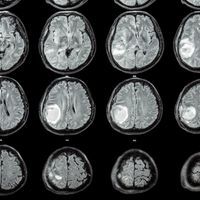
ABOVE: © ISTOCK.COM, STOCKDEVIL
An inducible, tumor-localized gene therapy has been tested for the first time in glioblastoma patients. The two-part approach, which involves receiving an injection of an immune-activator gene into the brain tumor site and swallowing a pill that switches on the gene, resulted in the production of the activator—interleukin 12 (IL-12)—and an infiltration of immune cells into tumor tissue, according to a report in Science Translational Medicine today (August 14). The results also hint that patients’ survival may be prolonged by the treatment.
“All the recent evidence suggests that if you can really get the immune system to attack a tumor, then you have increased potential to cure that tumor, and this [work] is moving in that direction,” says neurosurgeon Frederick Lang of the University of Texas MD Anderson Cancer Center in Houston who was not involved with the project. “I think that makes it exciting.”...
Glioblastoma is an aggressive and deadly form of brain cancer with an average survival after diagnosis of just six to nine months. Even with standard treatment (surgery to remove all or part of the tumor followed by six weeks of chemoradiation), “within an average of seven months . . . the tumor comes back,” says neurosurgeon Antonio Chiocca of Harvard Medical School who led the study.
A number of factors make glioblastoma such a formidable affliction. For one, the blood-brain barrier prevents a number of chemotherapeutics from reaching the tumor. The cancer itself is highly heterogeneous such that even if a drug is effective against certain cells others may grow to take their place. Furthermore, glioblastomas are notoriously “immunologically cold,” says Chiocca, meaning they create an immunosuppressive environment that limits the infiltration of tumor-fighting immune cells.
“Turning [such] a cold tumor into a hot tumor is one of the strategies” for novel treatment approaches, says Lang.
See “The Next Frontier of CAR T Cell Therapy: Solid Tumors”
To do so in glioblastoma patients, researchers have administered IL-12 protein—described by Chiocca as a “powerful master regulator of the immune system.” But systemic IL-12 treatment can be toxic, causing flu-like symptoms or, in more serious cases, an inflammatory response known as cytokine release syndrome that, if not rectified, can lead to organ failure.
To maximize local levels of IL-12 yet prevent dangerously high systemic levels, Chiocca’s team has used an adenovirus vector encoding the IL-12 gene and injected it directly into tumor sites. To control IL-12 dosage, the gene’s transcription is activated only in response to the drug veledimex. “If the patient stops taking the drug, the gene gets shut off again,” explains Chiocca. Drug and vector are both the property of Ziopharm Oncology Inc, which cofunded the trial with the National Institutes of Health.
Veledimex had been shown to cross the blood-brain barrier, drive vector IL-12 expression, and shrink tumors in mice with glioblastoma. So Chiocca and colleagues tested the approach in 31 patients undergoing repeat surgery to remove regrown tumor tissue.
During surgery, the patients were given injections of the vector into tissue surrounding the removed tumor. They then took varying daily doses (10, 20, 30, and 40 mg) of veledimex for up to two weeks. The blood levels of IL-12 and interferon g—a cytokine produced in response to IL-12—were measured before, during, and after the course of veledimex and were shown to rise with treatment and fall after cessation, with levels of the proteins correlating largely with dose. In tumor tissue removed from five patients who needed further surgery, the investigators saw more immune cells infiltrating the area compared with previously removed tumor tissue. The IL-12, interferon, and immune cell infiltration data all suggest the approach is indeed switching on the gene and ramping up immunity, says Lang.
Approximately half of the patients experienced cytokine release syndrome as a result of the therapy and so ceased treatment. Based on the frequency and severity of this complication, together with the patients’ drug-taking compliance and survival data, the authors determined the optimum dose of veledimex to be 20 mg. Patients in this group survived on average 12.7 months after surgery, with 26.7 percent and 13.3 percent surviving to 18 months and 24 months, respectively.
“We don’t get too excited about Phase 1 survival data,” says neurosurgeon Mitchel Berger of the University of California, San Francisco, who was not involved in the trial. Although, he adds, “when you consider the fact that recurrent glioblastoma is a deadly disease that usually has one or two percent of patients alive at two [years] . . . to have a median overall survival of twelve months and somewhere a little bit over ten percent of patients alive at twenty-four months is pretty darn good. It’s very encouraging.”
“It sets a strong foundation for moving forward [with larger trials],” says Lang.
E.A. Chiocca et al., “Regulatable interleukin-12 gene therapy in patients with recurrent high-grade glioma: Results of a phase 1 trial,” Sci Transl Med, 11:eaaw5680, 2019.
Ruth Williams is a freelance journalist based in Connecticut. Email her at ruth@wordsbyruth.com or find her on Twitter @rooph.
Interested in reading more?