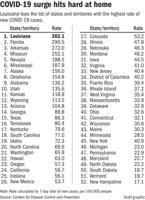
The tsunami of new coronavirus cases washing over Louisiana in a fourth wave of the pandemic has once again left the state with the most severe outbreak in the country.
The delta variant of the disease has found fertile ground in Louisiana, which has among the worst vaccination rates in the U.S., leading to a surge that so far appears on track to outpace any that came before it.
Weekly case counts have exploded to 8 times where they were just last month, going from some of the lowest numbers seen during the 16-month pandemic to among the highest. Hospitalizations have more than tripled over the same period once again putting a strain on health care resources that have already been stretched to the breaking point over the past year and a half.

David Gautreaux receives his dose of the Johnson & Johnson COVID-19 Vaccine from Dushanne Smith LPN, left, as doses were distributed at the Dutchtown Branch of the Ascension Parish Library Friday July 23, 2021, in Dutchtown, La.
More than 300 out of every 100,000 people in Louisiana have tested positive for the coronavirus in just the past week, eclipsing the numbers in other southern states – which are also seeing outbreaks amid low vaccination levels – and pushing the rate five times higher than in states like California, where far greater numbers have received their shots.
The White House has now declared #Louisiana, which has the highest recent case growth per capita nationwide, a “state of concern.” #COVID19 #Delta @SleevesUpLA
— Alyson Neel (@alyson_neel) July 23, 2021
And that might be the greatest tragedy of the latest surge, experts say: while vaccinations might not stop the more transmissible delta variant entirely, they have been shown to significantly reduce the chance of serious illness and death. Just 40.5% of Louisiana’s population has had at least one shot, according to the Centers for Disease Control and Prevention, compared to nearly 64% in California.
“It’s all unnecessary,” said Susan Hassig, an epidemiologist at Tulane University.

The surge has struck dramatically and quickly. The daily average number of new confirmed cases has nearly tripled in just two weeks.
The case counts have now grown to near where they were at the peak of last summer’s wave, which took more than twice as long to build up so much momentum.
The dramatic speed with which the delta variant has overtaken the state is not just limited to new cases. At least some of those cases will be mild or asymptomatic, particularly for those who have been vaccinated, but the number of severe cases is also growing dramatically.
Hospitals first started seeing an uptick in patients with severe respiratory symptoms a week ago.
The number of people hospitalized with the coronavirus in Louisiana has shot up by more than 400 over the past seven days, the largest weekly …
At Our Lady of the Lake Regional Medical Center in Baton Rouge, 30 patients were admitted over a 48-hour period last weekend. The hospital had to turn an entire floor into a COVID ward.
Statewide, patient counts in hospitals grown by double digits nearly every day in July, bringing the total number to 1,008 as of Thursday, the latest count available.
That’s just a little less than half the highest count recorded over the course of the pandemic in early January and there are signs the trend is accelerating. The number of people in hospitals with the coronavirus grew by 445 in just the past week, the largest seven-day increase since the first month of the pandemic.
If more staff contract COVID, miss work, it could imperil infection control and patient care
And hospital officials expect the numbers to keep growing.
“It’s rare to have big numbers then it stops,” said Dr. Catherine O’Neal, an infectious disease specialist at Our Lady of the Lake Regional Medical Center in Baton Rouge. “It usually escalates for a while.”

Dr. Catherine O’Neal, Our Lady of the Lake Chief Medical Officer and infectious disease expert, gives details about the new Delta variant of Covid-19 during a news conference at the State Capitol on July 17, 2021.
Government officials have taken to more urgent warnings that people should get vaccinated as soon as possible and return to wearing masks in public as the case counts have climbed, but largely stopped short of issuing mandates or new restrictions. Gov. John Bel Edwards issued a recommendation that residents wear masks indoors on Friday – shortly after similar recommendations came in New Orleans and Shreveport.
Infection cases have soared since early July, reaching two thirds the height of 2020's second wave
"It pains me to say this, but this surge is on us. How bad it gets, how long it stays bad, how many people ultimately die – on us," Edwards said. "We can do better. It's entirely within our control."
Much remains unknown about how a delta wave will differ from those caused by earlier iterations of the virus and how those differences will play out in an environment where at least some have protection due to the vaccine.
The speed with which delta is spreading could mean it will burn out more quickly as it runs out of new people to infect, leading to a sharp but short spike, Hassig said.

Louisiana Gov. John Bel Edwards
“In places where people are not masking and going out and still going to the bars and all that kind of stuff, living their normal life, the virus is going to burn through those populations pretty quickly because it’s going to be spreading like a proverbial wildfire,” she said.
But, she noted, at least one model is predicting the current surge lasting into the fall, far longer than other waves have been able to sustain their momentum.
As COVID-19 cases surge in Louisiana among unvaccinated people, the inevitable is occurring: some vaccinated people are also getting sick.
The other question is whether high vaccination rates among the elderly, who were the most vulnerable in earlier waves, will blunt the death toll this time. Nearly 60 deaths were attributed to the virus over the last seven days, more than twice as many as a month ago, but still lower than the count that would normally be expected in several weeks as the virus runs its course.
Typically it takes weeks for patients to succumb to the virus after an infection and the current case counts would suggest a staggering number of deaths to come in the next month. But it’s unclear how that pattern will play out in an environment where the most vulnerable, at least, have been vaccinated. More than 83% of residents 70 or older have had at least one shot, potentially reducing the mortality in an age group that has accounted for two-thirds of the state's coronavirus deaths so far.
Health care officials say, however, there are worrying signs that the current strain could have more severe impacts on the young.
The average age of the 313 patients hospitalized with COVID-19 at Ochsner Health’s hospitals is 55. That’s a full decade younger than the cohort of patients hospitalized at Ochsner six months ago in January. In April 2020, it was 69.
Warning of a new coronavirus surge, St. Tammany Parish officials and doctors urged unvaccinated people to get vaccinated, a move that Coroner …
Younger residents are also the least-likely to be vaccinated, with only 26.3% of 18 to 29 year olds having received a shot.
“It’s unbelievable the impact vaccinations might have had in that young population,” O’Neal said.
CORRECTION: Earlier versions of this story misspelled Blake Paterson's name.