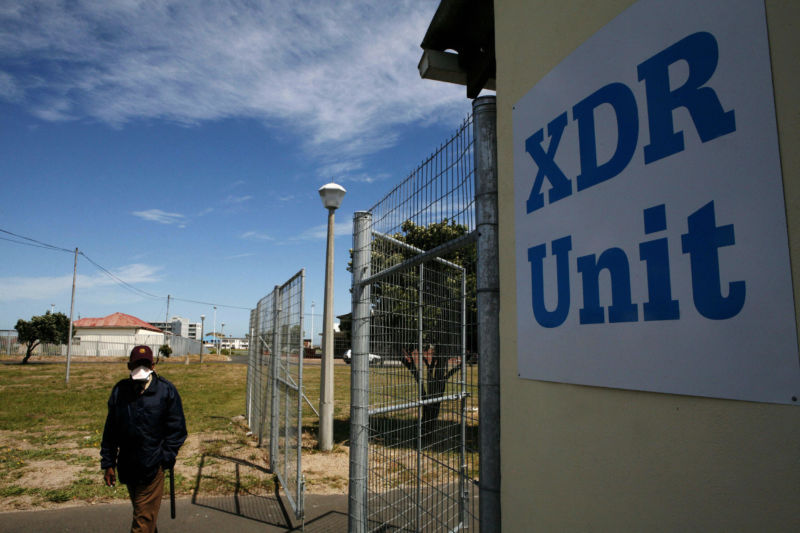
The Food and Drug Administration on Wednesday approved a new antibiotic that, when combined with two existing antibiotics, can tackle the most formidable and deadly forms of tuberculosis. The trio of drugs treats extensively drug-resistant tuberculosis (XDR-TB), along with cases of multidrug-resistant tuberculosis (MDR-TB) that have proven unresponsive to other treatments.
Tuberculosis is the single leading infectious killer in the world, infecting an estimated 10 million people in 2017 and killing 1.6 million of them. XDR-TB and MDR-TB are even more savage forms of the disease, which is caused by the bacterium Mycobacterium tuberculosis. The drug-resistant strains of TB kill an estimated 60% and 40% of their victims, respectively.
MDR-TB strains can resist at least the two most powerful anti-TB drugs, isoniazid and rifampin. A strain gets into XDR-territory when it also becomes resistant to any fluoroquinolone drug, such as ciprofloxacin or levofloxacin, plus at least one of three injectable second-line drugs, which are amikacin, kanamycin, and capreomycin. Drug-resistant strains of tuberculosis infected an estimated 558,000 people in 2017.
Existing treatments for MDR- and XDR-TB cases are long, complex, and often unsuccessful. Treatment regimens can include as many as eight antibiotics, taken for 18 months or longer. In the latest global report on tuberculosis, the World Health Organization found that MDR-TB treatments were only successful in 55% of cases, while treatments for XDR-TB had a success rate of 34%.The new three-drug regimen with the new FDA-approved antibiotic beats those figures handily, according to data from a small Phase III clinical trial. The regimen cleared the infection from 95 of 109 patients with XDR-TB or treatment-unresponsive MDR-TB in just six months. That’s an 87% treatment success rate for six months of treatment. (Two patients not included in the 95 extended their treatment to nine months.)
Triumphant trio
The three drugs in the lineup include two existing antibiotics: linezolid, which is used for drug-resistant infections, and a drug specifically developed for MDR-TB called bedaquiline. The newcomer is pretomanid, or PA-824.
Pretomanid was developed by the non-profit TB Alliance, which acquired the rights to it in 2002 from Chiron Corporation (which itself was later acquired by pharmaceutical giant Novartis). According to Reuters, TB Alliance this year granted a license to Mylan to manufacture and sell pretomanid as part of certain regimens in high-income countries as well as a non-exclusive license for sales in low-income and middle-income countries hardest hit by TB.
Pretomanid is a novel drug that works specifically against M. tuberculosis and appears to be able to kill both actively replicating cells and stealthy dormant ones. Molecular studies have suggested that pretomanid has a complex killing method, potentially busting the bacteria’s cell walls while also poisoning the germs by the release of nitric oxide.
Unfortunately, the drug only has these destructive effects on Mycobacterium, not other types of bacteria. M. tuberculosis and its relatives are a bit of an odd-ball group. They have a unique outer structure that makes them both difficult to characterize and difficult to kill.
Bright barriers
Most bacteria can be easily divided into one of two main groups based on how their cell walls are structured, which in turn can be determined by how the cells take up certain dyes. Generally, bacteria are sorted using a basic dye test designed by Danish physician Hans Christian Gram in 1884, called Gram staining.
In the staining, bacteria with a thick, homogenous cell wall primarily made of the polymer peptidoglycan will appear purple, or "Gram positive." That thick layer of peptidoglycan helps hold in a purple dye called crystal violet. By contrast, cells with more complex cell walls consisting of a relatively thin layer of peptidoglycan plus an outer membrane don’t hold in crystal violet as well. Instead, these can be counter-stained to be a contrasting pink color—"Gram negative."
The simple test sorts out common bacteria. E. coli is Gram-negative, for instance, while Staph. aureus is Gram-positive. The cell wall structure suggested by the Gram staining can also be helpful in determining which types of drugs will work against a given bacteria. After all, to kill a germ, a drug generally has to make it past the defensive cell wall somehow.
But none of this applies to Mycobacterium. The genus can’t be Gram stained. Instead of a cell-wall structure identified as Gram-negative or positive, M. tuberculosis and its relatives have a unique thick, waxy cell wall, rich in mycolic acid.
Small victory in a huge war
Pretomanid appears to mess with the synthesis of mycolic acid, according to a study that looked at gene activity while M. tuberculosis was in the throes of death. At the same time, the new antibiotic also seems to act as a “suicide bomb” by releasing nitric oxide that poisons the cell’s respiration. These activities seem to have the overall effect of bursting the cell while turning its insides toxic—a combination that would spell certain death. And even if the bacteria are in a stealth mode, in which it doesn't replicate or work on its wall—something M. tuberculosis sometimes does in human lungs—research found that the nitric oxide poisoning is enough to knock out those pesky sleepers.
Overall, it's good news for TB treatments. In a press release, TB Alliance president and CEO Dr. Mel Spigelman called this week’s FDA approval a “victory for the people suffering from these highly drug-resistant forms of the world’s deadliest infectious disease. The associated novel regimen will hopefully provide a shorter, more easily manageable and highly efficacious treatment for those in need.”
With its inherent specificity for dispatching M. tuberculosis, pretomanid has no effect on other bacteria, whether they're Gram-positive or Gram-negative. It would certainly be helpful if it did. Drug resistance among bacterial pathogens is not limited to TB—it's also reaching a critical level for many plagues. The WHO considers antibiotic resistance in general to be “one of the biggest threats to global health.” In the US alone, at least 2 million people get an antibiotic-resistant infection each year, killing at least 23,000, according to the Centers for Disease Control and Prevention. So far, drug-resistant TB is rare in the States.
Meanwhile, the development of antibiotics has stalled. Coming up with novel and effective antibiotics is challenging work and isn’t appealing to many pharmaceutical companies due to a lack of profit. Antibiotics are relatively cheap drugs, taken for short periods. They just don’t yield the revenue seen with longer-term drugs for chronic conditions, such as blood pressure medications. And with the ever-present threat of resistance, a new antibiotic that took decades to create may have a limited life-span in clinical use.To help incentivize the creation of new antibiotics, last year the FDA set up a program called the Limited Population Pathway for Antibacterial and Antifungal Drugs, or LPAD pathway. The program's goal is to hasten the development and approval of new antibiotics. So far, pretomanid is the second drug to be approved through this route.
FDA Principal Deputy Commissioner Amy Abernethy noted in a statement that “We hope we continue to see more development of antibacterial drugs for treating serious or life-threatening infections.”
reader comments
92