Japan: Real-Time Tumor Tracking & Quality Assurance with 3D Printed Phantoms & Moving Robotic Platform
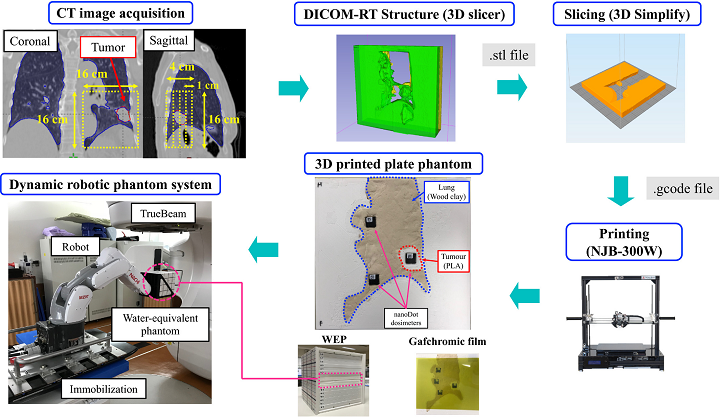
Researchers from Yamaguchi University in Japan enrolled three lung cancer patients in a study about their work assessing a dynamic moving phantom system that can reproduce patient anatomy and 3D tumor motion, in addition to using a tumor‐tracking system to perform patient-specific quality assurance of respiratory-gated radiotherapy. They reported on their results in “A novel dynamic robotic moving phantom system for patient-specific quality assurance in real-time tumor-tracking radiotherapy.”
When it comes to using stereotactic body radiation therapy (SBRT) for cancer treatment, the motion of a tumor located in the abdominal or thoracic regions during respiration can cause problems in accurate dose delivery. You need large internal margins, or IMs, to cover the changes in geometry that happen during free breathing, but this fix causes a different issue – toxicity to healthy tissues. The focus of this study is a novel system for managing respiration-caused tumor motion, made by combining Varian’s TrueBeam radiotherapy system with real‐time tracking radiotherapy (RTRT) system SyncTraX.
“This study was conducted with the objective of assessing a developed novel dynamic moving phantom system that can reproduce patient 3D tumor motion and patient anatomy, and performing patient‐specific QA of respiratory‐gated radiotherapy using SyncTraX,” the team wrote.
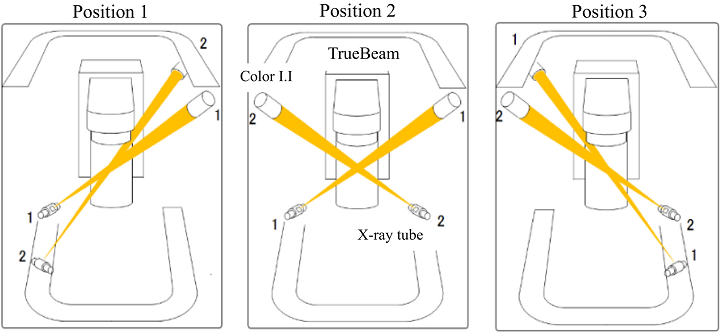
Positions of X‐ray tubes and color I.I.s can be selected from three options. The fiducial markers could be observed using fluoroscopy during radiation treatment with noncoplanar beams. This figure is based on the graphic user interface of SyncTraX.
You need an interaction between the internal tumor motion and external markers or sensors to use motion management strategies, like tumor tracking radiotherapy, breath-holding, and respiratory‐gated radiotherapy. The SyncTraX system can reduce IMs by using an internal fiducial marker for respiratory gating, while X-ray tubes and two color image intensifiers (I.I.s) help calculate the 3D coordinates of fiducial markers near a tumor in the TrueBeam system.
“In a preliminary study, our group reported that this system can track the motion of a fiducial marker and control radiation delivery with reasonable accuracy,” they stated.
When this study was performed in 2015, the researchers said that a SyncTraX log file and an electronic portal image device were able to verify the “geometric and positional accuracy” in the treatment, but weren’t able to “confirm the dose region that may be susceptible to radiation toxicity for the organ at risk.4 Moreover, patient‐specific quality assurance (QA) before treatment was not established.”
Meanwhile, “patient-specific dosimetric QA for respiratory‐gated radiotherapy” has been achieved, but commercially moving tumor phantoms are unable to reproduce the 3D respiratory motion that a complex moving phantom can – important because the moving surrogate, or phantom, causes the radiation beam-on trigger signal.
“Recently, 3D printing technology has opened the possibility of customization of a wide variety of applications in the medical field,” the team noted. “It is capable of producing individualized lung‐mimicking phantoms and is therefore potentially useful for investigating the accuracy of respiratory‐gated radiotherapy using SyncTraX.”
The three patients in this study “underwent respiratory‐gated SBRT with SyncTraX for a lung tumor,” and in each patient, a few fiducial markers with a 1.5 mm diameter were implanted near their tumors. A Siemens CT scanner was used to scan their lungs while they held their breath for about 15 seconds, and an “anisotropic analytical algorithm” was used to perform dose calculation.
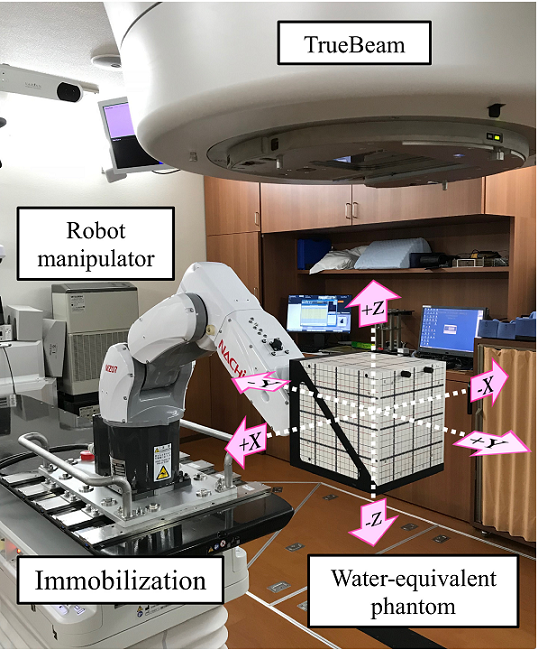
Novel dynamic robotic moving phantom and experimental setup. The robot manipulator was immobilized on the treatment couch. The posture of the manipulator was designated. The WEP was set at the tip of the robotic arm. The three axes of motion are along the left‐right (LR, X), superior–inferior (SI, Y), and anterior–posterior (AP, Z) directions.
A 6-axis robotic moving platform was used to make the 3D respiratory motion, and a 6.1 kg water-equivalent phantom (WEP) “with the 3D‐printed plate lung phantom was set at the tip of the robotic arm.” CT images were used to design four plate lung phantoms and the internal surrogate, which was a fiducial marker. The patient-specific phantoms were 3D printed out of PLA on an FDM 3D printer, and filled with wood clay. The individualized phantoms were designed so an optically simulated luminescence (OSL) dosimeter could be placed inside the lung region, and the four 3D printed ones were inserted into the WEP.
The robotic moving phantom system was used to reproduce 3D respiratory motion of the lung tumor, which was first measured with SyncTraX before treatment. The fiducial marker’s 3D coordinates were recorded at 30 Hz, and then logged.
“The log file that recorded the 3D positions of the lung tumor was used as the input to the dynamic robotic moving phantom,” the researchers explained.
“The command values for driving each joint were sent from the robot controller to the dynamic robotic moving phantom. Then, the dynamic robotic moving phantom reproduced the 3D respiratory motion of the lung tumor.”
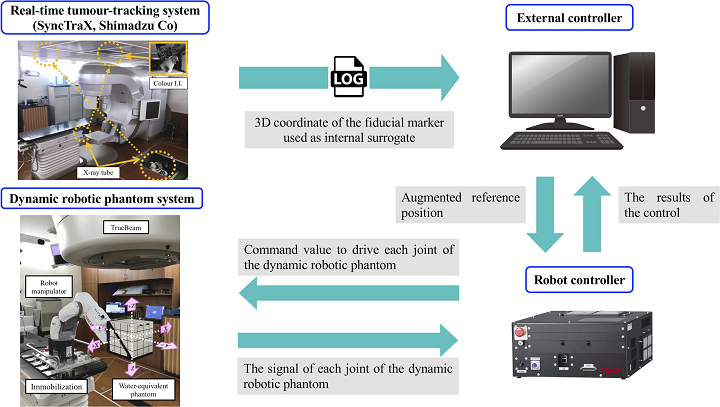
Schematic showing how 3D respiratory motion is reproduced using the dynamic robotic moving phantom system.
The driving signals of each of the robotic moving phantom’s joints were sent to the robot controller. The signals in the joint coordinate system were then transferred into the treatment room’s system through “forward kinematics calculation,” and recorded in a log file. The researchers used TPS to measure the mass density, volume, and Hounsfield unit (HU) of both the tumor and the lung of the 3D printed phantom, then compared the data with the patient’s actual CT images, in order to determine anatomic accuracy.
“The volumes of the 3D‐printed tumor were consistent with those of the patient CT images,” the team wrote.
“Small differences were observed in the HU and mass density of the 3D‐printed tumor.
“The HU and mass density of the 3D‐printed lung were nearly consistent with those of the patient CT images. The 3D printing technology could reproduce the patient anatomy with high accuracy.”

Example of CT images of WEP with 3D‐printed plate lung phantom inserted in the coronal, axial, and sagittal planes for Patient 1.
To determine patient-specific QA, respiratory-gated SyncTraX radiotherapy was sent to the robotic phantom that made the 3D respiratory motion, and specific conditions were set so that the team could recognize the marker in the WEP.
“The WEP was driven to track 3D respiratory motion. Respiratory‐gated radiotherapy was performed for driving the WEP,” the team wrote.
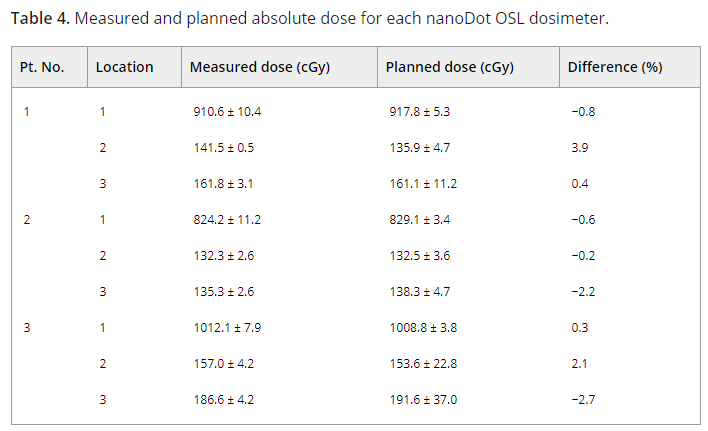
NanoDot OSL dosimeters and Gafchromic film were used to measure the absolute dose and dose distribution to find the dosimetric QA, and the measured dose was compared with the TPS-calculated planned dose. Finally, the driving phantom’s dose distributions were measured “without respiratory‐gated radiotherapy to evaluate the efficiency of motion management.”
“The differences between the planned and measured absolute doses were <1.0% at the isocenter and <4.0% for the lung region,” they explained. “The gamma pass ratios of γ3 mm/3% and γ2 mm/2% under the conditions of gating and no‐gating were 99.9 ± 0.1% and 90.1 ± 8.5%, and 97.5 ± 0.9% and 68.6 ± 17.8%, respectively, for all the patients. Furthermore, for all the patients, the mean ± SD of the root mean square values of the positional error were 0.11 ± 0.04 mm, 0.33 ± 0.04 mm, and 0.20 ± 0.04 mm in the LR, AP, and SI directions, respectively.”

3D printed plate lung phantom in the isocenter plane, where the numbers denote the individual nanoDot OSL measurements at the numbered locations.
They evaluated the SyncTraX tracking accuracy, compared to “the measured position with the actual position of the fiducial marker used as an internal surrogate,” to determine geometric QA.
“The RMS values in the AP direction were larger than those in the other directions because of gravity on the WEP. However, regardless of the gantry, couch angle, and SyncTraX position, the tracking accuracy of SyncTraX was <0.60 mm in all the directions and the 3D direction. The SyncTraX system could track the fiducial marker with high accuracy,” the team wrote.
Most moving phantoms can only perform 1D or 2D target motion, or have simple shapes without important anatomic details. The team’s dynamic robotic moving phantom is able to accurately reproduce complex 3D respiratory motions, and “cover lung tumor motion of up to 34 mm, 24 mm, and 16 mm in the SI, AP, and LR directions, respectively.”
“Furthermore, our developed system comprises an industrial robot. As industrial robots are mass produced, cost reduction can be expected. Therefore, our developed system will be less expensive than other phantom systems,” they noted.
This research showed that commercially available 3D printing can be used to fabricate a realistic lung plate phantom, with mass densities and tumor volumes very similar to the patients. One important thing to note is that the patient-specific QA was performed in a near-clinical situation, not a true one. But the rest of the data collected shows how “patient‐specific QA of respiratory‐gated radiotherapy using SyncTraX can be performed under realistic conditions using the moving phantom.”
“In the future, we plan to perform respiratory‐gated intensity‐modulated radiotherapy (IMRT) with SyncTraX,” the researchers concluded. “The developed phantom system will be useful for performing patient‐specific QA for respiratory‐gated IMRT. Furthermore, it will be useful for the acceptance, commissioning, and QA of novel motion management technologies, such as CyberKnife,30 kilovoltage intrafraction monitoring, 36, 38 and DMLC tracking 39.”
Discuss this and other 3D printing topics at 3DPrintBoard.com or share your thoughts below.
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
You May Also Like
Precision at the Microscale: UK Researchers Advance Medical Devices with BMF’s 3D Printing Tech
University of Nottingham researchers are using Boston Micro Fabrication‘s (BMF) 3D printing technology to develop medical devices that improve compatibility with human tissue. Funded by a UK grant, this project...
3D Printing Webinar and Event Roundup: April 21, 2024
It’s another busy week of webinars and events, starting with Hannover Messe in Germany and continuing with Metalcasting Congress, Chinaplas, TechBlick’s Innovation Festival, and more. Stratasys continues its advanced training...
3D Printing Webinar and Event Roundup: March 17, 2024
It’s another busy week of webinars and events, including SALMED 2024 and AM Forum in Berlin. Stratasys continues its in-person training and is offering two webinars, ASTM is holding a...
3D Printed Micro Antenna is 15% Smaller and 6X Lighter
Horizon Microtechnologies has achieved success in creating a high-frequency D-Band horn antenna through micro 3D printing. However, this achievement did not rely solely on 3D printing; it involved a combination...