Corticosteroids
Corticosteroids, or glucocorticosteroids, exhibit a wide range of effects on almost every phase of the immune and inflammatory responses in animals and humans. These agents, in pharmacologic doses, play a major role in the treatment of many diseases.[22,23] For more than 4 decades, the extraordinary ability of corticosteroids to prevent or suppress inflammation, whether the insulting agent is infectious, immunologic, or mechanical, has been studied and documented. Corticosteroids include the primary endogenous glucocorticoid, cortisol, and exogenous therapeutic agents such as prednisone and methylprednisolone. The anti-inflammatory effects of exogenous corticosteroids are similar to those of endogenous glucocorticoid.
Mechanism of Action
Used clinically since the 1920s, corticosteroids interrupt multiple steps in immune activation because of the ubiquitous expression of corticosteroid receptors. Corticosteroids inhibit antigen presentation, cytokine production, and proliferation of lymphocytes.
Corticosteroids have a profound effect on the concentration of peripheral blood leukocytes. Lymphocyte, monocyte, and basophil counts decrease in response to corticosteroid administration, while neutrophil counts increase. The peak effects are seen within 4 to 6 hours after a dose of corticosteroid. It is believed that corticosteroids induce their effects on the cell through a glucocorticoid receptor in the cytoplasm.[24] On contact with the receptor, the steroid-receptor complex translocates into the nucleus of the cell, where it attaches to DNA and causes transcription of specific messenger RNA, which produces synthesis of proteins that mediate glucocorticoid activity.
The lymphocyte effect. A single dose of corticosteroid produces lymphocytopenia within 4 hours. The peripheral lymphocyte count returns to normal within 24 to 48 hours. [25] Corticosteroid-induced lymphocytopenia occurs as a result of redistribution of circulating lymphocytes into other lymphoid compartments (eg, spleen, lymph nodes, thoracic duct, and bone marrow).[26,27] The recirculating lymphocyte pool, which accounts for approximately two thirds of the total lymphocyte pool, consists mainly of T lymphocytes (T cells) that migrate to and from the intravascular compartment and lymphoid tissue. Non-recirculating lymphocytes, which include some T cells and many B lymphocytes (B cells), live out their life span in the vascular compartment.
The monocyte effect. Monocytes/macrophages (promonocytes in the bone marrow, circulating monocytes, tissue macrophages) play a major role in the induction and regulation of immune reactivity. Macrophages are intricately involved in the presentation of antigens to lymphocytes and in the subsequent removal of immune complexes. Therefore, pharmacologic manipulation of these cells may directly and indirectly impair the immune response in general.
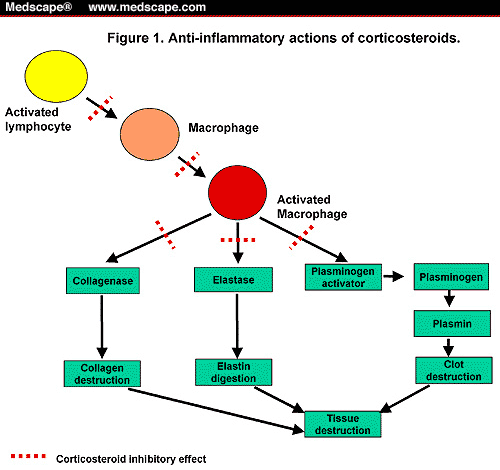
Corticosteroids cause a profound depletion of monocytes; cell counts drop from 300 to 400 cells/mm3 to < 50 cells/mm3. Corticosteroid-induced monocytopenia also appears to be related to the redistribution phenomenon[28] and inhibits inflammation by blocking responses to chemotactic factors and macrophage activation factor, phagocytosis, pyrogen production, and secretion of collagenase, elastase, and plasminogen activator.[29] Figure 1 illustrates corticosteroid inhibition of tissue destruction associated with inflammation.
Figure 1.
Anti-inflammatory actions of corticosteroids.
The neutrophil effect. Corticosteroids cause neutrophilia, manifested by an increase in the neutrophil count by 2000 to 5000 cells/mm3. This in turn, causes an accelerated release of neutrophils from the bone marrow into the circulation and a reduction in the migration of neutrophils out of the circulation. Corticosteroids also inhibit the ability of neutrophils to adhere to vessel walls, which is an essential step in the migration of cells from the circulation into the tissue. The net effect is a reduced number of neutrophils available to accumulate at the inflammatory site.
The eosinophil effect. Corticosteroids cause profound eosinophilia, manifested by a decrease in the eosinophil count to < 25 cells/mm3. Corticosteroid-induced eosinophilia is also caused by the redistribution phenomenon. Chemotaxis is also affected and may result from the inhibition of responses to chemotactic factors.
Other effects of corticosteroids. Corticosteroids have a negative effect on prostaglandin, probably as a result of reduction in the fatty acid precursors necessary for prostaglandin production. Corticosteroids also block production of IL-1, which normally stimulates prostaglandin production.[30] Another effect of corticosteroids is complete inhibition of T-cell growth factor or IL-2. IL-2 is produced by activated T cells and promotes proliferation of other T cells. Therefore, T cells under the influence of corticosteroids lose their ability to proliferate and react to specific antigens.[31,32] Antibody production is not commonly suppressed at conventional doses in humans; however, high doses of corticosteroids given for long periods of time may lead to a decrease in antibody formation, particularly IgG.
Pharmacokinetic Profile
Refer to product insert from the manufacturer for specific information on the pharmacokinetic parameters of corticosteroid preparations.
Therapeutic Uses
In physiologic doses, corticosteroids are used to replace deficient endogenous hormones. In pharmacologic doses, corticosteroids have both therapeutic and diagnostic applications. Corticosteroids are used in pharmacologic doses for their anti-inflammatory and immunosuppressive properties. When corticosteroids are used for these purposes, the systemic agents with the least mineralocorticoid activity (sodium and water retention) should be used. Table 2 provides the anti-inflammatory potency, equivalent dosage, and relative mineralocorticoid activity of commonly used corticosteroids.
Circulating lymphocytes play a major role in the initiation and persistence of immunologic disease. They perform functions such as antigen recognition and memory cell recruitment, direct cytotoxicity, production of lymphotoxins and other cytotoxic factors, and release of various immune mediators.[33] Sensitized lymphocytes are kept out of the peripheral circulation by corticosteroids, thus inhibiting the access of lymphocytes to target organs. Also, the effects of corticosteroids on circulating monocytes and monocyte-macrophage functions are important in the mechanism of immunosuppression. Figure 2 illustrates the anti-inflammatory and immunosuppressive effects of corticosteroids.
Anti-inflammatory and immunosuppressive effects of corticosteroids.
Corticosteroids
Corticosteroids, or glucocorticosteroids, exhibit a wide range of effects on almost every phase of the immune and inflammatory responses in animals and humans. These agents, in pharmacologic doses, play a major role in the treatment of many diseases.[22,23] For more than 4 decades, the extraordinary ability of corticosteroids to prevent or suppress inflammation, whether the insulting agent is infectious, immunologic, or mechanical, has been studied and documented. Corticosteroids include the primary endogenous glucocorticoid, cortisol, and exogenous therapeutic agents such as prednisone and methylprednisolone. The anti-inflammatory effects of exogenous corticosteroids are similar to those of endogenous glucocorticoid.
Administration and Dosage
Corticosteroids may be administered orally, by oral inhalation, and by parenteral routes (IV, IM, subcutaneously, and intra-articularly). Corticosteroids used for immunosuppression in transplantation are administered orally or parenterally. Because injections of slightly soluble corticosteroids may produce atrophy at the site of injection, IM injections should be administered deeply into gluteal muscle, and repeated injections at the same site should be avoided.
Dose ranges for corticosteroids vary with the disease or condition for which they are being prescribed. Types of dosing regimens used in various disease states include physiologic or replacement therapy (doses equivalent to the amount of corticosteroid normally secreted by the adrenal cortex per day) or pharmacologic therapy (any dose greater than physiologic dose). Pharmacologic prednisone therapy may be divided into several categories: (1) maintenance or low-dose: dosages slightly greater than physiologic (eg, 5-15 mg/day), (2) moderate-dose: approximately 0.5 mg/kg/day, (3) high-dose: approximately 1-3 mg/kg/day, and (4) massive-dose: approximately 15 to 30 mg/kg/day. Typically, pharmacologic doses of corticosteroids are used in immunosuppressive regimens. The approximate dosage equivalents of the commonly used corticosteroids are shown in Table 2 .
Long-term corticosteroid therapy should not be initiated without first considering the risks of therapy. Some basic principles for corticosteroid therapy include, if possible: (1) maintaining the patient on an alternate-day (every-other-day) dosing schedule (usually 2 1/2 to 3 times the minimum daily dose), (2) use of short-acting oral corticosteroids (prednisone is prescribed most often because it is inexpensive and has a short serum half-life), (3) administer in the morning to maintain the normal circadian cycle of morning peaks and evening troughs, and (4) administer the minimum dosage to produce the desired response.
Adverse Effects
The side effects of corticosteroids are not specific to lymphocytes and a number of serious adverse events are associated with the prolonged use. Complications of corticosteroid therapy are numerous and virtually any organ system in the body may be affected. It should be emphasized that when corticosteroids are used appropriately and judiciously, complications can be minimized. Short-term or acute adverse effects, which usually occur with initiation of therapy, include central nervous system (CNS) effects, psychosis, pseudotumor cerebri, impaired glucose tolerance, and retention of salt and fluid. CNS effects may range from euphoria to depression, probably as a result of increased brain excitability. Insomnia, jitteriness, and increased appetite are common. These CNS effects usually subside when the dose is decreased. Fluid and salt retention may exacerbate congestive heart disease; however, dietary restrictions may decrease fluid retention. Glucose intolerance may lead to steroid-induced diabetes mellitus (DM) or may aggravate preexisting DM.
Long-term adverse effects of corticosteroid therapy are insidious in onset and tend to subside more slowly when therapy is discontinued. These adverse effects are most likely to occur in patients who take corticosteroids daily for months or longer, such as the development of iatrogenic Cushing's syndrome with truncal obesity and "buffalo hump" associated with long-term corticosteroid use. Other effects of long-term corticosteroid use include acne, striae, and hirsutism. Growth retardation has also been shown to occur in pre-pubertal children. This phenomenon was a major limitation in pediatric transplantation before the introduction of CsA therapy. Adjustment to alternate-day therapy at the lowest possible dose or withdrawal of corticosteroids altogether may help to reduce or reverse these complications.
One of the most common side effects of corticosteroid therapy is cataract formation. Glaucoma may be induced or aggravated by corticosteroid ophthalmic preparations.
Osteoporosis is a particularly troublesome complication of prolonged corticosteroid therapy. Loss of bone matrix and bone mineral is caused by direct inhibition of bone formation and indirect stimulation of bone resorption, resulting from inhibition of calcium absorption from the intestine. The resultant bone thinning can lead to spontaneous vertebral compression and bone fractures.
High doses of corticosteroids for more than 2 weeks at a time may predispose patients to opportunistic infections (ie, Aspergillus species, Pneumocystis carinii, and Herpesvirus species).
Several drug interactions with corticosteroids may be of clinical importance. Drugs that induce liver enzyme systems, such as barbiturates, phenytoin, and rifampin, increase the metabolism of corticosteroids. Estrogens increase the effects of corticosteroids as a result of an increase in available transcortin, thereby decreasing the amount of corticosteroid available for metabolism. Potassium-wasting diuretics, such as furosemide and the thiazides, and other drugs that waste potassium, such as amphotericin B, may enhance the potassium-wasting effect of corticosteroids. Corticosteroids in combination with anticholinesterase agents may produce a pronounced muscle weakness.
Abrupt withdrawal of corticosteroids is dangerous. When corticosteroids are rapidly tapered, patients may exhibit withdrawal symptoms such as headaches, myalgias, and fatigue. These symptoms reflect mild adrenocortical insufficiency and are usually transient. They may be prevented or lessened by a more gradual tapering of corticosteroids. The abrupt withdrawal of high-dose corticosteroids may also cause cardiovascular collapse, resulting in hypotension and shock. Table 3 summarizes the side effects and nursing implications of corticosteroid therapy.
Because of their adverse events profile, corticosteroids have become persona non grata in immunosuppressive regimens. Over the past 20 years, an impressive body of research has been devoted to withdrawing or avoiding corticosteroids in immunosuppressive regimens. While conflicting results have prevented clinical consensus, the difference between corticosteroid withdrawal and corticosteroid avoidance is being acknowledged. Withdrawal of corticosteroids can trigger late acute rejection episodes, thought to be more harmful than early episodes. Corticosteroid avoidance is now being studied in earnest, using newer immunosuppressive agents to compensate for the lost efficacy of corticosteroids.
Organ Transplant © 2002 Medscape
Cite this: Susan L. Smith. Immunosuppressive Therapies in Organ Transplantation - Medscape - Jun 01, 2002.






Comments