Diagnosis
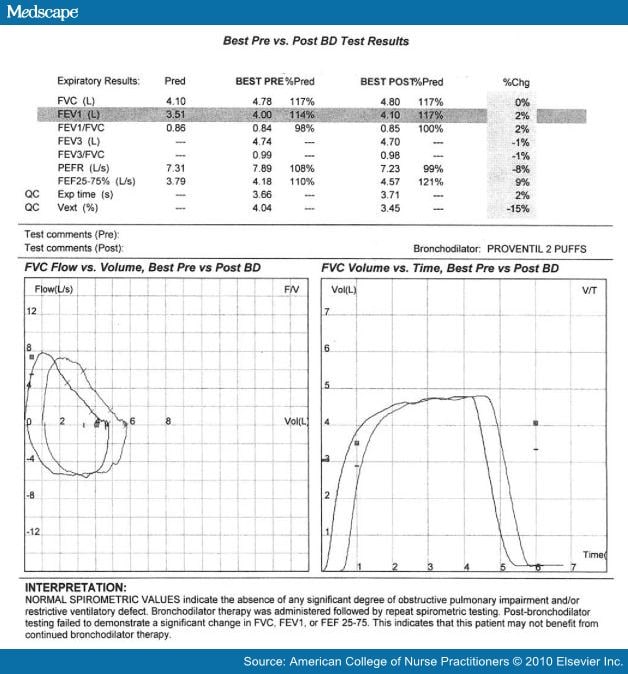
Complicating an often difficult diagnosis is the presence of asthma; as many as 40% of patients diagnosed with VCD also have asthma.[4] Diagnosis of VCD begins with a careful history, including signs and symptoms, triggers, physical exam, and spirometry testing before and after bronchodilator.[4] Patients with VCD often demonstrate a truncated or flattened inspiratory flow loop with an otherwise normal test.[7,8] After bronchodilator, patients who have VCD will not demonstrate significant reversibility (forced expiratory volume in one second [FEV1] improvement of $ 12%).[12] Pulmonary function testing with flow volume loop is commonly used to support the diagnosis of this condition but does not provide a definitive diagnosis as abnormal inspiratory flow loops may be the result of poor patient effort.[10,13,14] Figure 1 offers an example of inspiratory flow loop truncation seen with VCD, and Figure 2 illustrates a normal spirometry test.
Figure 1.
Spirometry test results seen with vocal cord dysfunction
Figure 2.
Normal spirometry test results
Methacholine challenge testing and exercise challenge testing may assist in the diagnosis of some patients but can result in a false positive for asthma 22% of the time.[15] Inhaling methacholine may cause severe bronchospasm and coughing, making it difficult to interpret the results in a patient suspected of having VCD.[3,4] During this test, the patient inhales methacholine in increasing concentrations, with spirometry performed before and after each incremental increase. A fall in FEV1 of 20% on the challenge is generally considered diagnostic of asthma, but a positive test may also be seen in patients with a respiratory tract infection (RTI), chronic obstructive pulmonary disease, bronchiectasis, or congestive heart failure.[7]
Exercise challenge testing is also occasionally obtained and is useful in ruling out exercise-induced bronchospasm and may detect VCD induced by exercise.[8] Formal testing is done on a treadmill with before and after spirometry. Vital signs and pulse oximetry are also checked before, during, and after exercise. Patients are advised not to eat or use their bronchodilator before testing and wear appropriate clothing and footwear. Protocols vary but most begin with stretching and 2 minutes of walking; then patients run on the treadmill until they are unable to continue, reach a target heart rate set by the provider, or have a bronchospasm. Spirometry is performed immediately after running and every 5 minutes up to 30 minutes. A bronchodilator is administered at the time of greatest decline to determine response. A positive test is a decrease in FEV1 of 12% or more and subsequent improvement after bronchodilator.
Laryngoscopy is the gold standard in diagnosis of VCD, with a higher degree of accuracy, but is invasive and difficult to obtain when the patient is having symptoms. Flexible fiber optic laryngoscopy, inserted through the nose or mouth after local anesthesia, takes about 10 minutes and may be performed in an ear, nose, and throat (ENT) specialty office. Care must be taken not to anesthetize the vocal cords. Direct laryngoscopy is done in an operating room and is performed if tissue samples are needed or growths need to be removed from the vocal cords.
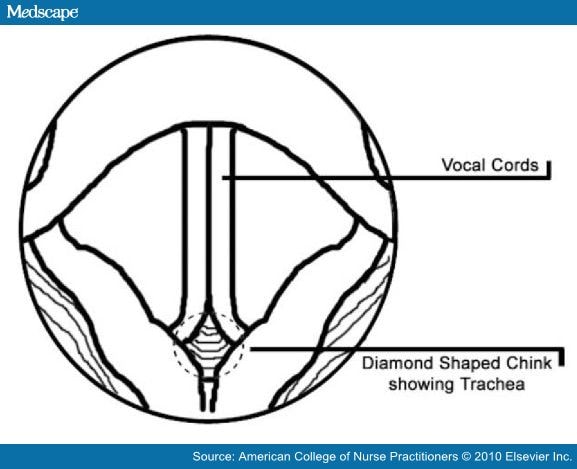
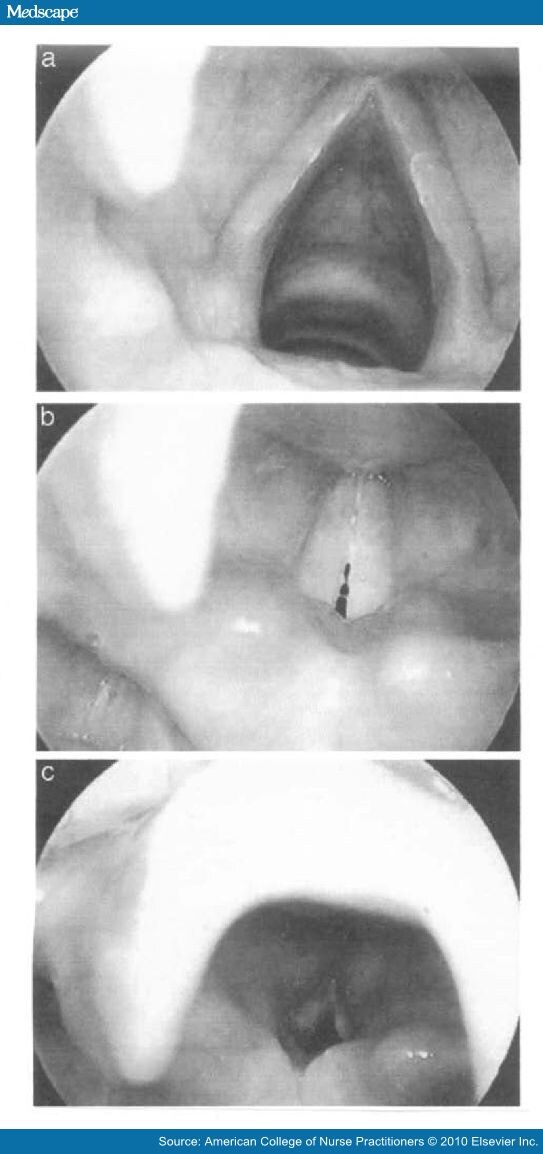
During patient inspiration, the healthcare provider can see the vocal cords adduct and may see a posterior "diamond-shaped chink" on examination with a laryngoscope.[16] (Figure 3, Figure 4). With laryngoscopy, vocal fold adduction can be seen on inspiration; this reduces inspiratory air flow with a normal expiratory flow.[15] The diagnosis of VCD is confirmed with direct examination but may be normal in 50% of people if their symptoms are not present during inspection.[5]
Figure 3.
Vocal cord adduction.
Figure 4.
A, Vocal cord abduction during normal inhalation. B, Vocal cords during normal phonation. C, Severe vocal cord adduction that clearly shows the diamond shaped posterior chink.
Other diagnoses to consider in the differential include anaphylaxis, croup, epiglottitis, foreign body aspiration, exercise-induced asthma, RTI, spasmodic dysphonia, tracheal stenosis, laryngeal collapse, thyroid tumor, subglottic mass, brainstem compression, and panic disorder.[4,8,13] VCD is often mistaken for exercise-induced bronchospasm, but the inspiratory stridor seen in this condition resolves quickly with rest and distraction.[12]
Contributing factors for VCD include gastroesophageal reflux, inhalation of irritants (e.g., dust, smoke, fumes, cleaning chemicals), increased cough reflex sensitivity and hyperreactivity of the airway, and emotional stressors.[4,13,15] Movement of the diaphragm when laughing or singing may worsen reflux, causing a cough and triggering vocal cord symptoms as well.[15]
It is essential that coexisting medical conditions such as asthma and gastroesophageal reflux be considered and a careful history obtained to determine if patient's inspiratory constriction is a result of stridor, dysphagia, or aspiration.[1] Providers should be aware that habitual cough and throat clearing increases sensitivity of the vocal cords as well.[2] Patient history should include presence of inspiratory or expiratory stridor, the pattern of symptoms (continuous, intermittent), triggers (allergens, symptoms occur after meals or awaken patient, associated with activity, stress), and associated symptoms, including hoarseness, chest or throat tightness, cough, dysphagia, heartburn, and globus sensation.[1]
Past medical history should include the presence of allergies, asthma, gastroesophageal reflux, dysphagia, stroke, brain tumor, head injury, vocal cord paralysis, and use of psychiatric medications.[1] Phenothiazines such as Thorazine (chlorpromazine) and Mellaril (thioridazine) are associated with extrapyramidal signs, including transient VCD.[13]
Patients benefit from reassurance that their condition is neither imagined nor life threatening.[4] VCD has long been correlated with conversion disorder and other psychiatric diagnoses.[17,18] However, there are often physical findings found on laryngoscopy and flattening of the inspiratory flow loop on spirometry that cannot be ignored. Placing too much emphasis on psychogenic causes or implying the patient is malingering will undoubtedly cause the patient to seek diagnosis and treatment elsewhere.[8,11]
Additional workup for VCD may include a chest x-ray if there is a chronic cough. Airway fluoroscopy and ultrasound of the vocal cords are still being investigated as non-invasive means of diagnosing these patients.[10] Allergy skin testing, eosinophil count, and serum immunoglobulin E levels help differentiate between asthma and VCD as asthma is often associated with allergies.[19] If there is a suspicion of hereditary angioedema with dyspnea, C1 inhibitor and C4 levels may be drawn as well.[19] Arterial blood gases are generally performed only during an acute asthma episode and will be normal in patients with VCD.[19]
Journal for Nurse Practitioners. 2010;6(9):675-682. © 2010 Elsevier Science, Inc.
Cite this: Diagnosis and Management of Vocal Cord Dysfunction - Medscape - Oct 01, 2010.









Comments