Advertisement
New Technology Can Identify Bacteria's Genetic Make-Up, Fight Drug Resistance
Resume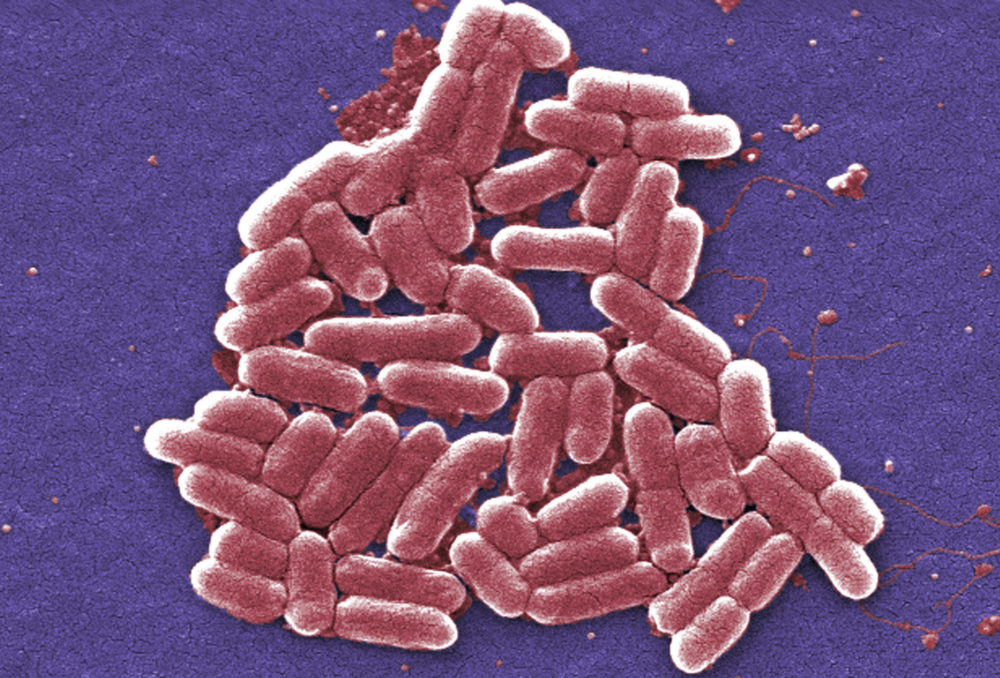
About 2 million Americans get drug-resistant infections every year, according to the Centers for Disease Control and Prevention — and about 23,000 patients die.
That resistance is wreaking havoc with patients suffering from urinary tract infections, leading to hospitalizations and even deaths, as well as lower respiratory tract infections, which doctors say patients are being routinely over-treated for before a correct diagnosis is made.
A new diagnostic tool that identifies bacteria quickly, at a genetic level, might help patients and fight antibiotic resistance.
“I'm pretty optimistic that our technology can solve these problems — the combination of rapid precision medicine diagnostics combined with new drug discovery,” says Evan Jones, CEO of the biotechnology company OpGen, which developed the diagnostic tool. “Having said that, there's so much inertia in the health care system that translating that into action and change has got to happen quickly.”
Oftentimes, doctors will prescribe a patient antibiotics without a proper diagnosis because testing isn’t fast enough, Jones says. With the new diagnostic tool, doctors will no longer have to play a guessing game of which antibiotic might help a patient.
The tool provides a proper diagnosis in just two to three hours, compared to a few days now with current urine tests, by testing the DNA of microbes found in the infection, Jones says.
“It's direct from the urine sample and will tell the physician what's the level of the microbe, what microbe is it,” he says. “And then we look at the antibiotic resistance genes, upload that data to the cloud, and give a report that says, 'OK, here's the antibiotics that this patient's likely to be susceptible to. And here are the ones that we predict resistance.’ ”
Interview Highlights
On the current state of antibiotic resistance
“It's a huge and growing problem. If you take a step back and just think about what's happened, antibiotics were first discovered around World War II. Before World War II, if you had an infection, you often lost a limb or died. That set the table for huge medical advances over the last 70 years, and a lot of them are at risk now. As antibiotics have been used, resistance is rising. And in this decade, particularly in areas like urinary tract infections, the rates of increase of resistance can be up in the 30% per-year-rate. So that sets the table for some of these problems that we're talking about.”
On antibiotic resistance to UTIs
“There's about 10 million cases a year of people with UTI infections. For the vast majority of them, about 8 million a year, you can probably treat them safely with what they call empiric therapy. So you have an idea of what antibiotics will work for that group of patients, and you simply prescribe in advance of having a confirmatory diagnostic result.
“But if you are of the two million that have something more complicated — the remaining 20 or 30% — if you tried that empirical approach, you would have given them the wrong medicine. They'd be resistant to it.”
On why it’s important to treat UTI patients quickly and correctly
“Almost everyone knows someone who's had a urinary tract infection that progressed into the kidney, then went from the kidneys up into the bloodstream. So this is an early stage of an infection that can become much more serious. So it's critical to treat these patients correctly. And we did a large outcome study with an integrated health care delivery network that showed that for every day the patient was on the wrong antibiotic, that could translate to up to two days length of stay in the hospital. So in this facility, it took three days to get the right decision. That would be six extra days of hospitalization.
“The more resistant the pathogen, the more complicated the testing needs to be. So in the simple case, they can oftentimes give you the results in a day or two, but if it's a multidrug resistant pathogen, that testing can take another two to three days.”
On if the new technology will be applicable to other infections besides UTIs
“It will be applicable really across the board of acute care infections. Our next area of focus is lower respiratory tract infections. The data suggests that up to 50 percent of those specimens, the classic microbiology, is ineffective. And so it's ripe for need of rapid, couple-of-hour DNA tests that can tell you what pathogen's there, what's the right antibiotic. This area of lower respiratory infections is one where patients are getting a lot of overtreatment. If you present yourself in an emergency room and say … you have acute pneumonia, they could treat you with up to five antibiotics and antifungals before they know what you have. And of course usually you only need one of those, so you can see that it's costing the system a lot of money. It creates more resistance, and it damages the patient.”
On what clinical trials have revealed about the technology
“We've been working for several years on this and recently completed a large outcome study with three large health care systems, and showed that this new technology is about 90% accurate in terms of making the antibiotic predictions, and even more accurate in saying, 'Yes, you have a UTI that needs treatment right away.'
“We have begun our clinical trials, [an] early version of the test is pending in front of FDA, and then that will be followed by a clearance hopefully of the information technology we call the 'lighthouse' that interprets the genomic test result.”
Karyn Miller-Medzon produced and edited this interview for broadcast with Todd Mundt. Samantha Raphelson adapted it for the web.
This segment aired on October 14, 2019.
