Dyck PJ, Chance P, Lebo RV. Hereditary motor and sensory neuropathies. Dyck PJ, Thomas PK, Griffen JW, et al, eds. Peripheral Neuropathy. 3rd ed. Saunders; 1993. 1094-136.
Dyck PJ, Karnes JL, Lambert EH. Longitudinal study of neuropathic deficits and nerve conduction abnormalities in hereditary motor and sensory neuropathy type 1. Neurology. 1989 Oct. 39(10):1302-8. [QxMD MEDLINE Link].
Burns J, Ryan MM, Ouvrier RA. Evolution of foot and ankle manifestations in children with CMT1A. Muscle Nerve. 2009 Feb. 39(2):158-66. [QxMD MEDLINE Link].
Thomas PK. Overview of Charcot-Marie-Tooth disease type 1A. Ann N Y Acad Sci. 1999 Sep 14. 883:1-5. [QxMD MEDLINE Link].
Birouk N, LeGuern E, Maisonobe T, et al. X-linked Charcot-Marie-Tooth disease with connexin 32 mutations: clinical and electrophysiologic study. Neurology. 1998 Apr. 50(4):1074-82. [QxMD MEDLINE Link].
Elliott JL, Kwon JM, Goodfellow PJ, et al. Hereditary motor and sensory neuropathy IIB: clinical and electrodiagnostic characteristics. Neurology. 1997 Jan. 48(1):23-8. [QxMD MEDLINE Link].
England JD, Garcia CA. Electrophysiological studies in the different genotypes of Charcot- Marie-Tooth disease. Curr Opin Neurol. 1996 Oct. 9(5):338-42. [QxMD MEDLINE Link].
Gutierrez A, England JD, Sumner AJ, et al. Unusual electrophysiological findings in X-linked dominant Charcot-Marie-Tooth disease. Muscle Nerve. 2000 Feb. 23(2):182-8. [QxMD MEDLINE Link].
Lewis RA, Sumner AJ. Electrophysiologic features of inherited demyelinating neuropathies: a reappraisal. Ann N Y Acad Sci. 1999 Sep 14. 883:321-35. [QxMD MEDLINE Link].
Quattrone A, Gambardella A, Bono F, et al. Autosomal recessive hereditary motor and sensory neuropathy with focally folded myelin sheaths: clinical, electrophysiologic, and genetic aspects of a large family. Neurology. 1996 May. 46(5):1318-24. [QxMD MEDLINE Link].
Guillebastre B, Calmels P, Rougier PR. Assessment of appropriate ankle-foot orthoses models for patients with Charcot-Marie-Tooth disease. Am J Phys Med Rehabil. 2011 Aug. 90(8):619-27. [QxMD MEDLINE Link].
Hassel B. Improvement of muscle function in Charcot-Marie-Tooth disease by transcutaneous electric nerve stimulation. Muscle Nerve. 1998 Feb. 21(2):267-8. [QxMD MEDLINE Link].
Holmes JR, Hansen ST Jr. Foot and ankle manifestations of Charcot-Marie-Tooth disease. Foot Ankle. 1993 Oct. 14(8):476-86. [QxMD MEDLINE Link].
Ward CM, Dolan LA, Bennett DL, et al. Long-term results of reconstruction for treatment of a flexible cavovarus foot in Charcot-Marie-Tooth disease. J Bone Joint Surg Am. 2008 Dec. 90(12):2631-42. [QxMD MEDLINE Link]. [Full Text].
Wukich DK, Bowen JR. A long-term study of triple arthrodesis for correction of pes cavovarus in Charcot-Marie-Tooth disease. J Pediatr Orthop. 1989 Jul-Aug. 9(4):433-7. [QxMD MEDLINE Link].
Anderson TJ, Klugmann M, Thomson CE, et al. Distinct phenotypes associated with increasing dosage of the PLP gene: implications for CMT1A due to PMP22 gene duplication. Ann N Y Acad Sci. 1999 Sep 14. 883:234-46. [QxMD MEDLINE Link].
Marrosu MG, Vaccargiu S, Marrosu G, et al. A novel point mutation in the peripheral myelin protein 22 (PMP22) gene associated with Charcot-Marie-Tooth disease type 1A. Neurology. 1997 Feb. 48(2):489-93. [QxMD MEDLINE Link].
Suter U, Nave KA. Transgenic mouse models of CMT1A and HNPP. Ann N Y Acad Sci. 1999 Sep 14. 883:247-53. [QxMD MEDLINE Link].
Duchesne M, Danigo A, Richard L, et al. Skin Biopsy Findings in Patients With CMT1A: Baseline Data From the CLN-PXT3003-01 Study Provide New Insights Into the Pathophysiology of the Disorder. J Neuropathol Exp Neurol. 2018 Apr 1. 77 (4):274-81. [QxMD MEDLINE Link].
Chapon F, Latour P, Diraison P, Schaeffer S, Vandenberghe A. Axonal phenotype of Charcot-Marie-Tooth disease associated with a mutation in the myelin protein zero gene. J Neurol Neurosurg Psychiatry. 1999 Jun. 66(6):779-82. [QxMD MEDLINE Link]. [Full Text].
Shy ME, Jani A, Krajewski K, et al. Phenotypic clustering in MPZ mutations. Brain. 2004 Feb. 127(Pt 2):371-84. [QxMD MEDLINE Link]. [Full Text].
Nicholson GA. The dominantly inherited motor and sensory neuropathies: clinical and molecular advances. Muscle Nerve. 2006 May. 33(5):589-97. [QxMD MEDLINE Link].
Krajewski KM, Lewis RA, Fuerst DR, et al. Neurological dysfunction and axonal degeneration in Charcot-Marie-Tooth disease type 1A. Brain. 2000 Jul. 123 Pt 7:1516-27. [QxMD MEDLINE Link]. [Full Text].
Vance JM. Charcot-Marie-Tooth disease type 2. Ann N Y Acad Sci. 1999 Sep 14. 883:42-6. [QxMD MEDLINE Link].
Marrosu MG, Vaccargiu S, Marrosu G, et al. Charcot-Marie-Tooth disease type 2 associated with mutation of the myelin protein zero gene. Neurology. 1998 May. 50(5):1397-401. [QxMD MEDLINE Link].
Piscosquito G, Saveri P, Magri S, Ciano C, Gandioli C, Morbin M, et al. Screening for SH3TC2 gene mutations in a series of demyelinating recessive Charcot-Marie-Tooth disease (CMT4). J Peripher Nerv Syst. 2016 Sep. 21 (3):142-9. [QxMD MEDLINE Link].
Jerath NU, Mankodi A, Crawford TO, Grunseich C, Baloui H, Nnamdi-Emeratom C, et al. Charcot-Marie-Tooth Disease type 4C: Novel mutations, clinical presentations, and diagnostic challenges. Muscle Nerve. 2018 May. 57 (5):749-755. [QxMD MEDLINE Link].
A service of the U.S. National Library of Medicine. Genetics Home Reference: Your reference to understanding genetics conditions. Charcot-Marie-Tooth disease. Published: February 25, 2014. Available at http://ghr.nlm.nih.gov/condition/charcot-marie-tooth-disease.
Kurihara S, Adachi Y, Wada K, et al. An epidemiological genetic study of Charcot-Marie-Tooth disease in Western Japan. Neuroepidemiology. 2002 Sep-Oct. 21(5):246-50. [QxMD MEDLINE Link].
Morocutti C, Colazza GB, Soldati G, et al. Charcot-Marie-Tooth disease in Molise, a central-southern region of Italy: an epidemiological study. Neuroepidemiology. 2002 Sep-Oct. 21(5):241-5. [QxMD MEDLINE Link].
Braathen GJ. Genetic epidemiology of Charcot-Marie-Tooth disease. Acta Neurol Scand Suppl. 2012. iv-22. [QxMD MEDLINE Link].
Carter GT, Jensen MP, Galer BS, et al. Neuropathic pain in Charcot-Marie-Tooth disease. Arch Phys Med Rehabil. 1998 Dec. 79(12):1560-4. [QxMD MEDLINE Link].
Garcia CA. A clinical review of Charcot-Marie-Tooth. Ann N Y Acad Sci. 1999 Sep 14. 883:69-76. [QxMD MEDLINE Link].
Auer-Grumbach M, Wagner K, Strasser-Fuchs S, et al. Clinical predominance of proximal upper limb weakness in CMT1A syndrome. Muscle Nerve. 2000 Aug. 23(8):1243-9. [QxMD MEDLINE Link].
Pareyson D, Taroni F, Botti S, et al. Cranial nerve involvement in CMT disease type 1 due to early growth response 2 gene mutation. Neurology. 2000 Apr 25. 54(8):1696-8. [QxMD MEDLINE Link].
van Pomeren M, Selles RW, van Ginneken BT, et al. The hypothesis of overwork weakness in Charcot-Marie-Tooth: a critical evaluation. J Rehabil Med. 2009 Jan. 41(1):32-4. [QxMD MEDLINE Link].
Burns J, Bray P, Cross LA, et al. Hand involvement in children with Charcot-Marie-Tooth disease type 1A. Neuromuscul Disord. 2008 Dec. 18(12):970-3. [QxMD MEDLINE Link].
Prada V, Schizzi S, Poggi I, et al. Hand Rehabilitation Treatment for Charcot-Marie-Tooth Disease: An Open Label Pilot Study. J Neurol Neurophysiol. 2018 Jul 30. 9 (4):465. [QxMD MEDLINE Link]. [Full Text].
Pazzaglia C, Vollono C, Ferraro D, Virdis D, Lupi V, Le Pera D. Mechanisms of neuropathic pain in patients with Charcot-Marie-Tooth 1 A: a laser-evoked potential study. Pain. 2010 May. 149(2):379-85. [QxMD MEDLINE Link].
Ribiere C, Bernardin M, Sacconi S, Delmont E, Fournier-Mehouas M, Rauscent H. Pain assessment in Charcot-Marie-Tooth (CMT) disease. Ann Phys Rehabil Med. 2012 Apr. 55(3):160-73. [QxMD MEDLINE Link].
Bjelica B, Peric S, Basta I, et al. Neuropathic pain in patients with Charcot-Marie-Tooth type 1A. Neurol Sci. 2020 Mar. 41 (3):625-30. [QxMD MEDLINE Link].
Tozza S, Bruzzese D, Severi D, et al. The impact of symptoms on daily life as perceived by patients with Charcot-Marie-Tooth type 1A disease. Neurol Sci. 2021 Apr 26. [QxMD MEDLINE Link]. [Full Text].
Kennedy RA, Carroll K, Hepworth G, Paterson KL, Ryan MM, McGinley JL. Falls in paediatric Charcot-Marie-Tooth disease: a 6-month prospective cohort study. Arch Dis Child. 2018 Aug 13. [QxMD MEDLINE Link].
Pipis M, Feely SME, Polke JM, et al. Natural history of Charcot-Marie-Tooth disease type 2A: a large international multicentre study. Brain. 2020 Dec 1. 143 (12):3589-602. [QxMD MEDLINE Link]. [Full Text].
Kousseff BG, Hadro TA, Treiber DL, et al. Charcot-Marie-Tooth disease with sensorineural hearing loss--an autosomal dominant trait. Birth Defects Orig Artic Ser. 1982. 18(3B):223-8. [QxMD MEDLINE Link].
Stojkovic T, Latour P, Vandenberghe A, et al. Sensorineural deafness in X-linked Charcot-Marie-Tooth disease with connexin 32 mutation (R142Q). Neurology. 1999 Mar 23. 52(5):1010-4. [QxMD MEDLINE Link].
Reynaud V, Morel C, Givron P, et al. Walking Speed is Correlated with the Isokinetic Muscular Strength of the Knee in Patients with Charcot-Marie-Tooth Type 1A. Am J Phys Med Rehabil. 2018 Oct 26. [QxMD MEDLINE Link].
Cardoso J, de Baptista CRJA, Sartor CD, et al. Dynamic plantar pressure patterns in children and adolescents with Charcot-Marie-Tooth disease. Gait Posture. 2021 May. 86:112-9. [QxMD MEDLINE Link].
Nelis E, Timmerman V, De Jonghe P, et al. Molecular genetics and biology of inherited peripheral neuropathies: a fast-moving field. Neurogenetics. 1999 Sep. 2(3):137-48. [QxMD MEDLINE Link].
Pareyson D. Charcot-Marie-Tooth disease and related neuropathies: molecular basis for distinction and diagnosis. Muscle Nerve. 1999 Nov. 22(11):1498-509. [QxMD MEDLINE Link].
Bergoffen J, Scherer SS, Wang S, et al. Connexin mutations in X-linked Charcot-Marie-Tooth disease. Science. 1993 Dec 24. 262(5142):2039-42. [QxMD MEDLINE Link].
Bone LJ, Dahl N, Lensch MW, et al. New connexin32 mutations associated with X-linked Charcot-Marie-Tooth disease. Neurology. 1995 Oct. 45(10):1863-6. [QxMD MEDLINE Link].
Lewis RA. The challenge of CMTX and connexin 32 mutations. Muscle Nerve. 2000 Feb. 23(2):147-9. [QxMD MEDLINE Link].
Nicholson SM, Ressot C, Gomes D, et al. Connexin32 in the peripheral nervous system. Functional analysis of mutations associated with X-linked Charcot-Marie-Tooth syndrome and implications for the pathophysiology of the disease. Ann N Y Acad Sci. 1999 Sep 14. 883:168-85. [QxMD MEDLINE Link].
Chance PF. Overview of hereditary neuropathy with liability to pressure palsies. Ann N Y Acad Sci. 1999 Sep 14. 883:14-21. [QxMD MEDLINE Link].
Ionasescu VV, Ionasescu R, Searby C, et al. Dejerine-Sottas disease with de novo dominant point mutation of the PMP22 gene. Neurology. 1995 Sep. 45(9):1766-7. [QxMD MEDLINE Link].
Ben Othmane K, Hentati F, Lennon F, et al. Linkage of a locus (CMT4A) for autosomal recessive Charcot-Marie-Tooth disease to chromosome 8q. Hum Mol Genet. 1993 Oct. 2(10):1625-8. [QxMD MEDLINE Link].
Bolino A, Muglia M, Conforti FL, et al. Charcot-Marie-Tooth type 4B is caused by mutations in the gene encoding myotubularin-related protein-2. Nat Genet. 2000 May. 25(1):17-9. [QxMD MEDLINE Link].
Gambardella A, Bolino A, Muglia M, et al. Genetic heterogeneity in autosomal recessive hereditary motor and sensory neuropathy with focally folded myelin sheaths (CMT4B). Neurology. 1998 Mar. 50(3):799-801. [QxMD MEDLINE Link].
Carter GT, Abresch RT, Fowler WM, et al. Profiles of neuromuscular diseases. Hereditary motor and sensory neuropathy, types I and II. Am J Phys Med Rehabil. 1995 Sep-Oct. 74(5 Suppl):S140-9. [QxMD MEDLINE Link].
Keller MP, Chance PF. Inherited neuropathies: from gene to disease. Brain Pathol. 1999 Apr. 9(2):327-41. [QxMD MEDLINE Link].
Bird TD, Ott J, Giblett ER, et al. Genetic linkage evidence for heterogeneity in Charcot-Marie-Tooth neuropathy (HMSN type I). Ann Neurol. 1983 Dec. 14(6):679-84. [QxMD MEDLINE Link].
Berciano J, Combarros O, Figols J, et al. Hereditary motor and sensory neuropathy type II. Clinicopathological study of a family. Brain. 1986 Oct. 109 ( Pt 5):897-914. [QxMD MEDLINE Link].
Rose KJ, Hiller CE, Mandarakas M, Raymond J, Refshauge K, Burns J. Correlates of functional ankle instability in children and adolescents with Charcot-Marie-Tooth disease. J Foot Ankle Res. 2015. 8:61. [QxMD MEDLINE Link]. [Full Text].
Murphy SM, Laura M, Fawcett K, Pandraud A, Liu YT, Davidson GL. Charcot-Marie-Tooth disease: frequency of genetic subtypes and guidelines for genetic testing. J Neurol Neurosurg Psychiatry. 2012 Jul. 83(7):706-10. [QxMD MEDLINE Link].
Miller LJ, Saporta AS, Sottile SL, Siskind CE, Feely SM, Shy ME. Strategy for genetic testing in Charcot-Marie-disease. Acta Myol. 2011 Oct. 30(2):109-16. [QxMD MEDLINE Link]. [Full Text].
Shaffer LG, Kennedy GM, Spikes AS, et al. Diagnosis of CMT1A duplications and HNPP deletions by interphase FISH: implications for testing in the cytogenetics laboratory. Am J Med Genet. 1997 Mar 31. 69(3):325-31. [QxMD MEDLINE Link].
Nicholson GA. Penetrance of the hereditary motor and sensory neuropathy Ia mutation: assessment by nerve conduction studies. Neurology. 1991 Apr. 41(4):547-52. [QxMD MEDLINE Link].
Hayasaka K, Himoro M, Sato W, et al. Charcot-Marie-Tooth neuropathy type 1B is associated with mutations of the myelin P0 gene. Nat Genet. 1993 Sep. 5(1):31-4. [QxMD MEDLINE Link].
Nicholson G, Nash J. Intermediate nerve conduction velocities define X-linked Charcot-Marie- Tooth neuropathy families. Neurology. 1993 Dec. 43(12):2558-64. [QxMD MEDLINE Link].
Bornemann A, Hansen FJ, Schmalbruch H. Nerve and muscle biopsy in a case of hereditary motor and sensory neuropathy type III with basal lamina onion bulbs. Neuropathol Appl Neurobiol. 1996 Feb. 22(1):77-81. [QxMD MEDLINE Link].
Nonnekes J, Hofstad C, de Greef-Rotteveel A, et al. Management of gait impairments in people with Charcot-Marie-Tooth disease: A treatment algorithm. J Rehabil Med. 2021 May 21. 53 (5):jrm00194. [QxMD MEDLINE Link]. [Full Text].
Njegovan ME, Leonard EI, Joseph FB. Rehabilitation medicine approach to Charcot-Marie-Tooth disease. Clin Podiatr Med Surg. 1997 Jan. 14(1):99-116. [QxMD MEDLINE Link].
Vinci P, Gargiulo P. Poor compliance with ankle-foot-orthoses in Charcot-Marie-Tooth disease. Eur J Phys Rehabil Med. 2008 Mar. 44(1):27-31. [QxMD MEDLINE Link].
Zuccarino R, Anderson KM, Shy ME, Wilken JM. Satisfaction with ankle foot orthoses in individuals with Charcot-Marie-Tooth disease. Muscle Nerve. 2021 Jan. 63 (1):40-5. [QxMD MEDLINE Link]. [Full Text].
Dufek JS, Neumann ES, Hawkins MC, O'Toole B. Functional and dynamic response characteristics of a custom composite ankle foot orthosis for Charcot-Marie-Tooth patients. Gait Posture. 2014 Jan. 39(1):308-13. [QxMD MEDLINE Link].
Guillebastre B, Calmels P, Rougier PR. Assessment of appropriate ankle-foot orthoses models for patients with Charcot-Marie-Tooth disease. Am J Phys Med Rehabil. 2011 Aug. 90(8):619-27. [QxMD MEDLINE Link].
Phillips MF, Robertson Z, Killen B, White B. A pilot study of a crossover trial with randomized use of ankle-foot orthoses for people with Charcot-Marie-tooth disease. Clin Rehabil. 2012 Jun. 26(6):534-44. [QxMD MEDLINE Link].
El Mhandi L, Pichot V, Calmels P, Gautheron V, Roche F, Féasson L. Exercise training improves autonomic profiles in patients with Charcot-Marie-Tooth disease. Muscle Nerve. 2011 Nov. 44(5):732-6. [QxMD MEDLINE Link].
Sman AD, Hackett D, Fiatarone Singh M, Fornusek C, Menezes MP, Burns J. Systematic review of exercise for Charcot-Marie-Tooth disease. J Peripher Nerv Syst. 2015 May 22. [QxMD MEDLINE Link].
Mori L, Signori A, Prada V, et al. Treadmill training in patients affected by Charcot-Marie-Tooth neuropathy: results of a multicenter, prospective, randomized, single-blind, controlled study. Eur J Neurol. 2020 Feb. 27 (2):280-7. [QxMD MEDLINE Link]. [Full Text].
Kamholz J, Menichella D, Jani A, et al. Charcot-Marie-Tooth disease type 1: molecular pathogenesis to gene therapy. Brain. 2000 Feb. 123 ( Pt 2):222-33. [QxMD MEDLINE Link]. [Full Text].
Gess B, Baets J, De Jonghe P, Reilly MM, Pareyson D, Young P. Ascorbic acid for the treatment of Charcot-Marie-Tooth disease. Cochrane Database Syst Rev. 2015 Dec 11. 12:CD011952. [QxMD MEDLINE Link].
Hoff JM, Gilhus NE, Daltveit AK. Pregnancies and deliveries in patients with Charcot-Marie-Tooth disease. Neurology. 2005 Feb 8. 64(3):459-62. [QxMD MEDLINE Link].
Graf WD, Chance PF, Lensch MW, et al. Severe vincristine neuropathy in Charcot-Marie-Tooth disease type 1A. Cancer. 1996 Apr 1. 77(7):1356-62. [QxMD MEDLINE Link].
Kuruvilla G, Perry S, Wilson B, et al. The natural history of vincristine-induced laryngeal paralysis in children. Arch Otolaryngol Head Neck Surg. 2009 Jan. 135(1):101-5. [QxMD MEDLINE Link].
Dyck PJ, Swanson CJ, Low PA, et al. Prednisone-responsive hereditary motor and sensory neuropathy. Mayo Clin Proc. 1982 Apr. 57(4):239-46. [QxMD MEDLINE Link].
Ginsberg L, Malik O, Kenton AR, et al. Coexistent hereditary and inflammatory neuropathy. Brain. 2004 Jan. 127:193-202. [QxMD MEDLINE Link]. [Full Text].
Sahenk Z, Nagaraja HN, McCracken BS, King WM, Freimer ML, Cedarbaum JM, et al. NT-3 promotes nerve regeneration and sensory improvement in CMT1A mouse models and in patients. Neurology. 2005 Sep 13. 65(5):681-9. [QxMD MEDLINE Link].
Pareyson D, Marchesi C. Natural history and treatment of peripheral inherited neuropathies. Adv Exp Med Biol. 2009. 652:207-24. [QxMD MEDLINE Link].
Passage E, Norreel JC, Noack-Fraissignes P, et al. Ascorbic acid treatment corrects the phenotype of a mouse model of Charcot-Marie-Tooth disease. Nat Med. 2004 Apr. 10(4):396-401. [QxMD MEDLINE Link].
Burns J, Ouvrier RA, Yiu EM, Joseph PD, Kornberg AJ, Fahey MC, et al. Ascorbic acid for Charcot-Marie-Tooth disease type 1A in children: a randomised, double-blind, placebo-controlled, safety and efficacy trial. Lancet Neurol. 2009 Jun. 8(6):537-44. [QxMD MEDLINE Link].
Micallef J, Attarian S, Dubourg O, Gonnaud PM, Hogrel JY, Stojkovic T, et al. Effect of ascorbic acid in patients with Charcot-Marie-Tooth disease type 1A: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2009 Dec. 8(12):1103-10. [QxMD MEDLINE Link].
Verhamme C, de Haan RJ, Vermeulen M, Baas F, de Visser M, van Schaik IN. Oral high dose ascorbic acid treatment for one year in young CMT1A patients: a randomised, double-blind, placebo-controlled phase II trial. BMC Med. 2009 Nov 12. 7:70. [QxMD MEDLINE Link]. [Full Text].
Pareyson D, Reilly MM, Schenone A, Fabrizi GM, Cavallaro T, Santoro L, et al. Ascorbic acid in Charcot-Marie-Tooth disease type 1A (CMT-TRIAAL and CMT-TRAUK): a double-blind randomised trial. Lancet Neurol. 2011 Apr. 10(4):320-8. [QxMD MEDLINE Link]. [Full Text].
Meyer zu Horste G, Prukop T, Liebetanz D, Mobius W, Nave KA, Sereda MW. Antiprogesterone therapy uncouples axonal loss from demyelination in a transgenic rat model of CMT1A neuropathy. Ann Neurol. 2007 Jan. 61(1):61-72. [QxMD MEDLINE Link].
Sereda MW, Meyer zu Hörste G, Suter U, Uzma N, Nave KA. Therapeutic administration of progesterone antagonist in a model of Charcot-Marie-Tooth disease (CMT-1A). Nat Med. 2003 Dec. 9(12):1533-7. [QxMD MEDLINE Link].
Shy ME. Charcot-Marie-Tooth disease: an update. Curr Opin Neurol. 2004 Oct. 17(5):579-85. [QxMD MEDLINE Link].
Weimer LH, Podwall D. Medication-induced exacerbation of neuropathy in Charcot Marie Tooth disease. J Neurol Sci. 2006 Mar 15. 242(1-2):47-54. [QxMD MEDLINE Link].
Shy ME, Blake J, Krajewski K, et al. Reliability and validity of the CMT neuropathy score as a measure of disability. Neurology. 2005 Apr 12. 64(7):1209-14. [QxMD MEDLINE Link].
Burns J, Ouvrier R, Estilow T, Shy R, Laurá M, Pallant JF, et al. Validation of the Charcot-Marie-Tooth disease pediatric scale as an outcome measure of disability. Ann Neurol. 2012 May. 71(5):642-52. [QxMD MEDLINE Link]. [Full Text].
Siskind CE, Panchal S, Smith CO, Feely SM, Dalton JC, Schindler AB, et al. A review of genetic counseling for Charcot Marie Tooth disease (CMT). J Genet Couns. 2013 Aug. 22(4):422-36. [QxMD MEDLINE Link].
Ramdharry GM, Pollard AJ, Marsden JF, Reilly MM. Comparing gait performance of people with Charcot-Marie-Tooth disease who do and do not wear ankle foot orthoses. Physiother Res Int. 2012 Dec. 17(4):191-9. [QxMD MEDLINE Link].
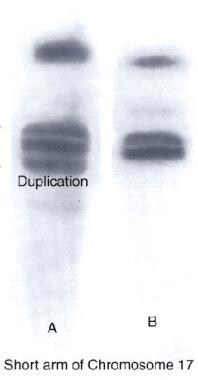
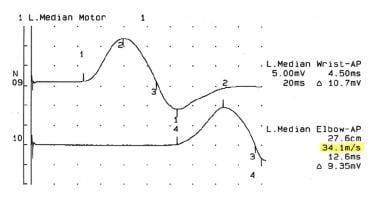
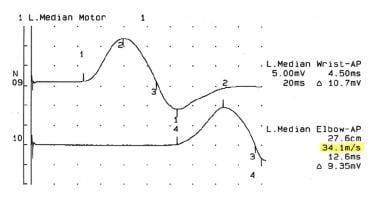 Nerve conduction study showing decreased nerve conduction velocity in the median nerve in an 18-year-old woman with Charcot-Marie-Tooth disease type 1.
Nerve conduction study showing decreased nerve conduction velocity in the median nerve in an 18-year-old woman with Charcot-Marie-Tooth disease type 1.
 Right ulnar motor nerve conduction study in a 29-year-old patient with advanced Charcot-Marie-Tooth disease type 1.
Right ulnar motor nerve conduction study in a 29-year-old patient with advanced Charcot-Marie-Tooth disease type 1.