Laboratory Studies
Routine blood analysis and serum chemistries are of limited value, and findings generally are nonspecific.
Serologic testing for rheumatologic disease or vasculitis (eg, antinuclear antibodies, rheumatoid factor, erythrocyte sedimentation rate, C-reactive protein, anticitrulline antibody, antineutrophil cytoplasmic antibodies, antiglomerular basement membrane) may be appropriate in specific cases, as may serum precipitins for common hypersensitivity antigens. ACE testing is not very specific or sensitive but may offer a confirmatory clue to the diagnosis of sarcoidosis.
Imaging Studies
Chest radiography findings are frequently abnormal in patients with fibrotic lung disease. Reticular and/or nodular opacities are the hallmark (see image below).
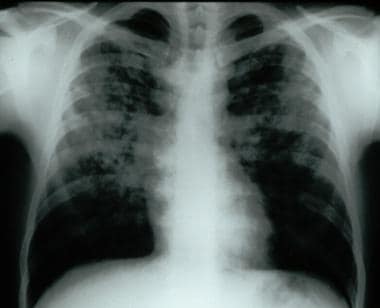 Frontal chest radiograph demonstrating bilateral reticular and nodular interstitial infiltrates with upper zone predominance.
Frontal chest radiograph demonstrating bilateral reticular and nodular interstitial infiltrates with upper zone predominance.
Honeycombing is a late finding and correlates with severe histopathologic findings. [3] Findings may be normal in 10% of patients with histologically proven disease. Therefore, a complete evaluation including pulmonary function testing and, in some cases, pulmonary exercise testing, should be undertaken in all patients clinically suspected to have underlying interstitial lung disease.
Certain patterns and distributions of abnormality seen on chest radiographs are suggestive of particular diseases. Sarcoid-associated interstitial disease often demonstrates symmetric hilar adenopathy. IPF, asbestosis, and connective-tissue disease–related changes are most often basilar and peripheral in distribution. Radiation fibrosis is restricted to the previous radiation port but also may have upper lung zone predominance, as may sarcoidosis, PLCH, HSP, pneumoconioses, and drug-related DPLD due to gold or nitrofurantoin therapy. Some patterns of abnormality, such as reverse congestive heart failure or a bat-wing pattern, are described with eosinophilic pneumonia.
High-resolution chest computed tomography (CT) scanning is more sensitive than chest radiography and may reveal characteristic, if not diagnostic, findings (see image below). [4, 5]
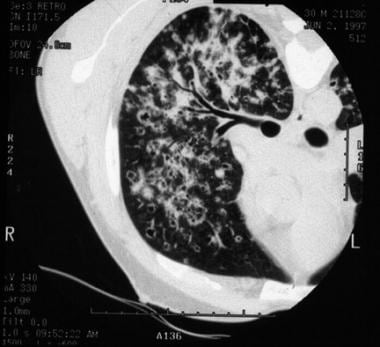 High-resolution chest CT scan of patient with bilateral reticular and nodular interstitial infiltrates with upper zone predominance.
High-resolution chest CT scan of patient with bilateral reticular and nodular interstitial infiltrates with upper zone predominance.
Findings seen on high-resolution chest CT scanning are as follows:
-
Linear reticular opacities are the most common findings.
-
A ground-glass pattern is less common. It is an opacification that does not obscure underlying lung markings and is thought to be a favorable prognostic finding.
-
Airspace consolidation may be present in eosinophilic pneumonia and COP.
-
The presence of nodules suggests HSP, granulomatous disease (eg, sarcoidosis), PLCH, and RBILD.
-
Large cystic spaces may be seen in PLCH and LAM.
-
Honeycombing is indicative of end-stage disease and carries a poor prognosis.
Other Tests
Pulmonary function testing may demonstrate reduced lung volumes with testing of total lung capacity, forced expiratory volume in 1 second, and forced vital capacity. The ratio of forced expiratory volume in 1 second to forced vital capacity is usually normal or increased. Diffusing capacity for carbon monoxide (DLCO) is generally reduced. Static pulmonary compliance is reduced. The restrictive defect may be absent in patients with significant smoking history due to coexistent chronic obstructive pulmonary disease. An obstructive defect may be present in patients with coexistent chronic obstructive pulmonary disease, sarcoidosis, LAM, and eosinophilic granuloma.
Arterial blood gas analysis often reveals an increased alveolar-arterial partial pressure of oxygen gradient and a reduced partial pressure of oxygen. Oxygen desaturation is common. All of these findings may be worsened with exercise.
Pulmonary exercise testing may demonstrate decreased exercise capacity with exercise-limiting impairments in ventilation and gas exchange.
Procedures
Bronchiolar lavage findings are frequently abnormal although generally not diagnostic. Bronchiolar lavage is useful in evaluating the possibility of infection or malignancy. It can also be diagnostic for eosinophilic pneumonia. [6]
Transbronchial and endobronchial lung biopsies may be diagnostic, particularly for sarcoidosis or lymphangitic spread of carcinoma but frequently are not useful for other diagnoses. This is due to the patchy distribution of the majority of these diseases.
Many patients require open or thoracoscopic lung biopsy to establish a definitive diagnosis. Currently, video-assisted thoracoscopic lung biopsy is the preferred method.
The role of lung biopsy in the setting of high-resolution CT scan findings characteristic of specific disease entities remains controversial, with expert opinion weighing in on both sides. [4, 5, 7] Consensus appears to be building on the side of forgoing biopsy when the typical clinical and high-resolution CT scan features of UIP/IPF are present.
Histologic Findings
The histopathology observed in diffuse interstitial diseases of the lung is varied. The histopathologic classification of idiopathic interstitial pneumonias were updated by Katzenstein and Myers [8] in 1998 to include the following 4 subgroups: UIP, AIP (diffuse alveolar damage), DIP/RBILD, and NSIP. Different histopathologic patterns may also be found in biopsy samples from different regions of the lung in these patients, particularly those with NSIP. Sometimes interstitial lung diseases with known etiologies may manifest one of the preceding histopathologic patterns. In addition, other pathologic patterns may be found. These may be consistent with COP, granulomatous lung disease, HSP, giant cell pneumonitis (hard-metal pneumoconiosis), eosinophilic pneumonia, and LIP (lymphoproliferative disorder).
Interpretation of histopathologic findings may be difficult, even in experienced hands, and disagreement may occur even among expert pathologists. [9] In 2005, a 52% rate of disagreement between local general pathologists and "expert" pathologists was documented in a retrospective analysis. [10]
Staging
Pulmonary function studies and the 6-minute walk study have demonstrated prognostic utility in IPF with histopathologic findings of UIP and NSIP. A diminished diffusion capacity (DLCO) on initial evaluation is a poor prognostic indicator, regardless of histologic type. Egan et al [11] have proposed a classification scheme of advanced versus limited disease based on a cutoff value of DLCO greater or less than 40%. Similarly, a trough saturation of less than 88% during a 6-minute walk study has been shown to confer a worse prognosis. Serial decrements in functional vital capacity and DLCO over time are also associated with increased mortality.
-
Frontal chest radiograph demonstrating bilateral reticular and nodular interstitial infiltrates with upper zone predominance.
-
High-resolution chest CT scan of patient with bilateral reticular and nodular interstitial infiltrates with upper zone predominance.




