Bacteria-fighting cells in the airways boosts infection risk from viruses
Having more bacteria-fighting immune cells in the nose and throat may explain why some people are more likely to be infected by respiratory viruses.
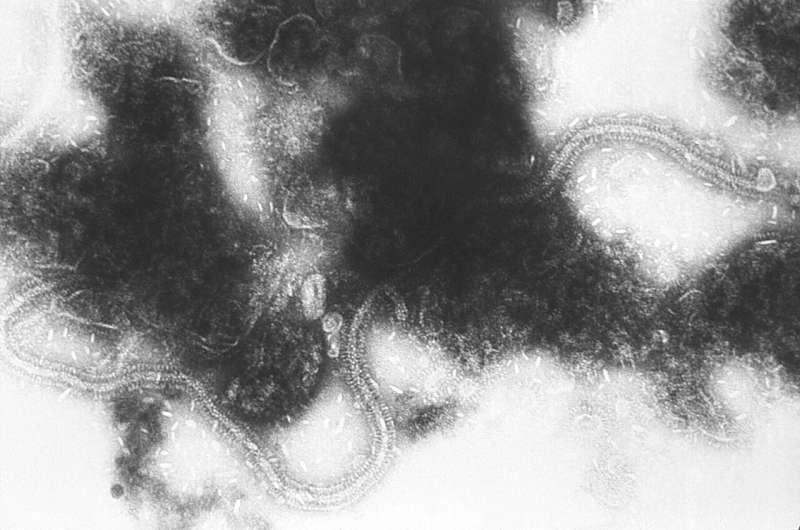
In a study, led by a team from Imperial College London and published today in Science, researchers found that volunteers who succumbed to infection from respiratory syncytial virus (RSV) had more specialized white blood cells called neutrophils in their airways before exposure to the virus, compared to those who staved off infection.
According to the researchers, this type of neutrophil-driven inflammation in the nose and throat—typically associated with fighting off bacterial infections—may compromise our ability to fight off invading viruses and make us more susceptible to viral infections.
The findings could help researchers to understand why people respond differently to the same viral threat, predict who is more at risk of infection, and even lead to preventative treatments to protect against RSV and potentially other respiratory viruses, including influenza and coronaviruses.
Same virus, different response
Dr. Ryan Thwaites, from the National Heart and Lung Institute at Imperial and study author, said: "If we think of a group of 10 people all exposed to the same strain of RSV under identical conditions, we'd expect around six of them to become infected and show symptoms, but the rest may be unaffected. To date, we have been unable to fully explain exactly why this is and why, under the same conditions, some people are more likely to succumb to respiratory viral infections. But this study offers tantalizing insights into how we might improve defenses against respiratory viruses, and potentially even COVID-19."
RSV is a common respiratory virus which typically causes the symptoms of a common cold in healthy adults. But for infants and the elderly it can lead to thousands of hospitalisations each year and can be fatal.
Unlike other respiratory viruses, such as influenza or rhinovirus, people can be infected by the same strain of RSV more than once. People can also react differently when exposed to the virus under the same conditions—some may get a mild infection while others get full-blown symptoms, and some may avoid infection altogether.
In the latest study, the team aimed to investigate the underlying mechanisms of why people succumb to RSV infection and the factors for the varied immune responses.
Healthy adults were enrolled to the study and exposed to RSV in a safe, controlled clinical setting where they were closely monitored. After receiving nasal drops containing the virus, 57% of volunteers became infected. Analysis of blood samples showed that the presence of protective antibodies and B and T cells could only partially explain who became infected.
Slipping through the net
However, when they analyzed samples from participants' airways taken before they were exposed to the virus, the team found evidence of neutrophil activation in the nasal mucosa—the cells lining the inside of the nose—in those who became infected with the virus.
These immune cells are known to release proteins which help create an antibacterial environment in response to a threat. But the researchers believe this antibacterial immune response may come at a cost, making a host more susceptible to viruses by effectively switching off the early warning system, letting them slip through the net to cause infection.
Professor Peter Openshaw, Professor of Experimental Medicine at Imperial and co-senior author on the study, said: "The variable transmission we see with respiratory viruses partly depends on the dose and duration of exposure, but also the person's own inbuilt immune defenses. You might assume that it's down to the presence of specific protective antibodies, but despite an immense effort over many years we have never really understood what makes one person vulnerable to RSV and another person resistant. Our finding that the state of the mucous membrane before the arrival of the virus is the major deciding factor is a real breakthrough. It seems as if the presence of activated neutrophils in the lining of the airways causes the mucous lining to fail to respond to the virus and to nip infection in the bud. Perhaps what's happening is that being ready to fight bacteria makes it more likely that viruses can gain a foothold. Once the virus does get in, our studies go on to show that there still is a chance that the infection will be terminated but only if the mucosa mounts an early defensive response. People who went on to get colds showed no evidence of an initial response; those who rejected the infection showed an immediate response before symptoms developed. These are the sort of findings that can only come from experimental studies in volunteers. We could never have discovered this by waiting for people with natural infections to present to us for investigation."
Human challenge studies
Dr. Christopher Chiu, Clinical Reader in Infectious Diseases at Imperial and co-senior author, said: "Our data highlight the complexity of the immune system, which has different arms providing layers of protection separated by anatomical location (such as the nose, lung or circulation) and timing. These different mechanisms may be directed to focus on a particular type of infection but this may come at the cost of protection against other pathogens. Controlled human infection challenge studies have a unique ability to tease out these complicated interactions and point out potential targets for prevention or treatment that cannot be seen in patients who have infections caused by diverse virus strains, in different amounts, on top of a wide range of other conditions that might affect their immunity."
To confirm the idea, they used animal models to test the impact of the neutrophilic pathway on RSV infection. In mice without neutrophilic inflammation, the immune system recognized the virus as a threat, releasing immune-mediating factors which cleared the infection with few symptoms.
However, in mice with a nasal mucosa rich in neutrophils this early detection of the virus was dampened. Under these antibacterial conditions, the virus was better able to invade the mucosal cells causing infection, worsened symptoms and shedding of the virus—to further transmit the virus.
The researchers say that if they can demonstrate the same mechanism is occurring in patient groups who are most at risk from RSV (babies under 12 months of age and adults over 65 with chronic conditions, such as COPD or asthma) it could help to identify subsets of patients most at risk.
Extending to other viruses
The team is set to explore the mechanism in larger patient groups as well as investigating whether the same immune mechanisms influence other viral respiratory infections, from influenza and coronaviruses.
Dr. Thwaites added: "Our initial studies show that in healthy people, neutrophilic inflammation in the airways is linked to RSV infection. If we can show this same mechanism is at play in those most at risk from the virus, it could provide opportunities to reduce the harms caused by RSV and other respiratory viruses. Severe bacterial respiratory infections tend to be quite rare in healthy adults so, in theory, it may be more beneficial to nudge the immune response towards fighting viruses during seasonal winter peaks. It might be possible to design therapies to temporarily inhibit some aspect of neutrophilic inflammation, such as through a simple nasal spray, to enhance protection against circulating viruses. This could be used in high risk settings, like hospitals, to enhance protection against respiratory viruses, prevent their spread and reduce the impacts of infection on vulnerable groups."
Dr. Cecilia Johansson, from Imperial's NHLI and study author, added: "Understanding the underlying mechanisms of susceptibility and protection against respiratory viruses is key for the development of treatments and therapies. By studying RSV infection in both human volunteer and in mice we are now one step closer in determining the delicate balance of resistance to virus infections and the lung disease these viruses can cause."
More information: Neutrophilic inflammation in the respiratory mucosa predisposes to RSV infection. Science, science.sciencemag.org/cgi/doi … 1126/science.aba9301




















