Abstract and Introduction
Abstract
Practitioners from around the country who have extensive experience in intrathecal baclofen (ITB) therapy gathered in early 2004 to develop best-practice guidelines for ITB therapy. Discussion focused on the idea that ITB therapy is a program rather than a procedure. Key recommendations were made in areas including team coordination, patient selection and goals, patient education, patient screening, implant technique, long-term management, individualized dosing options, ongoing evaluation of patient response, appraisal of the integrity of the catheter and infusion system, and appropriate practice resources.
Introduction
Intrathecal baclofen (ITB) therapy has been shown to benefit patients with severe spasticity related to spinal cord injury, multiple sclerosis (MS), cerebral palsy (CP), brain injury, and stroke (Albright et al., 2003; Meythaler, Guin-Renfroe, Brunner, & Hadley, 2001; Ordia, Fischer, Adamski, Chagnon, & Spatz, 2002). Possible outcomes vary greatly, based on the underlying neurological level of function, but may include improved ambulation or wheelchair seating, reduced spasticity-related pain, improved sleep, and easier positioning and caregiving (Azouvi et al., 1996; Gianino, York, Paice, & Shott, 1998; Stempien & Tsai, 2000). Documented complications occur in 10%–45% of patients; they may include catheter disconnections, kinks, or wound infections. Acute withdrawal syndrome is also possible but rare. (Campbell et al., 2002; Follet et al., 2003; Rawlins, 2004).
ITB therapy gained U.S. Food and Drug Administration (FDA) approval for managing severe spasticity of spinal origin in 1992 and for severe spasticity of cerebral origin in 1996. Adult and pediatric patients may receive ITB therapy in a variety of settings, including university medical centers, community hospitals, and private practices.
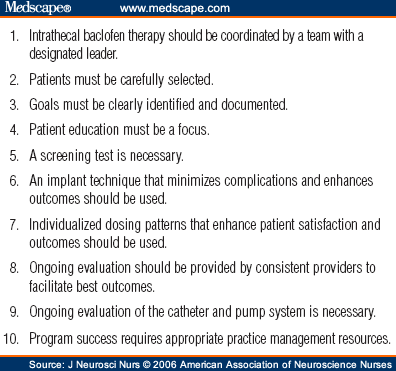
In March 2004, 14 practitioners with experience in ITB therapy met in Minneapolis to develop best-practice guidelines for providers. Participants included physicians from specialties such as neurosurgery, neurology, and physical medicine, as well as four advanced practice nurses from around the country. This article presents the perspective of two of the nurses and summarizes what the authors believe to be the most important recommendations from the meeting, with particular emphasis on nursing implications (Fig 1). The goal of this article is to offer practical considerations for clinicians based on the discussions at the forum and the professional experiences of the authors. The forum took place a few months before the release of a new pump model, the SynchroMed II ®; references to use of the new model reflect the opinions of the authors, not those of the forum as a whole.
Figure 1.
Top 10 recommendations for an intrathecal baclofen therapy program
J Neurosci Nurs. 2006;38(2):72-82. © 2006 American Association of Neuroscience Nurses
Cite this: Intrathecal Baclofen Therapy: Ten Steps Toward Best Practice - Medscape - Apr 01, 2006.





Comments