Screening Indicators: Gestational Age 16 to 18 Weeks
Brachycephaly. Brachycephaly is described as shortening of the occipitofrontal diameter (front to back of head) of the fetal head. One study found that brachycephaly was associated with 15% of fetuses affected with trisomy 21.[1] Two other antenatal ultrasound studies found no significant increase in the incidence of brachycephaly in fetuses with trisomy 21 when compared with normal fetuses.[1] However, postnatally it is well established that babies with Down syndrome often had signs of brachycephaly in utero.[1]
Mild ventriculomegaly. Enlarged ventricles in the fetal brain may be associated with a higher incidence of chromosomal anomalies. The presence of mild ventriculomegaly should prompt a detailed ultrasound evaluation to define more precisely any structural anomalies and is sufficient reason to consider genetic testing.[1]
Macroglossia and abnormal facies. Flattening of the facial profile and macroglossia (large tongue) are common postnatal findings associated with trisomy 21. Antenatally, these findings are rarely diagnosed unless other features are initially described. Clinically, these findings are not very significant; however, if identified, they may serve as ultrasound markers. One study did identify an increase in the detection of fetal macroglossia with advancing gestational age. Macroglossia may be recognized by the progressive enlargement and/or protrusion of the fetus' tongue as gestation advances. [1]
Nuchal edema. The use of nuchal fold measurement as a screening method for Down syndrome (Fig. 2) has been described extensively in the literature. In 1992, Benacerraf and associates[8] reported the association of soft-tissue thickening of the posterior aspect of the neck with trisomy 21. The nuchal fold was measured from the outer edge of the occipital bone to the skin edge in a modified transverse view of the head, including the brain stem, cerebellum, and the occipital bone. A measurement of 6mm or more was considered abnormal. The main drawback to the use of this measurement is that it is operator- and fetal-position-dependent. After evaluating 1382 pregnancies, Donnenfeld and coworkers[9] concluded that using 5mm or more as a positive nuchal fold thickness would yield an 8% detection rate and a 1.2% false-positive rate, making this a poor screening test for Down syndrome.
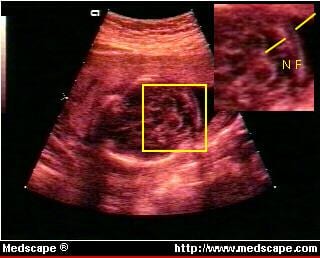
Figure 2. The nuchal fold, seen here in a view through lower portion of fetal head, could indicate a high risk for Down syndrome if thickness is increased. Ultrasound image reproduced with permission from "Nuchal Skin Fold," on the World Wide Web: ( https://www.fetal.com/nf.htm), Copyright © 1997 Greggory DeVore, MD.
Echogenic/hyperechoic bowel. The chance of identifying echogenic or hyperechoic bowel antenatally is calculated to be 1 in 200 mid-trimester fetuses. The bowel is thought to be echogenic when its echogenicity is similar to that of the iliac bones. This finding may be associated with an intra-amniotic hemorrhage, severe uteroplacental insufficiency, cystic fibrosis, and chromosomal defects. In 1994, Bromley and others[10] reported that approximately 12.5% of fetuses with trisomy 21 had echogenic bowel. Dicke and Crane[11] in 1992 and Vintzileos and Egan[12] in 1995 reported the incidence of echogenic bowel to be approximately 1% in infants with Down syndrome compared with 0.2% in infants without Down syndrome.
Pyelectasis. Renal anomalies or deviations from the normal renal anatomy have also been identified as markers for Down syndrome. Corteville and coworkers[13,14] reported that the presence of isolated pyelectasis (enlarged collecting system) prenatally did not warrant amniocentesis for assessment of fetal karyotype. Subsequently, however, Nicolaides and associates[15] reported that the presence of isolated pyelectasis was specifically associated with a 3-fold increase over the maternal age-related risk for chromosomal anomalies. In a 1996 evaluation by Wickstrom and others,[16] the association between isolated pyelectasis and an increased risk for Down syndrome was confirmed in gestational ages between 16 and 20 weeks, beginning at a maternal age of 31 years.
Shortening of the limbs. In 1989, FitzSimmons and colleagues[17] reported an association between shortening of the limbs and Down syndrome. Shortening of the humerus (Fig. 3) in fetuses with Down syndrome has been reported in various prenatal ultrasound studies; however, these studies have produced varying results. The association between shortening of the femur and trisomy 21 has also been made by various authors. In 1985, Benaceraff and others[18] first reported that if the ratio of the actual femur length to the expected length was less than or equal to 0.91, there was a sensitivity of 68% and a specificity of 98% in detecting fetuses with trisomy 21. Other studies have confirmed this association, but have found sensitivities and specificities lower than those originally reported. Still others have disagreed with these findings, suggesting that there is no significant association between shortening of the femur and trisomy 21.[1]

Figure 3. Shortened humerus in a fetus may be associated with high risk for Down syndrome. Ultrasound image reproduced with permission from "Measuring the Arm," on the World Wide Web: ( https://www.fetal.com/arm.htm), Copyright © 1997 Greggory DeVore, MD.
Medscape General Medicine. 1997;1(2) © 1997
Cite this: Identifying Ultrasound Markers for Down Syndrome - Medscape - Jun 13, 1997.




