Abstract
Placental transfusion results in a significant decrease in the risk of death for extremely preterm infants. With immediate cord clamping (ICC), these infants can leave up to one-half of their normal circulating in utero blood volume in the placenta. Extremely preterm infants are at highest risk of harm from ICC yet are currently the most likely to receive ICC. Receiving a placenta transfusion provides infants with life-saving components and enhanced perfusion. We present some lesser-known but important effects of placental transfusion. New research reveals that enhanced vascular perfusion causes an organ’s endothelial cells to release angiocrine responses to guide essential functions. High progesterone levels and pulmonary artery pressure in the first few hours of life assist with neonatal adaptation. We propose that lack of essential blood volume may be a major factor contributing to inflammation, morbidities, and mortality that preterm infants frequently encounter.
Key points
-
Placental transfusion provides enhanced vascular perfusion and reduces the risk of death for preterm infants
-
Enhanced vascular perfusion stimulates endothelial cells to release vital angiocrine messengers to guide normal function and development of neonatal organs
-
High progesterone levels and pulmonary artery pressure in the first 12 h may assist the newborn to adapt to the placental transfusion throughout the body
-
Blood volume conservation is important at birth and during the NICU stay for preterm infants
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Augustin HG, Koh GY. Organotypic vasculature: from descriptive heterogeneity to functional pathophysiology. Science. 2017;357:6353.
Committee on Obstetric Practice. Committee Opinion No. 684. Delayed umbilical cord clamping after birth. Obstet Gynecol. 2017;129:e5–10.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Backes CH, Rivera BK, Haque U, Bridge JA, Smith CV, Hutchon DJR, et al. Placental transfusion strategies in very preterm neonates: a systematic review and meta-analysis. Obstet Gynecol. 2014;124:47–56.
Rabe H, Gyte GM, Díaz-Rossello JL, Duley L. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Pregnancy and Childbirth Group, editor. Cochrane Database Syst Rev. 17 Sep 2019. http://doi.wiley.com/10.1002/14651858.CD003248.pub4. Accessed 10 Nov 2019.
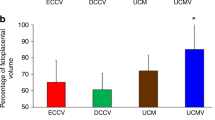
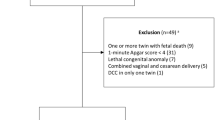
Lodha A, Shah PS, Soraisham AS, Rabi Y, Abou Mehrem A, Singhal N, et al. Association of deferred vs immediate cord clamping with severe neurological injury and survival in extremely low-gestational-age neonates. JAMA Netw Open. 2019;2:e191286.
Katheria A, Garey D, Truong G, Akshoomoff N, Steen J, Maldonado M, et al. A randomized clinical trial of umbilical cord milking vs delayed cord clamping in preterm infants: neurodevelopmental outcomes at 22–26 months of corrected age. J Pediatr. 2018;194:76–80.
Mercer JS, Erickson-Owens DA, Vohr BR, Tucker RJ, Parker AB, Oh W, et al. Effects of placental transfusion on neonatal and 18 month outcomes in preterm infants: a randomized controlled trial. J Pediatr. 2016;168:50–55. e1.
Rabe H, Sawyer A, Amess P, Ayers S. Brighton Perinatal Study Group Neurodevelopmental outcomes at 2 and 3.5 years for very preterm babies enrolled in a randomized trial of milking the umbilical cord versus delayed cord clamping. Neonatology. 2016;109:113–9.
Bhatt S, Polglase GR, Wallace EM, te Pas AB, Hooper SB. Ventilation before umbilical cord clamping improves the physiological transition at birth. Front Pediatr. 20 Oct 2014. http://journal.frontiersin.org/article/10.3389/fped.2014.00113/abstract. Accessed 4 Oct 2019.
Cashore W. Hypovolemia resulting from a tight nuchal cord at birth. Pediatr Res. 1973;7:399.
Chaudhury S, Saqibuddin J, Birkett R, Falcon-Girard K, Kraus M, Ernst LM, et al. Variations in umbilical cord hematopoietic and mesenchymal stem cells with bronchopulmonary dysplasia. Front Pediatr. 2019;7:475.
Cotten CM, Murtha AP, Goldberg RN, Grotegut CA, Smith PB, Goldstein RF, et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J Pediatr. 2014;164:973. e1.
Liao Y, Cotten M, Tan S, Kurtzberg J, Cairo MS. Rescuing the neonatal brain from hypoxic injury with autologous cord blood. Bone Marrow Transpl. 2013;48:890–900.
Yao AC, Moinian M, Lind J. Distribution of blood between infant and placenta after birth. Lancet Lond Engl. 1969;2:871–3.
Sippell WG, Becker H, Versmold HT, Bidlingmaier F, Knorr D. Longitudinal studies of plasma aldosterone, corticosterone, deoxycorticosterone, progesterone, 17-hydroxyprogesterone, cortisol, and cortisone determined simultaneously in mother and child at birth and during the early neonatal period. I. Spontaneous delivery. J Clin Endocrinol Metab. 1978;46:971–85.
Trotter A, Maier L, Kron M, Pohlandt F. Effect of oestradiol and progesterone replacement on bronchopulmonary dysplasia in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2007;92:F94–98.
González-Orozco JC, Camacho-Arroyo I. Progesterone actions during central nervous system development. Front Neurosci. 2019;13:503.
Berger R, Söder S. Neuroprotection in preterm infants. BioMed Res Int. 2015;2015:1–14.
Katheria AC, Lakshminrusimha S, Rabe H, McAdams R, Mercer JS. Placental transfusion: a review. J Perinatol. 2017;37:105–11.
Kresch M. Management of the third stage of labor: how delayed umbilical cord clamping can affect neonatal outcome. Am J Perinatol. 2017;34:1375–81.
Mercer JS, Erickson-Owens DA. Rethinking placental transfusion and cord clamping issues. J Perinat Neonatal Nurs. 2012;26:202–17. quiz 218–9.
Tolosa JN, Park D-H, Eve DJ, Klasko SK, Borlongan CV, Sanberg PR. Mankind’s first natural stem cell transplant. J Cell Mol Med. 2010;14:488–95.
Li J, Wang Z, Chu Q, Jiang K, Li J, Tang N. The strength of mechanical forces determines the differentiation of alveolar epithelial cells. Dev Cell. 2018;44:297–312. e5.
Peng T, Morrisey EE. Development of the pulmonary vasculature: current understanding and concepts for the future. Pulm Circ. 2013;3:176–8.
Rafii S, Butler JM, Ding B-S. Angiocrine functions of organ-specific endothelial cells. Nature 2016;529:316–25.
Pasquier J, Ghiabi P, Chouchane L, Razzouk K, Rafii S, Rafii A. Angiocrine endothelium: from physiology to cancer. J Transl Med. 2020;18:52.
Lorenz L, Axnick J, Buschmann T, Henning C, Urner S, Fang S, et al. Mechanosensing by β1 integrin induces angiocrine signals for liver growth and survival. Nature 2018;562:128–32.
Morrisey EE, Hogan BLM. Preparing for the first breath: genetic and cellular mechanisms in lung development. Dev Cell. 2010;18:8–23.
Li J, Tang N. May the force be with you. Dev Cell. 2018;47:673–4.
Askenazi D, Selewski D, Willig L, Warady B. Chapter 90. Acute kidney injury and chronic kidney disease. In: Gleason C, Juul S (eds). Avery’s disease of the newborn. 10th ed. Philadephia, PA: Elsevier; 2018. p. 1280–5.
Awad AS, Okusa MD. Distant organ injury following acute kidney injury. Am J Physiol-Ren Physiol. 2007;293:F28–9.
Oh WOM, Lind J. Renal function and blood volume in newborn infant related to placental transfusion. Acta Paediatr Scand. 1967;55:197–210.
Arcilla RA, Oh W, Wallgren G, Hanson JS, Gessner IH, Lind J. Quantitative studies of the human neonatal circulation. II. Hemodynamic findings in early and late clamping of the umbilical cord. Acta Paediatr Scand 1967;179(Suppl):25.
Arcilla RA, Oh W, Lind J, Gessner IH. Pulmonary arterial pressures of newborn infants born with early and late clamping of the cord. Acta Paediatr. 1966;55:305–15.
Nelle M, Zilow EP, Bastert G, Linderkamp O. Effect of Leboyer childbirth on cardiac output, cerebral and gastrointestinal blood flow velocities in full-term neonates. Am J Perinatol. 1995;12:212–6.
Oh W, Lind J. Body temperature of the newborn infant in relation to placental transfusion. Acta Paediatr Scand. 1967;172(Suppl):135.
Oh W, Lind J, Gessner IH. The circulatory and respiratory adaptation to early and late cord clamping in newborn infants. Acta Paediatr Scand. 1966;55:17–25.
Pietra GG, D’Amodio MD, Leventhal MM, Oh W, Braudo JL. Electron microscopy of cutaneous capillaries of newborn infants: effects of placental transfusion. Pediatrics 1968;42:678–83.
Plosa E, Guttentag SH. Lung development. In: Gleason C, Juul S (eds). Avery’s diseases of the newborn. 10th ed. Philadephia, PA: Elsevier; 2018. p. 586–99.
Hooper SB, Harding R. Fetal lung liquid: a major determinant of the growth and functional development of the fetal lung. Clin Exp Pharm Physiol. 1995;22:235–47.
Jaykka S. Capillary erection and the structural appearance of fetal and neonatl lungs. Acta Paediatr. 1958;47:484–500.
Haworth SG, Hall SM, Chew M, Allen K. Thinning of fetal pulmonary arterial wall and postnatal remodelling: ultrastructural studies on the respiratory unit arteries of the pig. Virchows Arch A Pathol Anat Histopathol. 1987;411:161–71.
Hall SM, Haworth SG. Normal adaptation of pulmonary arterial intima to extrauterine life in the pig: ultrastructural studies. J Pathol. 1986;149:55–66.
Mercer JS, Skovgaard RL. Neonatal transitional physiology: a new paradigm. J Perinat Neonatal Nurs. 2002;15:56–75.
Avery ME, Frank NR, Gribetz I. The inflationary force produced by pulmonary vascular distension in excised lungs. J Clin Invest. 1959;38:456–62.
Weibel ER, Gomez DM. Architecture of the human lung: use of quantitative methods establishes fundamental relations between size and number of lung structures. Science. 1962;137:577–85.
Sherwood L. Human physiology: from cells to systems. 9th ed. Boston, MA, USA: Cengage Learning; 2016. 1 p.
Sherwood L. Human physiology: from cells to systems. 8th ed. Belmont, CA: Brooks/Cole, Cengage Learning; 2013. 1 p.
Giovannini N, Crippa B, Denaro E, Raffaeli G, Cortesi V, Consonni D, et al. The effect of delayed umbilical cord clamping on cord blood gas analysis in vaginal and caesarean‐delivered term newborns without fetal distress: a prospective observational study. BJOG Int J Obstet Gynaecol. 2020;127:405–13.
Wiberg N, Källén K, Olofsson P. Delayed umbilical cord clamping at birth has effects on arterial and venous blood gases and lactate concentrations. BJOG Int J Obstet Gynaecol. 2008;115:697–703.
Mokarami P, Wiberg N, Olofsson P. Hidden acidosis: an explanation of acid-base and lactate changes occurring in umbilical cord blood after delayed sampling. BJOG Int J Obstet Gynaecol. 2013;120:996–1002.
Kirpalani H, Ratcliffe SJ, Keszler M, Davis PG, Foglia EE, Te Pas A, et al. Effect of sustained inflations vs intermittent positive pressure ventilation on bronchopulmonary dysplasia or death among extremely preterm infants: the SAIL randomized clinical trial. JAMA 2019;321:1165–75.
Jackson JC, Truog WE, Standaert TA, Juul SE, Murphy JH, Chi EY, et al. Effect of high-frequency ventilation on the development of alveolar edema in premature monkeys at risk for hyaline membrane disease. Am Rev Respir Dis. 1991;143:865–71.
Barbagallo M, Dominguez LJ, Licata G, Shan J, Bing L, Karpinski E, et al. Vascular effects of progesterone: role of cellular calcium regulation. Hypertension. 2001;37:142–7.
Linderkamp O. Placental transfusion: determinants and effects. Clin Perinatol. 1982;9:559–92.
Baker EK, Jacobs SE, Lim R, Wallace EM, Davis PG. Cell therapy for the preterm infant: promise and practicalities. Arch Dis Child Fetal Neonatal Ed. 2020;105:563–8.
Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH, et al. Bronchopulmonary dysplasia. Nat Rev Dis Prim. 2019;5:78.
Haneline LS, Marshall KP, Clapp DW. The highest concentration of primitive hematopoietic progenitor cells in cord blood is found in extremely premature infants. Pediatr Res. 1996;39:820–5.
Wisgrill L, Schüller S, Bammer M, Berger A, Pollak A, Radke TF, et al. Hematopoietic stem cells in neonates: any differences between very preterm and term neonates? PLoS One. 2014;9:e106717.
Makley AT, Goodman MD, Belizaire RM, Friend LAW, Johannigman JA, Dorlac WC, et al. Damage control resuscitation decreases systemic inflammation after hemorrhage. J Surg Res. 2012;175:e75–82.
Rajnik M, Salkowski CA, Thomas KE, Li Y-Y, Rollwagen FM, Vogel SN. Induction of early inflammatory gene expression in a murine model of nonresuscitated, fixed-volume hemorrhage. Shock Augusta Ga. 2002;17:322–8.
Makley AT, Goodman MD, Friend LAW, Deters JS, Johannigman JA, Dorlac WC, et al. Resuscitation with fresh whole blood ameliorates the inflammatory response after hemorrhagic shock. J Trauma. 2010;68:305–11.
Carroll PD, Widness JA. Nonpharmacological, blood conservation techniques for preventing neonatal anemia—effective and promising strategies for reducing transfusion. Semin Perinatol. 2012;36:232–43.
Hellström W, Forssell L, Morsing E, Sävman K, Ley D. Neonatal clinical blood sampling led to major blood loss and was associated with bronchopulmonary dysplasia. Acta Paediatr. 2020;109:679–87.
Katheria AC. Neonatal resuscitation with an intact cord: current and ongoing trials. Children 2019;6:60.
Kuehne B, Kirchgaessner C, Becker I, Kuckelkorn M, Valter M, Kribs A, et al. Mask continuous positive airway pressure therapy with simultaneous extrauterine placental transfusion for resuscitation of preterm infants—a preliminary study. Biomed Hub. 2018;3:1–10.
Christensen RD, Lambert DK, Baer VL, Montgomery DP, Barney CK, Coulter DM, et al. Postponing or eliminating red blood cell transfusions of very low birth weight neonates by obtaining all baseline laboratory blood tests from otherwise discarded fetal blood in the placenta. Transfus (Paris). 2011;51:253–8.
Carroll PD, Christensen RD. New and underutilized uses of umbilical cord blood in neonatal care. Matern Health Neonatol Perinatol. 2015;1:16.
Rosebraugh MR, Widness JA, Nalbant D, Veng-Pedersen P. A mathematical modeling approach to quantify the role of phlebotomy losses and need for transfusions in neonatal anemia. Transfus (Paris). 2013;53:1353–60.
Rabe H, Wacker A, Hülskamp G, Hörnig-Franz I, Schulze-Everding A, Harms E, et al. A randomised controlled trial of delayed cord clamping in very low birth weight preterm infants. Eur J Pediatr. 2000;159:775–7.
Rabe H, Alvarez J, Lawn C, Seddon P, Amess P. A management guideline to reduce the frequency of blood transfusion in very-low-birth-weight infants. Am J Perinatol. 2009;26:179–83.
Acknowledgements
The authors wish to thank John (Jack) Widness, MD, for his generous and insightful reviews of this article.
Author information
Authors and Affiliations
Contributions
JSM conceived of the idea for the paper; all authors made substantial contributions, revised and reviewed the article, and finally approved the paper. All authors agree to be accountable for the information presented in the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mercer, J.S., Erickson-Owens, D.A. & Rabe, H. Placental transfusion: may the “force” be with the baby. J Perinatol 41, 1495–1504 (2021). https://doi.org/10.1038/s41372-021-01055-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01055-0
This article is cited by
-
What does the evidence tell us? Revisiting optimal cord management at the time of birth
European Journal of Pediatrics (2022)