Using Ultrasound to Measure Carotid Plaque
Measurement of Carotid Plaque Area
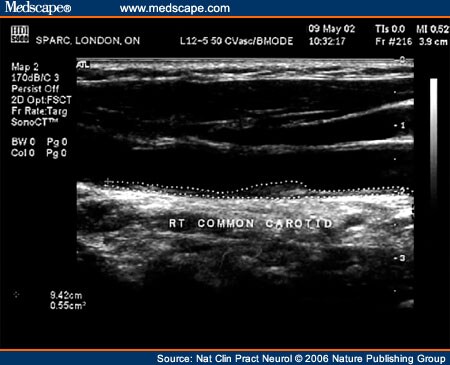
In my laboratory, my colleagues and I initially used ultrasound to evaluate the effects of antihypertensive drugs on blood velocity, in relation to flow disturbances.[11,12] In the mid-1980s, when we acquired duplex carotid ultrasound equipment, we discovered that we could evaluate the extent of atherosclerosis by detecting plaques. For several years, we recorded information on composite drawings of the location and size of plaques, and followed them from year to year to evaluate the effectiveness of therapy in our prevention clinic. Then, in 1990, our outstanding ultrasound technologist, Maria DiCicco, suggested to me that she could measure plaques using software embedded in the ATL® equipment (Advanced Technology Laboratories, Inc., Bothell, WA). We began to measure total plaque area—a representation of atherosclerosis burden—by measuring the cross-sectional area of each plaque in a longitudinal view in which the plaque was biggest, freezing the frame, enlarging the view, and tracing around the plaque perimeter with a cursor on the screen (Figure 1).
Figure 1.
Measurement of carotid plaque area using ultrasound. Each plaque (a local thickening exceeding 1 mm and protruding into the lumen) seen (from the clavicle to the angle of the jaw on both sides) is measured in the longitudinal view. The thickening seen on the near wall would be measured separately, in its own view. The cross-sectional area of the plaque is measured by tracing around the plaque with a cursor; the example in this figure has an area of 0.55 cm2. The total of all plaque areas represents atherosclerosis burden.
We started to use this approach in the management of patients, and to investigate new risk factors for atherosclerosis. In 1997, for example, we reported that the rise in blood pressure during mental stress was a stronger predictor of plaque progression than were any of the traditional risk factors.[13]
Table 1 shows the proportion of patients in my clinic with measurable plaque, divided by age-group. For studies in children and very young people, measurement of plaque is not a viable option, and IMT would be the better approach; above the age of 35, however, most patients will have measurable plaque. At any age, men have greater total plaque area than do women; plaque area progression accelerates after the age of 50 years in both sexes (Figure 2).[14]
Figure 2.
Progression of total plaque area by age and sex.[14] Abbreviation: SE = standard error.
There is some controversy over the definition of plaque. The 2004 IMT consensus conference[15] defined plaque as "a focal structure that encroaches into the arterial lumen of at least 0.5 mm or 50% of the surrounding IMT value or demonstrates a thickness of 1.5 mm as measured from the media-adventitia interface to the intima-lumen interface". In my laboratory, however, we have defined plaque as a localized thickening exceeding 1 mm, and we have been the only group to publish a study relating plaque area to risk of events; I therefore suggest that 1 mm is a more appropriate definition. Furthermore, this definition permits measurement of plaque in a higher proportion of patients. Some might argue that such measurement amounts to measuring IMT, but measuring the area of such lesions, particularly when assessing progression, is much more informative than measuring the thickness alone, because plaque progresses along the carotid artery 2.4 times faster than it thickens,[13] as discussed below.
Measurement of Three-dimensional Carotid Plaque Volume
Beginning in 1994, my group collaborated with Dr Aaron Fenster, leader of the Imaging Research Laboratories at the Robarts Research Institute, on measurement of carotid plaque volume. This procedure involves scanning along the carotid arteries in a cross-sectional view, with equipment that captures ~30 slices per second and stacks them to form a volume in reconstruction (Figure 3). Plaque area is measured in each cross-sectional slice, in slices of 1 mm thickness, to measure plaque volume. Intraobserver reliability is 94%, and interobserver reliability is 93%; accuracy compared with known volumes is 95%.
Figure 3.
Disk segmentation method for measurement of plaque volume. Plaques are outlined in cross-sectional slices, stepping along the artery in 1 mm slices. The upper plaque has had the discs segmented for measurement of plaque volume; the lower plaque has also had contours applied for assessment of surface plaque roughness. Permission obtained from Walter de Gruyter GmbH & Co. KG © Spence JD et al. (2003) Clin Chem Lab Med 41: 1498-1504.
Technical issues, including precise spatial localization of slices, have largely been overcome. The chief difficulty with measurement of plaque volume by the manual disk segmentation method, which requires close attention and precision, is fatigue of the person carrying out the measurements if large numbers of scans are being processed. To overcome this difficulty, Fenster's group is now developing semi-automated methods for plaque segmentation, and also for quantification of surface plaque roughness, a parameter that reflects the amount of ulceration on the plaque surface (A Fenster, personal communication).
Nat Clin Pract Neurol. 2006;12(11):611-619. © 2006 Nature Publishing Group
Cite this: Technology Insight: Ultrasound Measurement of Carotid Plaque—Patient Management, Genetic Research, and Therapy Evaluation - Medscape - Nov 01, 2006.














Comments