Coronavirus Disease 2019
Troubles Ahead for the Unvaccinated
What is the price of not getting vaccinated?
Posted June 25, 2021 Reviewed by Ekua Hagan
Key points
- A study on brain tissue identified changes in the brain in COVID-19 patients, including loss of grey matter.
- Possible long-term effects of COVID-19 and its variants include brain pathologies and cognitive deficits.
- The long-lasting cost to society of post-COVID cognitive impairment could be suicides, crimes, and failed friendships.
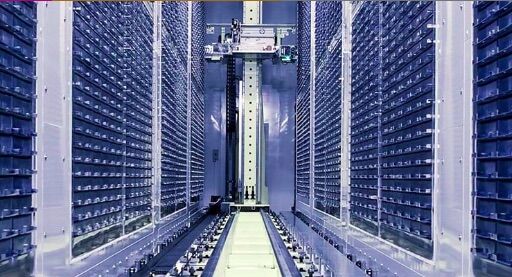
Long before the COVID-19 outbreak, UK Biobank, a biomedical research database information center, collected brain scans of 40,000 volunteers. The data were stored for biomedical research on common life-threatening diseases but not particularly for viruses of any kind.
In January 2021, when COVID-19 vaccines were starting to become available, and the virus was well into its worldwide spread, hundreds of previously imaged participants returned to UK Biobank for a second brain scan. From 782 new scans, 394 participants had tested positive for SARS-CoV-2 infection sometime before their second CT, PET, or MRI scans.
The effects of COVID on brain tissue linger long after recovery.
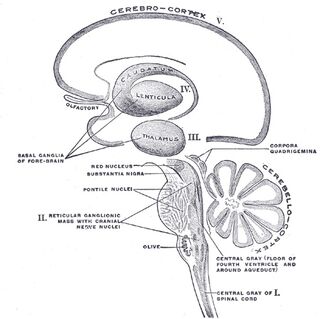
Researchers comparing old data with new ones were interested in COVID-19's long-lasting effects on the brain. They found major cerebral abnormalities involving white matter lesions and increased blood flow, surprising and troublesome outcomes for those who contracted the virus along with moderate to severe symptoms. Between 394 COVID-19 participants and 388 controls matched by age, sex, ethnicity, and intervals between scans, there were identifiable changes in the brain, including loss of grey matter in three areas. They “identified significant effects of COVID-19 in the brain with loss of grey matter surrounding the hippocampus, the left lateral orbitofrontal cortex”—controlling sensory integration and decision-making—and “the left insula” that plays a role in empathy and social cognition functioning."
It means that there is strong evidence for brain pathologies associated with possible cognitive deficits for 80% of patients who experience severe neurological symptoms due to COVID-19. Moreover, for those severe cases, the virus could continue to be active in the central nervous system long after tests prove to be negative.
Risks for the unvaccinated
For the unvaccinated: COVID is coming for you, and it no longer plays nice.
I am sure we all hope COVID does not leave long-term effects. My worries are for the unvaccinated and for those who have had to deal with COVID-19 directly. The old variants have left their marks, but new ones are far more severe in every respect. So the hope is that this new research is a warning signal for those that are hesitant.
Hesitant people may have good reasons for their COVID-19 views. Some have underlying issues connected to allergic reactions, immune deficiencies, and other health issues. With this current information, however, there should be new considerations in debating whether or not to be vaccinated. Survival may no longer mean escaping death with a full recovery. Recent studies of post-sepsis syndrome show multifaceted problems long after severe bouts of the SARS virus.
Between the time of the first case, on January 22, 2020, and now, 33.5 million Americans (10% of the population) have tested positive for COVID-19. Approximately 3.6 million cases were considered severe enough to have long-standing possible brain pathologies associated with cognitive deficits leading to sensory integration and decision-making, empathy, and social cognition functioning. What will be the cost?
The price adds up in suicides, crimes, and failing friendships.
After sepsis, many cognitive, physical, and psychological impairments are expected. Memory decline, concentration, fatigue, and depression were reported for almost 90 percent of ICU patients for more than a year after release. Fifteen months ago, that was not expected. Many studies using neuroimaging practices have detected viral DNA in olfactory and brainstem areas with a dominance of cerebrovascular damage in white matter.
The damage might not be temporary, and it might not be what many people once believed to be a temporary loss of olfactory senses through damage to neuro-nasal passageways. Who knows what harm future variants will bring when they come for the unvaccinated? Lineage B.1.617.2, known as the Delta variant of SARS-CoV-2, has already gone through more than a dozen mutations with a random ugly happenstance of coming for the unvaccinated.
Fauci is worried. He says, "More worrisome is that we know that there are pockets of unvaccinated people. And so I would be worried about Delta spreading very quickly in those pockets."
In the US, benefits outweigh the risks by high-stakes winning odds with a godsend surplus of vaccines available to anyone over 12.
When Dr. Fauci says he is worried, so am I.
© 2021 Joseph Mazur
References
Paterson RW, Brown RL, Benjamin L, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain 2020; 143(10): 3104-20.
Meinhardt J, Radke J, Dittmayer C, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci 2021; 24(2): 168-75.
doi.org/10.3389/fnagi.2021.646908
Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit. Crit Care Med. 2012;40(2):502-509.
Hallie C. Prescott, Timothy D. Girard, “Recovery From Severe COVID-19 Leveraging the Lessons of Survival From Sepsis,” JAMA, 2020; 324(8) 739-740.
Ahmed H, Patel K, Greenwood DC, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalization or ICU admission. J Rehabil Med. 2020;52(5):jrm00063.
Manca R. De Marco M, Ince PG and Venneri A(2021) Heterogeneity in Regional Damage Detected by Neuroimaging and Neuropathological Studies in Older Adults With COVID-19: A Cognitive-Neuroscience Systemic Review to Inform the Long-Term Impact of the Virus on Neurocognitive Trajectories. Front. Aging Neurosci. 13:646908. Doi: 10.3389/fmagi.2021.646908.
Kai Kupferschmidt and Meridith Wadman, “Delta variant triggers new phase in the pandemic,” Science 25 June 2021: Vol. 372, Issue 6549, pp. 1375-1376




