Abstract and Introduction
Abstract
Spinal cord compression (SCC) occurs in 5% to 30% of the oncology population and affects patient function, comfort, and general quality of life. Patients with lung cancer, breast cancer, prostate cancer, cancer with an unknown primary site, or renal cancer are at high risk for the development of SCC by metastatic tumor. Spinal cord compression can also occur in sarcoma, myeloma, leukemia, thyroid cancer, lymphoma, melanoma, and gastrointestinal malignancies. Favorable response to treatment directly correlates with early recognition of the signs and symptoms of SCC. Treatment includes administration of corticosteroids, radiation therapy, surgery, and chemotherapy. Nurses should watch for early symptoms (particularly pain), obtain a thorough history, perform a complete physical examination, and teach the patient and his or her family about signs and symptoms of SCC that need to be reported as soon as they occur.
Introduction
Compression of the spinal cord and nerve roots is the second most frequent neurologic complication of cancer (brain metastases are the most frequent neurologic complication).[1] Each year in the United States, approximately 20,000 persons with cancer develop SCC; this group represents 5% to 10% of the general cancer population.[2,3] Because of improved treatments and prolonged survival in various cancers, the incidence of SCC may be increasing.[4]
Cancers most likely to spread to the spine are lung, breast, and prostate cancer; kidney cancer and lymphoma tend to spread to the spinal cord as well.[1,5,6] Patients with melanoma, renal cell carcinoma, multiple myeloma, or certain sarcomas are also at risk for SCC.[1,3] Sarcomas and neuroblastoma cause more than 80% of cases of metastatic SCC in children.[2]
Malignant SCC is defined as compressive indentation, displacement, or encasement of the spinal cord's thecal sac by metastatic or locally advanced cancer.[1] Spinal cord compression produces edema, inflammation, and mechanical compression, which causes direct neural injury to the cord, as well as vascular damage and impairment of oxygenation.[6]
Malignancies of the breast, prostate, lung, and kidney have a propensity to metastasize to bony structures, but any invasive cancer capable of hematogenous spread can produce SCC. Cancers that spread to the spine move to the bone marrow of the vertebral column by way of blood vessels. Spinal cord compression can also occur through direct tumor extension, which is frequently seen in non-Hodgkin's lymphoma. In such cases, there is direct extension of a paraspinal mass through the epidural foramen, and this extension produces the compression. Finally, metastasis results when tumor cells in the cerebrospinal fluid deposit tumor cells in the epidural space.This scenario most often occurs in leukemia.[2]
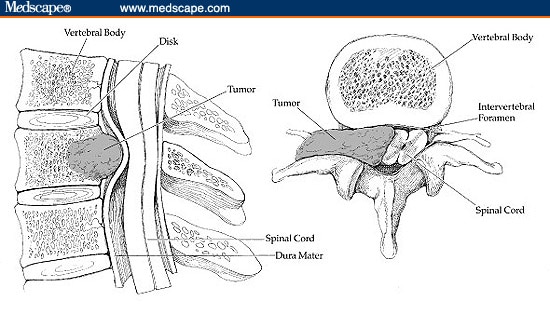
Spinal cord compression results when a metastatic tumor grows into the epidural space and impinges on the dura (the tough membrane that covers the spinal cord), thereby producing pressure on neurologic tissue. As the mass grows, it destroys the bony structure of the vertebrae and weakens them to the point of collapse. The spinal column may then become weak and destabilized.[1,2] (See Figure.)
Figure 1.
Spinal cord compression.
Spinal cord compression constitutes a true emergency because the initial injury to the spinal cord will lead to permanent loss of neurologic function if the pressure of the tumor on the cord is not relieved quickly. Prognosis depends greatly on the length of time of the cord impingement, the location of the mass in the spinal column, and the tissue type of the mass.
Prognosis of SCC also depends on the functional status and length of survival after treatment. Spinal cord compression is fatal only if it occurs in the cervical region of the spinal cord (C4 and above) and if it results in respiratory paralysis that is uncompensated by mechanical ventilation.[7] Tumor tissue type must be considered when the treatment plan is being determined. Some tumors, such as Hodgkin's lymphoma and small cell lung cancer, are very sensitive to chemotherapeutic agents, whereas lymphoma and myeloma are more radiosensitive, and breast and prostate cancers may respond to hormonal agents.[2,4,8]
Advanced practice nurses (APNs) such as nurse practitioners, clinical nurse specialists, and independent hospice and home care nurses are often the first members of the health care team to see the patient and detect the signs and symptoms of SCC. Advanced practice nurses may encounter SCC in any practice serving patients with a cancer diagnosis. An APN may see patients with SCC in an ambulatory clinic, the emergency department of a community or rural hospital, or the primary care setting. However, an APN is more likely to encounter patients with this complication in the acute care setting, particularly in an acute care hospital that specializes in oncology. The APN must be able to recognize the often subtle signs of SCC so that a diagnostic work-up and subsequent treatment can be started as quickly as possible -- ideally, within 24 hours of presentation of signs or symptoms.
Topics in Advanced Practice Nursing eJournal. 2002;2(4) © 2002 Medscape
Cite this: Spinal Cord Compression: An Obstructive Oncologic Emergency - Medscape - Oct 10, 2002.