Cells in the human body chat with each other all the time. One major way they communicate is by releasing tiny spheres called exosomes. These carry fats, proteins, and genetic material that help regulate everything from pregnancy and immune responses to heart health and kidney function.
Now, a new Columbia University study in Nature Nanotechnology demonstrated that these "nanobubbles" can deliver potent immunotherapy directly to tough-to-treat lung cancer tumors via inhalation.
"Exosomes work like text messages between cells , sending and receiving information," said lead researcher Ke Cheng, PhD, professor of biomedical engineering at Columbia. "The significance of this study is that exosomes can bring mRNA-based treatment to lung cancer cells locally, unlike systemic chemotherapy that can have side effects throughout the body. And inhalation is totally noninvasive. You don't need a nurse to use an IV needle to pierce your skin."
Cheng expects a human trial could launch within 5 years. For now, his study is attracting attention because it marks an advance in three areas of intense interest by researchers and biotech companies alike: Therapeutic uses of exosomes, inhalable treatments for lung conditions, and the safe delivery of powerful interleukin-12 (IL-12) immunotherapy.
Inside the Study
Cheng, who has been developing exosome and stem cell therapies for more than 15 years, and his lab team focused on lung cancer because the disease, often detected in later stages, "has a huge mortality rate," he said. "Therapies have been suboptimal and leave the organ so damaged."
He wanted to explore new alternatives to systemic treatments. Most are given intravenously, but Cheng thinks exosomes — also called extracellular vesicles (EVs) — could change that.
"One of the advantages of exosomes is that they are naturally secreted by the body or cultured cells," he noted. "They have low toxicity and have multiple ways of getting their message into cells."
The scientists borrowed an approach that captured public attention during the pandemic: Using messenger RNA, which directs cells to make proteins for tasks — including boosting immune response.
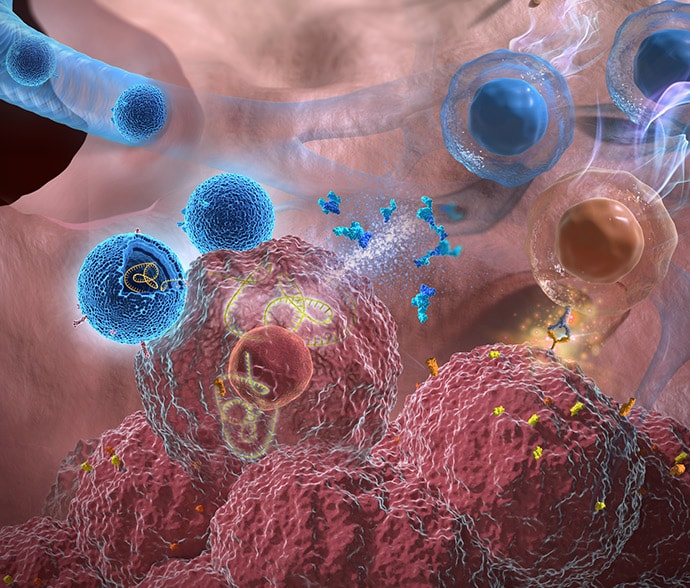
IL-12 has shown promise against cancer for decades, but early human trials triggered serious side effects and several deaths. Researchers are now trying new delivery methods that target tumor cells without affecting healthy tissue. Cheng's team took a new approach, inserting mRNA for IL-12 into exosomes.
One aim of the study was to compare the effectiveness of inhaled exosomes vs inhaled liposomes, engineered fat droplets also under investigation as drug carriers. The team's question: Which would work better at introducing IL-12 to the lungs to affect cancer, without triggering side effects?
After lab mice inhaled the particles through the nose, the researchers found that exosomes delivered more mRNA into cancer cells in the lungs and fought lung cancer with few side effects. Three days after treatment, researchers saw an influx of cancer-fighting T cells within tumors — with higher levels for exosome-based treatment. Plus, the exosomes led to more cancer-destroying nature killer cells and more monocytes, a sign of immune-system activation.
Researchers also found the treatment acted as a vaccine, training the immune system to battle newly introduced cancers. Little of the exosome-delivered drug escaped into the bloodstream, and the study found minimal side effects. Inhalation didn't affect normal breathing, Cheng added.
The study's use of inhaled exosomes makes it significant, said Raghu Kalluri, MD, PhD, professor and chair of the Department of Cancer Biology at MD Anderson Cancer Center. "This is an interesting study that explores the inhalable delivery of engineered EVs for the treatment of lung cancer and offers insights into focused delivery of EV-based drugs…with implications for diseases beyond cancer," he said. Kalluri is also an exosome researcher.
New Frontiers
Once seen as a "quirky biological phenomenon" or just cellular trash, exosomes are now the subject of intense medical research for their potential as drug carriers, as treatments in their own right for everything from wound healing and pneumonia to heart attacks and bowel disorders, and as measurable biological markers that could lead to new tests for cancer and other conditions. One exosome-based prostate cancer test, the ExoDx Prostate Test, is already on the market.
The explosion in exosome research — the number of published studies has grown from just a handful in the early 1980s to more than 9000 — spotlights a particular focus on cancer. According to a 2021 paper in Annals of Oncology, clinical trials for exosomes in cancer treatments and tests far out-paces those for diabetes, heart disease, or neurologic conditions. Currently, 52 clinical trials using exosomes in cancer diagnosis or treatment have been completed, are underway, or are looking for participants, according to clinicaltrials.gov.
Cheng's approach could also be used to deliver other drugs to the lungs and other organs via inhalation. "We're testing inhalation for a different type of lung disease, acute lung injury," Cheng said. Other potential targets include lung disorders like pulmonary hypertension. Inhaled exosomes could potentially reach the brain via the olfactory bulb or the heart as it receives oxygenated blood from the lungs.
Breathing in Medicine
So far, inhalable cancer treatments are not available outside research studies in the United States or Europe , said Remi Rosiere, PhD, a lecturer at the Université libre de Bruxelles in Brussels, Belgium, and chief scientific officer of InhaTarget Therapeutics, a company developing its own inhaled treatments for severe respiratory diseases. "Oncologists are very interested," he said. "If you concentrate the drug on the tumor site, you can avoid distribution to the body."
Early research into inhalable chemotherapy began in the 1960s but was unsuccessful because breathing equipment dispersed toxic cancer drugs into the air or delivered only small amounts to the lungs, he said.
New delivery techniques aim to change that. Rosiere's company is starting a human trial of a dry powder inhaler with the chemotherapy drug cisplatin for lung cancer. Also in the pipeline is an immunotherapy treatment for lung cancer inserted in lipid nanoparticles, which are tiny fat particles similar to liposomes.
He said Cheng's study shows the advantages of sending in exosomes. "The data are very persuasive," Rosier said of the study. "Exosomes have a good safety profile and are able to remain in the lung for quite a long time. This prolongs exposure to the drug for greater effectiveness, without causing toxicities."
Getting from a mouse study to a human trial will take time. "You need to understand this is very early stage," Rosiere added. "There will be many challenges to overcome."
One is purely practical: If the drug approaches human trials, he said, regulators will ask whether the exosomes can be produced in large quantities to meet the huge demand for new lung cancer treatments. "Lung cancer is the number one fatal cancer in the world," Rosiere said.
A New Route for 'Powerful' Cancer Treatment
Meanwhile, the Columbia University study showed that inhalable exosomes are a unique delivery method for IL-12 — and could help solve a major problem that's plagued this promising cancer treatment for decades.
Called "one of the most powerful immunotherapy agents ever discovered" in a 2022 literature review, IL-12 showed serious side effects that stalled research in the 1980s , sparking an ongoing search for new delivery methods that continues today. In 2022 and 2023, Big Pharma companies including AstraZenca, Moderna, and Bristol Myers Squib reduced their involvement with IL-12 treatment research, leaving the field open to smaller biotech companies working on a variety of drug-delivery approaches that could make IL-12 safe and effective in humans.
These include injecting it directly into tumors, encasing it in various types of particles, masking the drug so it is activated only in cancer cells, and using IL-12 mRNA, which essentially turns tumor cells into IL-12–producing factories. Another IL-12 mRNA drug, from Pittsburgh-based Krystal Biotech, received a fast-track designation from the US Food and Drug Administration in February 2024 for an inhaled lung cancer treatment that packages mRNA for IL-12 and IL-2 inside an engineered virus.
And of course, there is Cheng's inhalable treatment, culminating decades of work across three burgeoning fields.

