Few states cover fertility treatment for same-sex couples, but that could be changing
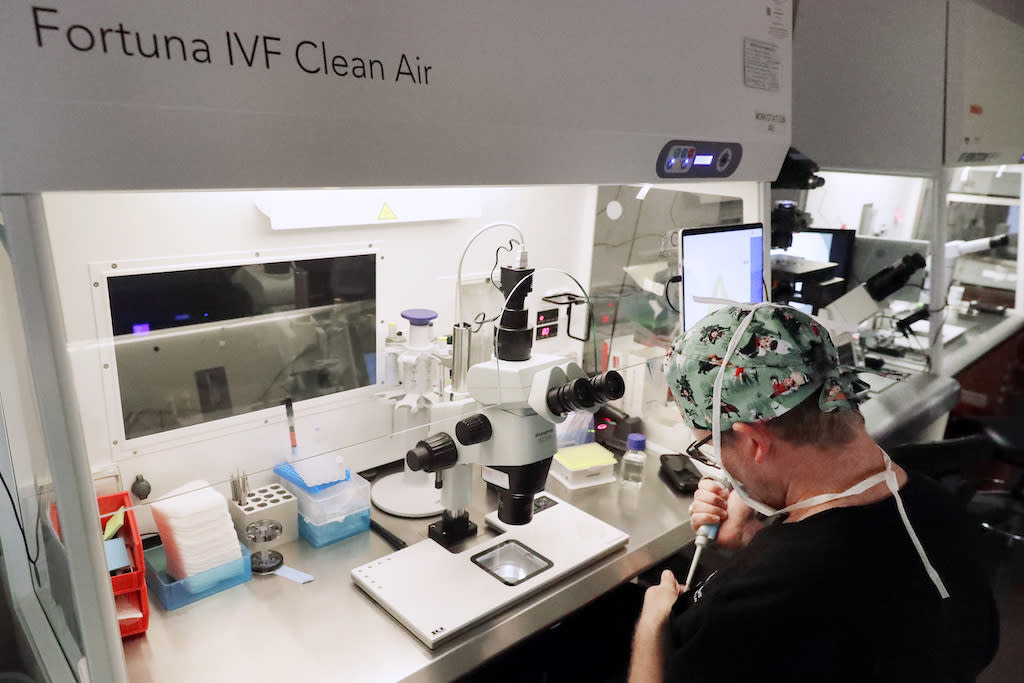
Lab staff prepare small petri dishes, each holding several 1- to 7-day-old embryos, so cells can be tested for viability at the Aspire Houston Fertility Institute in vitro fertilization lab in Houston. Only a handful of states require insurers to cover fertility treatments for same-sex couples, but more are considering it. (Michael Wyke/The Associated Press)
This story originally appeared on Stateline.
Elizabeth Bauer was working out at the gym one morning last August when she got a phone call from her fertility nurse. It was a call that Bauer and her wife, Rebecca, had long been waiting for.
Elizabeth dialed in Rebecca so they could listen together: They were pregnant.
The Washington, D.C., couple decided before they got married three years ago that they wanted to have a child. Both wanted to play a biological part in the pregnancy. So, they used a process called reciprocal in vitro fertilization, through which eggs were retrieved from Rebecca and fertilized with donor sperm to create embryos. Then one of the embryos was implanted in Elizabeth’s uterus.
Elizabeth, a 35-year-old elementary school teacher, and Rebecca, a 31-year-old nonprofit consultant, had health insurance, but it wouldn’t cover the roughly $20,000 procedure, so they had to pay out of pocket.
But beginning next year, insurers providing coverage in D.C. will have to pay for IVF for beneficiaries, including same-sex couples, who can’t conceive on their own. Only seven states (Colorado, Delaware, Illinois, Maine, Maryland, New Jersey and New York) have similar mandates. However, a new definition of “infertility” could prompt other states to follow suit.
The American Society for Reproductive Medicine in October expanded the definition of infertility to include all patients who require medical intervention, such as use of donor gametes or embryos, to conceive as a single parent or with a partner. Previously, the organization defined infertility as a condition in which heterosexual couples couldn’t conceive after a year of unprotected intercourse.
The group emphasized the new definition should not “be used to deny or delay treatment to any individual, regardless of relationship status or sexual orientation.”
Rebecca Bauer, left, and her wife, Elizabeth Bauer, who is due to give birth in April, pose for a photo together. The Washington, D.C., couple paid out of pocket for in vitro fertilization, or IVF, last year. (Courtesy of Rebecca Bauer)
Dr. Mark Leondires, a reproductive endocrinologist and founder and medical director at Illume Fertility and Gay Parents To Be, said the new definition could make a huge difference.
“It gives us extra ammunition to say, ‘Listen, everybody who meets the definition of infertility, whether it’s an opposite-sex couple or same-sex couple or single person, who wants to have a child should have access to fertility services,’” he said.
At least four states (California, Connecticut, Massachusetts and Rhode Island) are currently weighing broader IVF coverage mandates that would explicitly include same-sex couples, according to RESOLVE: The National Infertility Association. Bills were introduced but failed to advance in Oregon, Washington and Wisconsin.
A recent policy shift at the federal level also might add to the momentum. Earlier this month, the departments of Defense and Veterans Affairs announced expanded IVF service benefits to patients regardless of marital status, sexual orientation or whether they are using donor eggs or sperm. The new policy follows a lawsuit filed in federal court last year.
“The federal government is the largest employer in the country, so if they’re providing these type of benefits, it definitely adds pressure on other employers and states to do the same,” said Betsy Campbell, RESOLVE’s chief engagement officer.
A total of 21 states have laws mandating that private insurers cover fertility treatments, but only 15 include at least one cycle of IVF in that mandate. Only New York and Illinois provide some fertility coverage for people who are insured through Medicaid, the state-federal program for people with low incomes and disabilities. Neither state covers IVF for Medicaid recipients.
100,000 babies
IVF involves collecting mature eggs from ovaries, using donated sperm to fertilize them in a lab, and then placing one or more of the fertilized eggs, or embryos, in a uterus. One full cycle of IVF can take up to six weeks and can cost between $20,000 and $30,000. Many patients need multiple cycles before getting pregnant.
Nearly 100,000 babies in the U.S. were born in 2021 through IVF and other forms of assisted reproductive technology, such as intrauterine insemination, according to federal data.
IVF continues to garner nationwide attention in the wake of the Alabama Supreme Court’s ruling last month that under state law, frozen IVF embryos are children, meaning patients or IVF facilities can be criminally charged for destroying them. The decision caused an uproar, and three weeks later Alabama Republican Gov. Kay Ivey signed a bill into law that provides criminal and civil immunity for IVF clinicians and patients.
Polly Crozier, director of family advocacy at GLBTQ Legal Advocates & Defenders, or GLAD, described the Alabama decision as “a shock to the system.” But Crozier said the reaction to it sparked a “bipartisan realization that family-building health care is important to so many people.”
Crozier praised the insurance mandates in Colorado, Illinois, Maine and Washington, D.C., for more explicitly including LGBTQ+ people. Maine’s law, for example, states that a fertility patient includes an “individual unable to conceive as an individual or with a partner because the individual or couple does not have the necessary gametes for conception,” and says that health insurers can’t “impose any limitations on coverage for any fertility services based on an enrollee’s use of donor gametes, donor embryos or surrogacy.”
Christine Guarda, financial services representative at the Center for Advanced Reproductive Services at the University of Connecticut School of Medicine, said more same-sex couples are seeking help starting families. One reason, she said, is that more large employers that provide insurance directly to their employees, such as Amazon, are including broad IVF coverage.
‘Elective procedure’?
But some lawmakers are skeptical of expanding the definition of infertility to include same-sex couples. That was evident at a hearing on the Connecticut bill earlier this month, where Republican state Rep. Cara Pavalock-D’Amato noted that “infertility isn’t necessarily elective, but having a baby is.”
“Now, we are changing definitions to cover elective procedures,” Pavalock-D’Amato said. “If we’re changing the definition for this elective procedure, then why not others as well?”
She added: “Infertility, whether you are straight or gay, up to this point has been a requirement. Now, is it through this bill that we are no longer requiring people to be sick? They no longer have to be infertile?”
But proponents of the change argue that extending IVF mandates to cover same-sex couples is a question of fairness.
“I don’t think anybody in the LGBTQ community is asking for more. They’re just asking for the same benefit, and it is discriminatory to say, ‘You don’t get the same benefit as your colleague simply because you have a same-sex partner,’” Leondires said in an interview.
“If you’re paying to the same health care system as the person sitting next to you, then you should have the same benefit,” he said.
If you're paying to the same health care system as the person sitting next to you, then you should have the same benefit.
– Dr. Mark Leondires, reproductive endocrinologist
Elizabeth and Rebecca Bauer, who are busy decorating a nursery and buying baby clothes, recognize that they were fortunate to have the money to pursue IVF even without insurance coverage, and that “there are plenty of people who don’t have the time or the ability.”
“There are so many ways that people who want to build a family might struggle,” Elizabeth said, adding that the previous infertility definition felt like a “pretty impossible barrier” for non-straight couples. “Insurance should make building a family possible for any person or persons who want to.”
Stateline is part of States Newsroom, a nonprofit news network supported by grants and a coalition of donors as a 501c(3) public charity. Stateline maintains editorial independence. Contact Editor Scott S. Greenberger for questions: info@stateline.org. Follow Stateline on Facebook and Twitter.
The post Few states cover fertility treatment for same-sex couples, but that could be changing appeared first on Alabama Reflector.


