or more years after stopping. It was also determined that the risk of breast cancer increased with birth control use as women advanced in age. The researchers estimated that over a 15-year period, the risk of developing breast cancer in women who used oral contraceptives for at least five years ranged from 0.008% for use from age 16 to 20, to 0.265% for use from age 35 to 39.
Kirstin Pirie, statistical programmer at Oxford Population Health, and one of the lead authors of the study, said in a press release, “The findings suggest that current or recent use of all types of progestogen-only contraceptives is associated with a slight increase in breast cancer risk, similar to that associated with use of combined oral contraceptives.” She continued to say that given a person’s underlying risk of developing breast cancer increases with advancing age, the risk of breast cancer associated with either type of oral contraceptive will be smaller in women who use it at younger ages. “These excess risks must, however, be viewed in the context of the well-established benefits of contraceptive use in women's reproductive years,” she added.
First, what contraceptives qualify as hormonal birth control?
The birth control pill, patch, and vaginal ring, as well as Depo-Provera injections, and implants provide systemic hormones (into the bloodstream) for contraception, says Erika Banks, M.D., board-certified OBGYN at NYU Langone Hospital, Long Island. “The progesterone IUD is also hormonal but focuses the hormone inside the uterus so has a lesser systemic effect.”
How does hormonal birth control affect your risk for breast cancer?
The pill itself does not cause breast cancer, but the same hormones that control a menstrual cycle can also drive the growth of breast cancer, explains Jessica Jones, M.D., board-certified oncologist at UTHealth Houston and Memorial Hermann. “If a woman has any irregular breast cells that are using estrogen to grow—the pill may give those cells ‘fuel.’” Therefore, it is important for a doctor to also look at the age of a woman when they prescribe birth control, she adds.
The risk of breast cancer for people in the age groups that most use hormonal contraception is incredibly small, explains Dr. Banks. “This study confirmed what we know—that the overall risk of breast cancer among those who use hormonal contraceptives is very low.” However, she notes that this risk does not continue after about five years since last use.
For women who are already at increased risk of breast cancer, there are both personal, inherited, and environmental factors at play, says Dr. Jones. “Having had started puberty early, or menopause late; Having a history of breast biopsies; Having a family history of breast cancer; are all important risk factors to consider.”
Anyone who uses hormonal birth control methods has some risk, though the degree of risk depends on age, says Parvin Peddi, M.D., director of Breast Medical Oncology at Saint John’s Cancer Institute. “The risk is much lower for women in their twenties and lower thirties than it is for women in their upper thirties and forties.”
What to know if you currently use hormonal birth control
Any medication has risks, says Dr. Banks. “The risk of breast cancer in the early reproductive years, when most people take hormonal birth control, is incredibly low at baseline.” This risk is all very low, and the contraceptive benefits are high, as these are some of our most effective forms of birth control, she notes.
Dr. Banks continues to say that the non-contraceptive benefits of hormonal contraception are well-known, including actually decreasing risk of ovarian, uterine, and colon cancer, as well as the reduction in heavy bleeding, painful cramps, and many premenstrual symptoms. The benefits of hormonal contraceptives in preventing pregnancy are also important, she says. “In 2015, the maternal mortality rate in the United States was 26.4 deaths per 100,000 women which is double the risk of developing invasive breast cancer.”
The bottom line
Experts are not saying that birth control methods should be avoided, says Dr. Peddi. “We aren’t saying don’t use it, but we are saying don’t just use progestogen-only options if you perceive that one type is better than the other. All have breast cancer risk. Choose the one that’s right for you by discussing with your doctor.” She adds that, “The older a woman is that uses it, they should also be aware that procedures like a vasectomy or tubal ligation could be safer options to avoid pregnancy, especially in higher risk women.”
If you think you may be at higher risk for developing breast cancer, talk to your doctor about your concerns, and if you think you may be at increased risk of breast cancer because of family history or your own personal breast history, ask for a breast cancer risk assessment, suggests Dr. Jones. “Please ask your doctor for a breast cancer risk assessment, or ask for a referral to a specialist who can provide this assessment,” she adds. “Even women who are at increased risk of breast cancer can mitigate this risk by enhanced screening.”
Madeleine, Prevention’s assistant editor, has a history with health writing from her experience as an editorial assistant at WebMD, and from her personal research at university. She graduated from the University of Michigan with a degree in biopsychology, cognition, and neuroscience—and she helps strategize for success across Prevention’s social media platforms.