Identity
Our Identity Is Defined by Our Moral Character
Research suggests that how we are perceived crucially depends on our values.
Posted June 23, 2019
Have you ever wondered just what it is that makes you, you? If all of your memories were to fade away, would your identity dissolve along with them? Would friends and family no longer perceive you to be the same person as before? For the 5.3 million Americans experiencing memory loss due to Alzheimer’s disease, these frightening questions are more than just theoretical.
Fortunately, science appears to suggest that being robbed of one’s memory does not equate with being robbed of one’s identity. A study published in the journal Psychological Science has found that “who one is” is largely defined by one’s moral behavior and not by one’s memory capacity or other cognitive abilities. Thus, although Alzheimer’s and other neurodegenerative diseases may powerfully impact the mental functioning of individuals, sufferers can find some solace in the fact that substantial memory deficits—when unaccompanied by changes in moral characteristics—seem to have no effect on how others perceive “who you are.”
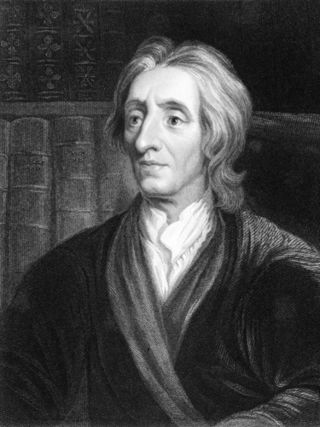
Determining the factors that define one’s identity is an old philosophical problem that first received serious consideration in the 17th century by the early British empiricist, John Locke. According to Locke’s “memory theory,” a person’s identity only reaches as far as their memory extends into the past. In other words, who one is critically depends upon what one remembers. Thus, as a person’s memory begins to disappear, so does his identity.
This notion of identity as memory has received experimental support from psychology research. A 2004 study followed Alzheimer’s patients and found that those exhibiting impairments in autobiographical memory—one’s knowledge of their own past experiences and events—on standard psychological tests showed changes in the strength and quality of identity. The strength of identity was measured by the number of unique statements given by the patient in response to the question, “Who am I?” while the quality of identity was measured by the abstractness of their answers, i.e., their lack of specific details. These findings seem to imply that autobiographical memories create a continuous, first-person narrative that helps form a sense of self.
However, other scientists remain unconvinced of Locke’s premise, as some theorize that more central to identity is moral capacity—a variable that these previous studies did not adequately control for. Evidence for this idea comes from social cognition research, which has found that impression formation is largely dependent on the moral dimension. In other words, how we see people—whether they are positive or negative, to be approached or avoided—is mostly determined by our assessment of their moral character and not their intellect, knowledge, or other personality traits. The concept that morals are essential to identity is aptly known as the essential-moral-self hypothesis.
Researchers from the University of Arizona and Yale decided to investigate this hypothesis directly in a real-world clinical population. Their study was designed to test what types of cognitive damage cause people to no longer appear to be themselves to others. A crucial element of the design was testing for changes in identity from the perspective of a third-person observer, rather than the individual himself. In addition to sidestepping many of the reliability problems intrinsic to first-person accounts, focusing on perceived identity allowed the investigators to assess the effects of memory and moral changes on the patient’s relationship with others. This is an extremely important facet, because when someone appears to be “not the same person,” the social bonds between patients and loved ones or caregivers quickly deteriorate. These bonds are critical to one’s well-being and health, as they are the source of the connectedness one feels to the people in their lives and the outside world.
The investigators recruited 248 volunteers with family members who suffered from one of three types of neurodegenerative diseases. Patients had either Alzheimer’s disease, frontotemporal dementia, or amyotrophic lateral sclerosis (ALS), each of which is characterized by relatively distinct cognitive and behavioral changes. While ALS primarily affects motor but not mental function, both Alzheimer’s and frontotemporal dementia affect cognition. However, where Alzheimer’s strongly affects things like memory and IQ, those with frontotemporal dementia tend to undergo changes in moral traits—i.e., things like honesty, compassion, decency, and integrity.
The participants, most of whom were married to or romantically involved with the patients, were instructed to indicate how much the patient had changed in 30 trait categories since the disease began; 15 were related to morality and the other 15 to personality. To evaluate the degree of change in the perceived identity, participants were asked to give information regarding any differences in their relationship with the patient that had occurred over the course of the disease’s progression. For example, they were asked questions like, “Does the patient ever seem like a stranger to you?” and “Do you feel like you still know who the patient is?”
Analysis of the data revealed that participants perceived the greatest disruptions in patients’ identity when they observed changes in moral traits. Other cognitive deficits—like those seen with amnesia—had no measurable effect on the perception of identity. Consequently, those with frontotemporal dementia showed the greatest changes in perceived identity, since it specifically affects the frontal lobe functions underlying moral reasoning and behavior.
Interestingly, those with ALS showed no significant change in perceived identity despite the distorted physical appearance that results from the widespread deterioration of motor function. Although there were minor changes in identity perception in those with Alzheimer’s, this was associated with changes in moral traits and not memory loss.
These findings have important implications for patients with neurodegenerative diseases. Efforts aimed at helping sufferers to understand themselves in terms of their moral traits—characteristics like altruism, mercy, and generosity—can restore their sense of identity and control as memory fades or cognition declines. Simply knowing that others continue to perceive them as the same person, even when they feel that their own identity is changing, can allow them to securely protect their sense of self. Additionally, the results highlight the need for future neurological interventions and clinical therapies that specifically focus on maintaining those cognitive faculties involved in moral function in the face of disease.
This article was originally published at Scientific American.




