Current Treatments
Currently, there is no treatment available that effectively prevents visual loss or improves vision in all patients with CNV and ARMD. However, randomized clinical trials have demonstrated the value of laser photocoagulation and photodynamic therapy (PDT) with verteporfin in selected patients. In addition, new treatment modalities are currently under investigation.
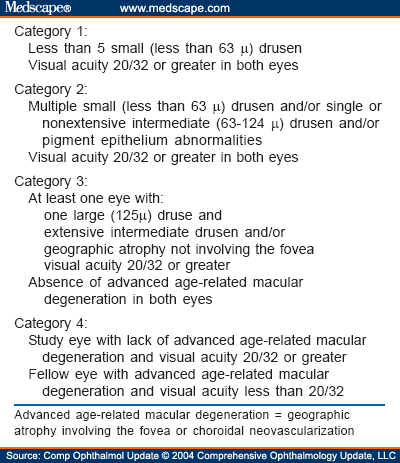
Before deciding which modality of treatment is appropriate for each patient, it is important to recognize the location and fluorescein angiographic characteristics of the CNV (Figures 1 and 2). These have been summarized in Table 1 .
Top: Early phases of the fluorescein angiogram in patients with extrafoveal (left), juxtafoveal (center), and subfoveal (right) classic choroidal neovascularization. Bottom: Late phases of the fluorescein angiogram in patients with extrafoveal (left), juxtafoveal (center), and subfoveal (right) classic choroidal neovascularization.
Top: Early phases of the fluorescein angiogram in patients with predominantly classic (left), minimally classic (center), and occult (right) choroidal neovascularization. Bottom: Late phases of the fluorescein angiogram in patients with predominantly classic (left), minimally classic (center), and occult (right) choroidal neovascularization.
The Macular Photocoagulation Study (MPS) demonstrated the value of laser photocoagulation in patients with ARMD and extrafoveal CNV (Figure 3).[17,18,19] In this study, patients with well defined extrafoveal CNV were treated with argon blue-green laser. After a follow-up of 5 years, 64% of eyes assigned to no treatment compared with 46% of eyes randomized to argon laser experienced severe visual loss (six or more lines of visual acuity loss using Bailey-Lovie visual acuity charts). The difference was statistically significant. Although the risk of severe visual loss was reduced in treated patients, a high rate of persistent and recurrent CNV was observed.[20] The recurrence rate observed in treated eyes at 6, 12, 24, 36, and 60 months was of 24%, 41%, 50%, 51%, and 54%, respectively (Figure 3).
Top left: Late phase of the fluorescein angiogram in a patient with extafoveal classic choroidal neovascularization. Top right: The choroidal neovascularization was ablated using laser photocoagulation. Bottom left: Recurrence of the choroidal neovascularization was observed soon after treatment. Bottom right: Further laser treatment was applied. Two years following laser photocoagulation no new recurrences have been detected and visual acuity remains 20/20.
The MPS also showed the benefit of treating patients with juxtafoveal CNV and no systemic hypertension with laser photocoagulation.[21] In this study, patients with well defined juxtafoveal CNV were treated with krypton red laser. At 3 years after randomization, 49% of laser-treated eyes experienced severe visual loss compared with 58% of untreated eyes. Although a statistically significant benefit was observed in patients with no evidence of systemic hypertension, this was not the case in hypertensive patients, in whom no statistically significant benefit was observed following laser treatment. In this study, 32% of treated eyes had persistent CNV leakage detected within 6 weeks of initial treatment and recurrent CNV developed in an additional 47% of treated eyes over a 5-year period.[22] The treatment benefit observed in patients with laser-treated juxtafoveal CNV and no systemic hypertension was maintained at 5 years.[23]
Two other MPS trials demonstrated the value of laser photocoagulation in the treatment of patients with ARMD and new or recurrent subfoveal CNV.[24,25] In the new subfoveal CNV study, patients with subfoveal CNV were treated with either krypton red or argon green laser. In addition to classic CNV, the lesion could be formed by occult CNV, blood, and areas of blocked fluorescence corresponding to scar tissue, pigment, or a serous detachment of the RPE. Although at 3 months following treatment 20% of laser-treated eyes and 11% of observed eyes had experienced severe visual loss, at 24 months only 20% of laser-treated eyes compared with 37% of untreated eyes had this outcome. The difference was statistically significant. At 4 years this treatment benefit was still maintained.[26] Laser-treated eyes experienced an average of three line visual acuity loss 3 months following treatment. The largest treatment benefit was observed in eyes with low levels of visual acuity (less than 20/125) and small lesions (two or fewer MPS disk areas).[27]
In the recurrent subfoveal CNV study, patients who had undergone laser treatment for extrafoveal or juxtafoveal CNV and later developed a subfoveal recurrence were treated with krypton red or argon green laser. At 24 months after treatment only 9% of laser-treated eyes had experienced severe visual loss compared with 28% of untreated eyes. The difference was statistically significant. At 3 years, this treatment benefit was still maintained.[26] Three months following treatment, laser-treated eyes experienced an average of 2.4 lines of visual loss.
In both subfoveal studies (new and recurrent CNV) persistent CNV was observed in 13% of eyes, and recurrent CNV was detected in 35% of eyes 3 years following treatment.[28]
It should be noted that the interpretation of fluorescein angiography during the initial years of the MPS was incomplete. It was not until the beginning of 1989 that the characteristics of the lesions on fluorescein angiography, as we know now, were introduced. The fact that differentiation between classic and occult CNV and the recognition of the lesion components was not established until later on in the course of macular photocoagulation trials may have had some repercussion in the results observed.[29]
A different technique for laser photocoagulation of subfoveal CNV was proposed by Coscas and colleagues.[30] With this technique, laser photocoagulation was applied over the subfoveal CNV, avoiding the central foveal avascular zone. In a randomized controlled clinical trial a statistically significant benefit with regard to avoiding visual loss and maintaining reading vision with the aid of magnifiers was observed in patients treated with this perifoveal laser photocoagulation compared to those observed with no treatment.[31]
Photodynamic therapy (PDT) involves the intravenous infusion of a light-activated drug (photosensitizer) and the application of a continuous nonthermal laser light directed at the CNV. The wavelength of the laser light used corresponds to the absorption peak of the drug, but it is not strong enough to produce any thermal (photocoagulation) damage. Although the mechanism of action is not completely understood, it is believed that the excited photosensitizer generates singlet oxygen and free radicals that cause cellular damage. Since the photosensitizer accumulates predominantly in the CNV, a fairly selective damage to the CNV is expected. To date, only PDT with the photosensitizer verteporfin has been proven to decrease the risk of visual loss in patients with neovascular ARMD. Thus, this section will be limited to this form of therapy.
A large prospective, randomized, multicenter, placebo-controlled, double-masked clinical trial showed that PDT with verteporfin reduced the risk of moderate (loss of 15 ETDRS letters or three lines) and severe (loss of 30 ETDRS letters or six lines) visual loss in patients with ARMD and subfoveal CNV (Figures 4 and 5).[32,33] Only patients with subfoveal CNV and evidence of some classic CNV were eligible for the trial. Photodynamic therapy was performed using a diode laser (689 nm) connected to a slit-lamp. The treatment was done as follows. First, the intravenous infusion of placebo/verteporfin was given throughout a 10-minute period. Then, 15 minutes after the start of the infusion the laser light was applied for 83 seconds. Patients were followed every 3 months and retreatment was performed if fluorescein leakage from CNV was noted.
Early (top, left) and late (top, center) phases of the fluorescein angiogram in a patient with subfoveal classic choroidal neovascularization. After one (top, right), two (bottom, left), and three (bottom, center) sessions of photodynamic therapy the area of leakage from choroidal neovascularization decreased in size, although some activity of the choroidal neovascularization was still present after the third photodynamic therapy session (bottom, right).
Early (top, left) and late (top, center) phases of the fluorescein angiogram in a patient with subfoveal classic choroidal neovascularization. Following one session of photodynamic therapy (top, right and bottom, left) the lesion appeared to have increased in size. After three photodynamic therapy sessions (bottom, center and right) no active leakage from choroidal neovascularization was observed and only staining of the fibrovascular scar was present.
Using Kaplan-Meier survival curves it was found that at 2 years, 53% of patients that received PDT had experienced moderate visual loss compared with 68% of patients in the placebo group.[33] The greatest treatment benefit was seen in those patients with predominantly classic CNV. When data from the latter patients were analyzed, it was observed that at 2 years, 59% of patients treated with PDT had visual loss of three or fewer lines compared with only 31% of patients receiving placebo (Visudyne, product monograph, Novartis Ophthalmics, 2001, pp 41-54) No treatment benefit was detected, however, in patients with minimally classic CNV. The mean number of PDT treatments required during the first year was three and during the second year, the mean number was two treatments.
Although patients with occult-only CNV were not eligible, 9% of eyes evaluated in the above trial had this type of CNV. The number of patients in this group was too small to draw any significant conclusion, but a treatment benefit appeared to be apparent in these patients. For that reason, patients with occult CNV were enrolled in a prospective, randomized, multicenter, placebo-controlled, double-masked clinical trial.[34] In this trial, no statistically significant benefit of PDT was observed at 12 months. However, a statistically significant treatment benefit was apparent at 24 months, with moderate visual loss occurring in 55% of treated patients compared with 68% of those randomized to placebo. The greatest benefit was achieved in patients with either smaller lesions (four or fewer disk areas) or lower levels of visual acuity (letter score of less than 65 ETDRS letters, an approximate Snellen equivalent of 20/50 or less). The mean number of PDT treatments required during the first year was three and during the second year it was two.
Complications related to PDT are infrequent, and include photo-sensitivity reactions; injection-site adverse events; infusion-related back, chest, and leg pain; and visual disturbances. Severe visual loss within 7 days of PDT has been also described in 4% of patients with occult CNV.[34]
Guidelines for the treatment of patients with ARMD and subfoveal CNV with PDT have been recently published.[35] In these guidelines, treatment with PDT is recommended for patients with predominantly classic CNV and for those with occult and no classic CNV with recent disease progression (e.g., presence of blood associated with the CNV, growth of the CNV, or deterioration of the visual acuity within the past 12 weeks) and a lesion size of four or fewer disk areas or a lesion size greater than four disk areas associated with low levels of vision (i.e., approximately in the level of 20/50 Snellen vision). In these guidelines, it is also recommended to treat juxtafoveal lesions that are so close to the fovea that conventional laser photocoagulation almost certainly would extend under the center of the foveal avascular zone, and subfoveal lesions that are contiguous to the optic nerve provided that treatment spots do not overlie the optic nerve. The recommendations included a 3-month interval follow-up for at least 2 years from the time of initial treatment in all patients, except in those in whom no treatment was recommended for two consecutive visits (6-month period) who could be followed at 6- and eventually 12-month intervals. Patients should receive retreatments as often as every 3 months if there is any fluorescein leakage from CNV noted. In cases in which the entire area of the lesion cannot be covered by the largest treatment spot available and the visual acuity is poor or if visual acuity remains stable or has improved, the biomicroscopic and angiographic appearance of the lesion remains unchanged or improved, there is minimal fluorescein leakage from CNV (less than 50% of the area treated at the previous visit) without progression of fluorescein leakage beyond the boundaries of the area treated at previous visit, the lesion is flat (scar-like appearance), and there is minimal or no subretinal fluid on clinical examination, retreatment could be then deferred for another 3 months. The guidelines also state that if well defined extrafoveal fluorescein leakage from CNV is present at one of the follow-up visits, treatment with conventional laser photo-coagulation could be then performed. Although no data are currently available on the treatment of pregnant or nursing women and patients with moderate or severe liver disease, the guidelines suggest to carefully consider PDT in these patients. Photodynamic therapy is contraindicated in patients with porphyria.
Although not specified in the above guidelines, it seems reasonable to consider PDT in hypertensive patients with juxtafoveal CNV, in whom the MPS failed to show a significant benefit of laser treatment.
Compr Ophthalmol Update. 2004;5(3) © 2004 Comprehensive Ophthalmology Update, LLC
Cite this: Neovascular Age-Related Macular Degeneration - Medscape - May 01, 2004.