A technique described by its creators as “like picking up a pea by placing a drinking straw on it and sucking through the straw” could make it easier to fabricate precise 3D patterns of biological tissues in the laboratory. The approach, dubbed aspiration-assisted bioprinting, could be used for applications such as regenerative medicine, tissue engineering and in vitro modelling of human diseases.
In 3D bioprinting, cell-laden hydrogels or “bioinks” are used to build biological structures layer-by-layer. Recent advances in the field mean that researchers can routinely fabricate patterned tissues and vascular-like networks and perfuse them with living cells and nutrients. The techniques employed vary depending on the viscosity and nature of the bioinks, and include ink-jet printing, microvalve- and extrusion-based bioprinting to name but three.
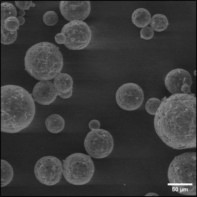
The great hope of 3D bioprinting is that it will enable patient-specific human tissues to be fabricated in the lab – perhaps even using a patient’s own cells. The problem is that current 3D bioprinting techniques cannot accurately position the densely packed aggregates of living cells that act as building blocks for functional human tissues and organs. These aggregates, known as “tissue spheroids”, can also be rendered non-viable if the printing process damages their biological, structural or mechanical properties. A further challenge is that most techniques cannot print spheroids of different sizes, or accommodate the scaffold-like structures that are the starting point for many tissue-engineering applications.
Aspiration-assisted bioprinting
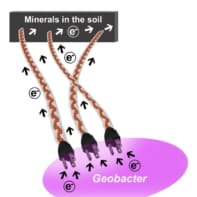
A team of researchers at Pennsylvania State University in the US has now developed a new bioprinting technique that overcomes these difficulties by using suction to pick up and print different types of spheroids. The spheroids they tested were made of human or mouse mesenchymal stem cell aggregates and ranged in size from 80 to 600 microns. To avoid damaging them, the researchers kept the suction force to a minimum value, which they calculated based on the critical lifting pressure needed to overcome the thermodynamic barrier at the interface between the air, the tissue and the cell growth medium.
By holding the suction forces on the spheroids, team leader Ibrahim Ozbolat and colleagues demonstrated that they could move the spheroids to the proper locations before releasing them. They used this technique in conjunction with conventional micro-valve printing to build up tissues.
Collective capillary sprouting
By controlling the exact placement and type of spheroid, the Penn State team created tissues made from different types of cell, such as bone, as well as tissues that consist of a single cell type. This precise control also enabled them to create a matrix of spheroids with capillaries sprouting in specific directions. Since capillaries deliver oxygen and nutrients to cells, and are thus crucial for tissue growth and viability, controlling their spread is an important step towards creating viable tissues.

The past, present and future of 3D bioprinting
As well as bioprinting spheroids, Ozbolat says the team also printed tissue strands and single electrocytes – the modified muscle or nerve cells that generate electricity in fish such as electric eels. The bioprinted electrocytes might be used to fabricate biological batteries for various applications, including pacemakers, cochlear implants and brain chips, he tells Physics World.
The researchers, who report their work in Science Advances, say they are now focusing on improving their system so it can print spheroids at a higher rate, which would allow them to create larger tissue samples faster and with more intricate shapes.