Early Diagnosis in AS
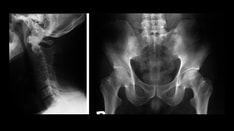
Recently, the Association of Spondyloarthritis International Society (ASAS) has developed more inclusive criteria that allow for the recognition of patients suffering from an axial spondyloarthritis (SpA) at every stage of the disease, even in the presence of normal radiographs. This is because of the inclusion of MRI in addition to x-ray as the imaging tool of choice for the sacroiliac joint (SIJ) and spine. According to these criteria, a patient with low back pain who is younger than 45 years at onset can be classified as having axial SpA if there is imaging evidence of sacroiliitis (either by conventional radiography and/or MRI) plus at least one other clinical feature of SpA. In the absence of sacroiliitis on imaging, the diagnosis can be made if the patient is HLA-B27 and has at least two other clinical SpA features with a sensitivity of 82% and a specificity of 84.4%.[5]
MRI has the capability to identify acute changes, such as those due to active inflammation, and structural changes that reflect an inactive or chronic disease state. Active inflammatory lesions are best visualized by fat-saturated T2-weighted turbo spin-echo sequence or a short tau inversion recovery (STIR) sequence, while chronic lesions are best visualized by T1-weighted turbo spin-echo sequence.
Although the ASAS criteria were initially developed as classification criteria, they are likely to be useful as diagnostic criteria. This may help to prevent diagnostic delay and make an early diagnosis in order to prevent future progression and enable treatment at an early stage. Indeed, there is already published evidence of time to diagnosis and treatment having improved over recent decades. According to Salvadorini et al., the mean of diagnostic delay has been reduced from 12 years in the 1970s to 2 years in the decade from 2000.[6] This improvement in the time to diagnosis is largely owing to the increased use of MRI.
It is well established that the greater the delay in the diagnostic and treatment of the disease, the more likely that radiographic damage would become apparent. The rate of progression from nonradiographic axial spondyloarthritis to AS has been estimated as approximately 10% over 2 years. Poddubnyy et al. found a rate of progression of 11.6% over 2 years;[7] Sampario-Barros et al. reported 24.3% over 5–10 years;[8] and Mau et al. reported 59% after 10 years of follow-up.[9]
"Although the Association of Spondyloarthritis International Society criteria were initially developed as classification criteria, they are likely to be useful as diagnostic criteria."
Early axial ankylosis is seen more frequently in men than in women. The absence of peripheral arthritis or the presence of uveitis, or HLA-B27 positivity is associated with multiple syndesmophytes or fusion of multiple vertebrae of the lumbar spine.[10] In a recent study, the combination of severe MRI sacroiliitis and HLA-B27 positivity was highly predictive of radiographic progression at the SIJ after 8 years. These findings support the concept that MRI is of great utility for the early diagnosis of AS and it also has prognostic value.[11] In another study, the combination of MRI features typical of sacroiliitis in patients with inflammatory back pain who were HLA-B27 positive was shown to have a 90% probability of being diagnosed as axial SpA in patients with well-established symptoms.[12] Oostven et al. investigated 25 HLA-B27 positive patients, with inflammatory back pain and without definite radiographic evidence of sacroiliitis. They assessed the diagnostic value of MRI in the detection of sacroiliitis. The positive-predictive value of ≥grade 2 sacroiliitis on MRI at study entry for the development of ≥grade 2 sacroiliitis on plain radiograph after 3 years was 60%.[13] On the other hand, a longitudinal study investigated MRI, computed tomography and radiographic changes in the SI joints over 1 year in 34 patients with early inflammatory back pain and no correlation between MRI scores and radiographic changes at follow-up was found.[14] This may have been owing to the short follow-up period, as it is expected that 2 years is the minimum time period for radiographic progression to become apparent.[15] Nevertheless, MRI could detect significant inflammatory and destructive changes in the sacroiliac joint over the 1-year follow-up period.
Although the late stage of the disease is the major concern, it is important to note that not all AS patients will progress to spinal fusion and some patients will only develop mild radiographic sacroiliitis. For this reason it is important to identify those patients with the worst prognosis at an early stage. Amor et al. reported seven variables that are correlated with disease severity: hip arthritis; erythrocyte sedimentation rate >30 mm/h; poor efficacy of NSAIDs; limitation of lumbar spine; sausage-like finger or toe; oligoarthritis and onset ≤16 years. If none of these factors are present at diagnosis a mild outcome can be predicted (sensitivity: 92.5%; specificity: 78%). If a hip is involved or if three factors are present, a severe outcome is predictable (sensitivity: 50%) and a mild disease practically excluded (specificity: 97.5%).[16]
"MRI is of great utility for the early diagnosis of ankylosing spondylitis…"
Clinicians and researchers are increasingly focusing on the identification and application of biomarkers for disease activity, prognosis and response to therapy. Several biomarkers have been identified as candidates reflecting disease activity such as the C-reactive protein (CRP), an acute phase reactant that is elevated in approximately 50% of patients with SpA.[17] CRP is regulated by IL-6 and both biomarkers correlate with MRI features of inflammation. Moreover, IL-6 was shown to predict MRI response to anti-TNF-α therapy independently of CRP.[18]
Int J Clin Rheumatol. 2012;7(6):575-578. © 2012 Future Medicine Ltd.