Organ-on-a-chip: New age research to replace animal testing
The global disease burden is on a constant rise, with deadly diseases like cancer and many more continuing to claim countless lives every year. But did you know that there is another crisis that is looming around the corner that is further fueling the burden of diseases? We are losing the battle to bring novel drugs to the market for the treatment of such diseases, which is causing people to suffer even more. The way we currently develop drugs takes on average 10 to 12 years to get to the market. But have you wondered why it takes such a long time to discover drugs for diseases? Before we can test the drugs on humans, they are subjected to different tests to prove their safety and efficacy. These tests, called preclinical trials, are being carried out in various model systems. For instance, one of the latest systems used is 3D cell culture. The main feature of this tool is that it provides the cells a medium to proliferate in all three dimensions just like they do inside the body. This allows examination of human tissues in their inherent architecture and functionality in the laboratory. Before the innovation of such a sophisticated tool, researchers used the traditional tools that were available - 2D cell culture and animals. Although these tools have been beneficial for advancements in medicine, they carry their baggage of limitations.
2D Culture- These are cells acquired from humans are cultured in dishes in laboratories. The cells attach to the dishes and proliferate in the form of a singular sheet, and thus these models are known as monolayers. This is the most simple and basic way of culturing human cells in laboratories. But a major limitation of this model is that cells do not behave or function in such a way inside the body. The Human body is a dynamic environment and cells inside the body are subjected to different mechanical forces all the time. Cells cultured in 2D simply do not represent the complexity and functionality of cells inside the body. This is why we move to animals to provide reliable results.
Animal models- Animals have been extensively used in research and they have contributed vital information about the physiology of different organs, mechanisms of diseases, and much more. But animal models have often failed to predict how a drug acts when given to humans. To give an example of the discrepancies in the data produced by animal testing, consider chocolate as a drug to treat a disease. As we know humans can safely consume chocolates, but if we test the ‘drug’ in dogs, they would die because of it. This simply tells that animals and humans process chemicals differently. This is backed by the staggering statistics for drug testing in animals that says that for every 10 drugs successful in animal models, 9 fail during the clinical trials on humans. That is a failure rate of 90%!
There is a need for new tools!
We are using outdated tools against new-age diseases that are far more complex. It’s like fighting with swords and shields against rifle guns. The poor success rate in drug development not only has repercussions on patients but also wastes a lot of resources. Billions of dollars are invested in drug research and development (R&D), but a high failure rate means that the overall productivity and efficiency are on a steep decline. Imagine spending billions over a span of 12 years to get nothing in return! That is devastating. Researchers acknowledged this gap in the preclinical models for drug discovery which ultimately led to the innovation of 3D cell culture. To test the drugs, all we needed was a way to culture human cells in their inherent complexity and architecture, but outside the body. 3D cell culture makes this possible because of its ‘near to in vivo’ characteristics. 3D cell culture provides a platform that preserves the cell-to-cell and cell-to-matrix interaction that are important for essential and cellular functions. This makes it a great tool to study mechanisms of disease and most importantly address the concerns regarding preclinical studies for drug discovery. However, 3D cell cultures fail to capture the true essence of living organs although superior to 2D cultures and animal models. Thus, researchers wanted a more sophisticated tool.
Organ-on-a-chip, a disruptive tool of modern medicine.
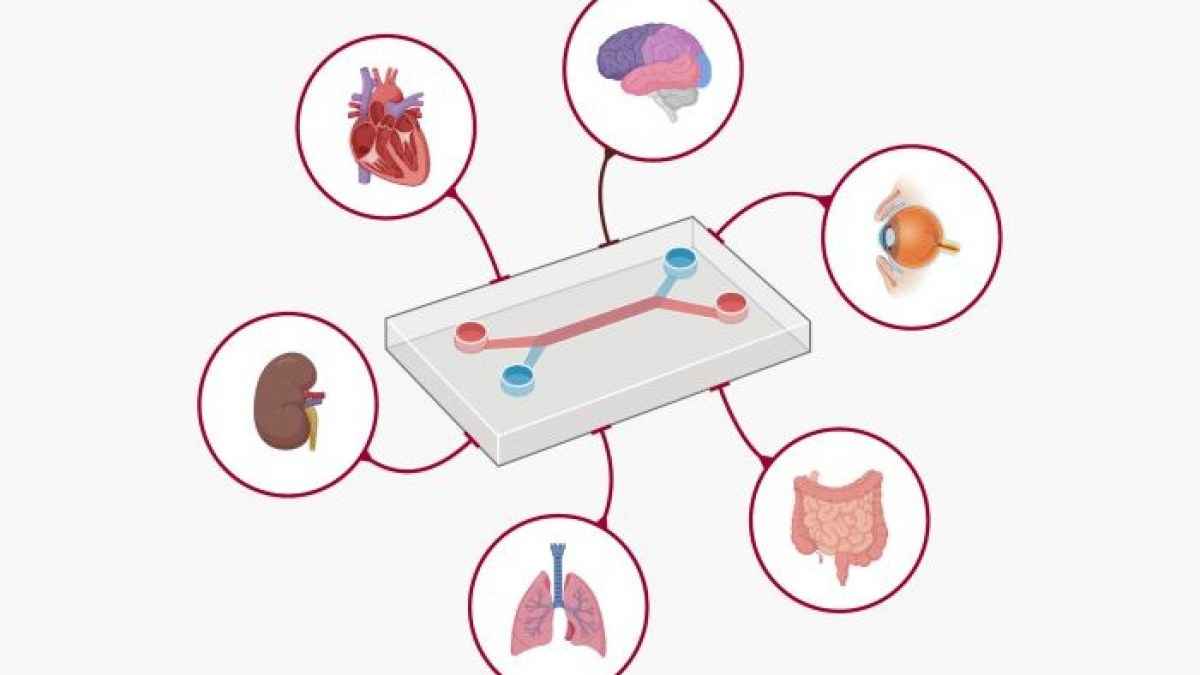
In recent years, biomedical engineers have integrated the foundations of 3D culture with microfluidic technology to create an innovative and powerful tool called organ-on-a-chip (OOC). These micro-engineered systems are not visually identical to a human organ but mimic the mechanical properties as well as the functioning of a living organ. They are embedded with microchambers and microvessels that allow a continuous supply of nutrients and oxygen. For instance, researchers at the Harvard Wyss Institute developed a lung-on-a-chip that demonstrates the exact physiology and functionality of an actual lung. The cells even undergo the mechanical strains that they face during breathing. Researchers across the globe have now successfully developed OOCs for multiple organ systems, including the liver, kidneys, and blood-brain barrier. But it doesn't end here. Due to the fluidic nature of the systems, multiple chips of different organs can be linked with each other to build more complex systems. New advancements and developments in the field will soon allow researchers to create ‘human-on-a-chip’.
What does this mean for the future of medicine?
We are facing a global health challenge and one of the key factors contributing to it is due to the current tools we are using to discover new therapies for diseases. It's time-consuming, requires more money, and is highly unreliable with a poor success rate. Disruptive innovations like OOC are very crucial to provide pharmaceutical industries an upper hand to speed up drug development. Mimicking the complex physiology of organs, OOCs enable researchers to accurately predict the efficacy and toxicity of a drug. They can also be used to identify novel drug delivery methods, for instance, lung-on-chip models can be used to test and analyze inflammatory responses to nanoparticle-mediated drug delivery. They offer a great alternative to traditional platforms for preclinical studies and could possibly put an end to animal testing. Cosmetic industries that often receive backlash for using animals to test their products can develop skin-on-chip models to establish the toxicity and safety of a potential cosmetic. The future prospects of organ-on-chips are limitless. They can be used to model complex deadly diseases like Cancer, Alzheimer's as well as infectious diseases like SARS and understand the mechanism of diseases which allows us to discover new therapeutic targets. OOCs, which are miniaturized organs, provide physiological relevant and yet powerful alternatives to existing 2D and animal models for researchers in academia and pharmaceutical industries for a wide range of biomedical applications.
Learn more about the recent research and technological developments in the field of organ on a chip at 3D cell culture workshop 2022. Register today at https://forms.gle/j358V2cn2dKtZJqb9
References :
- https://www.sciencedaily.com/releases/2012/11/121107141044.htm
- https://academic.oup.com/biostatistics/article/20/2/273/4817524
- https://onlinelibrary.wiley.com/doi/abs/10.1002/biot.202100154
Written by - Parth Choudhari, Science Communicator, Nanomedicine Research Group.